A P P E N D I C I T I S
- 1. APPENDICITIS DR KULWANT SINGH
- 2. Contents Dr Kulwant Singh Definition 1 Pathophysiology 2 Clinical Features 3 Diagnosis 4 Differential Diagnosis 5 Treatment 6
- 3. Incidence Commonest abdominal surgical emergency. One person in six develops appendicitis at some time. It is relatively uncommon in developing rural communities. Dr Kulwant Singh
- 4. Appendicitis Dr Kulwant Singh INFLAMMATION OF APPENDIX IS APPENDICITIS Generally Caused by an obstruction: Faecalith. Lymphoid obstruction, Infection.
- 5. Surgical Anatomy The appendix is attached at the point of convergence of the three taeniae coli of the caecum on its posteromedial wall - The meso-appendix is a peritoneal fold containing fat & appendicular artery - Commonly behind the caecum ( Retrocaecal ) - On psoas muscle at or below pelvic brim ( Pelvic ) - Rarely : Pre-ileal – Post-ileal – Paracaecal - Length less than 1 to greater than 30cm ( most are 6-9 cm in length ) - After age of 60 no lymphoid tissue remains Dr Kulwant Singh
- 6. POSITIONS OF APPENDIX Dr Kulwant Singh
- 7. Surgical Anatomy Dr Kulwant Singh Predisposing factors : 1- Obstructive agents 2- Infective agents Obstructive agents Foreign bodies : animal (e.g. thread worms ,round worms) , vegetables (e.g. seeds , date stones) mineral (faecalith = common cause) submucous lymphoid tissue hyperplasia leads to obstruction
- 8. Causes Dr Kulwant Singh Infective agents : Primary infection leading to lymphoid hyperplasia Secondary infection caused by pressure of an obstructed agent leads to epithelial erosion and bacteria gain access to the wall Both aerobic & anaerobic organisms are involved including ( coliforms , enterococci , bacteroids & other intestinal commensals )
- 9. APPENDICITIS Acute appendicitis is thought to begin with obstruction of the lumen Obstruction can result from food matter, adhesions, or lymphoid hyperplasia Mucosal secretions continue to increase intra luminal pressure PATHOPHYSIOLOGY
- 10. APPENDICITIS Eventually the pressure exceeds capillary perfusion pressure and venous and lymphatic drainage are obstructed. With vascular compromise, epithelial mucosa breaks down and bacterial invasion by bowel flora occurs. PATHOPHYSIOLOGY
- 11. APPENDICITIS Increased pressure also leads to arterial stasis and tissue infarction End result is perforation and spillage of infected appendiceal contents into the peritoneum PATHOPHYSIOLOGY
- 12. APPENDICITIS As inflammation continues, serosa and adjacent structures become inflamed This triggers somatic pain fibers, innervating the peritoneal structures. causing pain in the RLQ PATHOPHYSIOLOGY
- 13. APPENDICITIS The change in stimulation form visceral to somatic pain fibers explains the classic migration of pain in the peri-umbilical area to the RLQ seen with acute appendicitis. PATHOPHYSIOLOGY
- 14. APPENDICITIS Exceptions exist in the classic presentation due to anatomic variability of the appendix Appendix can be retrocecal causing the pain to localize to the right flank In pregnancy, the appendix ca be shifted and patients can present with RUQ pain PATHOPHYSIOLOGY
- 15. ACUTE APPENDCITIS ACUTE APPENDCITIS WITH MASS ACUTE APPENDCITIS WITH PERITONITIS Dr Kulwant Singh TYPE
- 16. Acute appendicitis Dr Kulwant Singh - Organisms enter the wall & lodge in sub mucosa , proliferate , wall becomes red & turgid - Rate of acceleration of inflammation increase in presence of obstruction to lumen of appendix
- 17. Acute appendicitis with mass Dr Kulwant Singh Obstruction + infection lead to distension with pus hence increase intraluminal pressure lead to venous occlusion , oedema , arterial occlusion , gangrene and perforation follows , rapidly localised by defence mechanism (greater omentum & coils of bowel ) . Appendix mass is formed , can undergo suppuration to produce an appendix abscess
- 18. Acute appendicitis with peritonitis Dr Kulwant Singh - Free perforation following obstruction + infection allows infected material to disperse widely in peritoneal cavity lead to intense peritoneal reaction with outpouring of fluid - Serosal surfaces of bowel become injected flaked with clotted lymph
- 19. Clinical Features 1 2 3 Abdominal pain periumblical at first , then to right iliac fossa within a few hours it becomes persistent . Onset is usually sudden , may arise in right iliac fossa and remains there Retrocaecal appendix may cause flank or back pain Pelvic appendix may cause suprapubic pain Anorexia nearly always accompanies appendicitis Vomiting occurs in about 75% of patients (most vomit once or twice )
- 20. Clinical Features 5 4 Most patients give history of constipation before onset of pain , diarrhea in some particularly children 6 Fever Low grade Around 100 degee F Oc. Haematuria Murphy’s Triad Pain Vomiting Fever
- 21. Clinical Features 2 1 Stage of shock pale , sweating & anxious - Elevated pulse rate - Low blood pressure - Temperature is subnormal - Respiration is rapid & shallow - Tenderness in the RIF 3 Appendicitis with peritonitis : three stages Stage of perritoneal reaction Severe local tenderness in the RIF - Rebound tenderness - Board –like rigidity - Marked rectal tenderness RIF Stage of flank peritonitis Abdominal distension Absent bowel sounds Faecal vomitus Dehydration
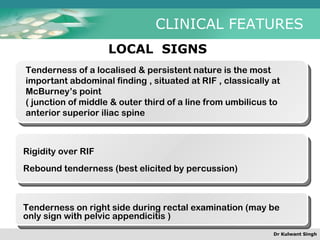
- 22. CLINICAL FEATURES Dr Kulwant Singh LOCAL SIGNS Tenderness of a localised & persistent nature is the most important abdominal finding , situated at RIF , classically at McBurney’s point ( junction of middle & outer third of a line from umbilicus to anterior superior iliac spine Rigidity over RIF Rebound tenderness (best elicited by percussion) Tenderness on right side during rectal examination (may be only sign with pelvic appendicitis )
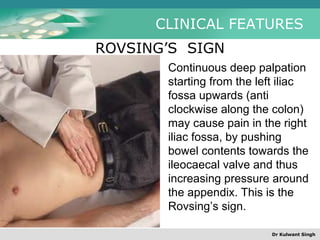
- 23. CLINICAL FEATURES ROVSING’S SIGN Continuous deep palpation starting from the left iliac fossa upwards (anti clockwise along the colon) may cause pain in the right iliac fossa, by pushing bowel contents towards the ileocaecal valve and thus increasing pressure around the appendix. This is the Rovsing’s sign. Dr Kulwant Singh
- 24. CLINICAL FEATURES CAECUM Iliacus muscle Inflamed appendx Psoas muscle caecum Iliacus muscle inflamed appenix Psoas muscle PSOA’S SIGN Psoas sign is right lower-quadrant pain that is produced with the patient extending the hip due to inflammation of the peritoneum overlying the psoas muscles and inflammation of the psoas muscles themselves. Straightening out the leg causes the pain because it stretches the muscles, and flexing the hip into the "fetal position" relieves the pain. Dr Kulwant Singh
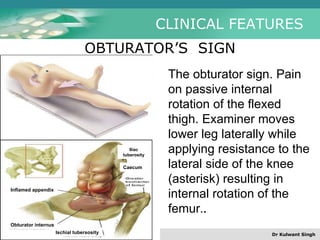
- 25. CLINICAL FEATURES Inflamed appendix Obturator internus Ischial tubersosity Caecum Iliac tuberosity OBTURATOR’S SIGN The obturator sign. Pain on passive internal rotation of the flexed thigh. Examiner moves lower leg laterally while applying resistance to the lateral side of the knee (asterisk) resulting in internal rotation of the femur. . Dr Kulwant Singh
- 26. CLINICAL FEATURES BLOOMBERG’S SIGN Also referred as rebound tenderness . Deep palpation of the viscera over the suspected inflamed appendix followed by sudden release of the pressure causes the severe pain on the site indicating positive Blumberg's sign and peritonitis Dr Kulwant Singh
- 27. CLINICAL FEATURES MCBURNEY’S SIGN To elicit Mcburney’s sign patient should be in supine position with his knees slightly flexed and his abdominal muscles relaxed. Palpate deeply and slowly in the right lower quadrant over McBurney’s point located about 2” from the Rt. Ant. Sup. Iliac Spine. On a line between the spine and umbilicus. Point pain and tenderness is a positive sign and indicates appendicitis. Dr Kulwant Singh
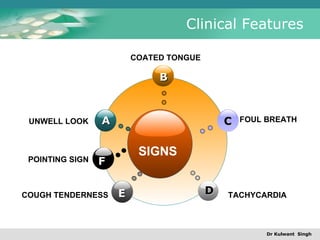
- 28. Clinical Features Dr Kulwant Singh POINTING SIGN SIGNS B E F C D A UNWELL LOOK COATED TONGUE FOUL BREATH COUGH TENDERNESS TACHYCARDIA
- 29. Alvarado Score Dr Kulwant Singh Above 8-9: Sure Below 5: negative 5-8: investigate
- 30. Differential Diagnosis Dr Kulwant Singh Differential Diagnosis Ca Caecum Perforated P.U. Empyema GB Renal Mass Ovarian cyst Fibroid uterus Crohn’s disease Ureteric calculus Ileo caecal TB Liver and GB inflamm. Ileo caecal TB Eterocolitis Pancreatitis Rt Lobar Pneumonia Ectopic gestation Worm Ball Oophoritis
- 31. Dr Kulwant Singh CHILD OLD FEMALE ADULT Differential Diagnosis
- 32. Dr Kulwant Singh Iris Tenax Bell Lycopod Bryonia Homoeopathic Medicines
- 33. Dr Kulwant Singh Echin Bell Lycopod Merc Sol Homoeopathic Medicines
- 34. Dr Kulwant Singh Thank You !