Prolonged labour
Download as PPTX, PDF7 likes7,414 views
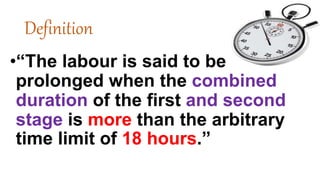
Prolonged labor is the inability of a woman to proceed with childbirth upon going into labor. Prolonged labor typically lasts over 20 hours for first time mothers, and over 14 hours for women that have already had children.
1 of 22
Downloaded 40 times




Recommended
Prolonged labour...



Prolonged labour...Snehlata Parashar
Ėý
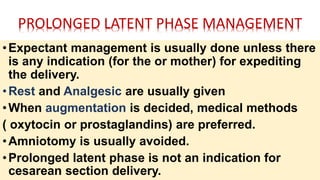
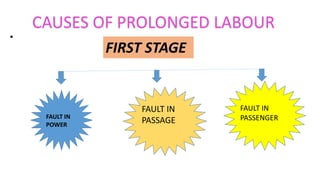
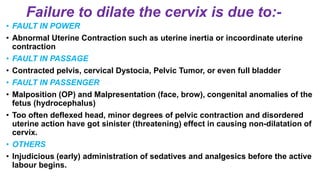
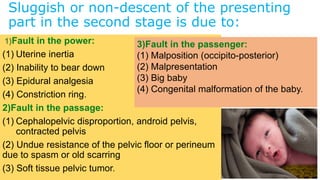
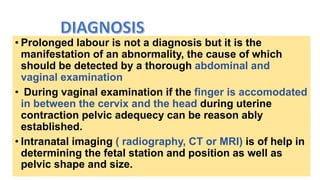
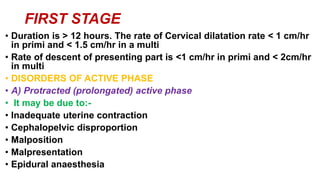
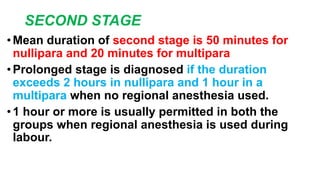
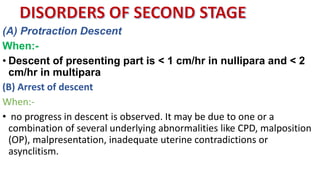
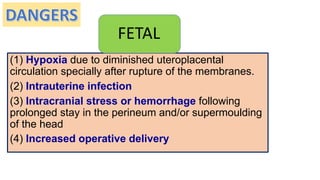
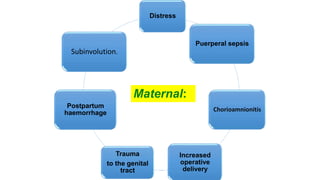
This presentation discusses prolonged labor, which occurs when labor lasts over 20 hours for first-time mothers or 14 hours for women who have given birth before. Prolonged labor can happen in the latent or active phases of the first stage, or the second stage. Causes include problems with uterine contractions, the birth canal, or the baby. Prolonged labor can endanger the baby through hypoxia or infection and endanger the mother through hemorrhage, trauma, or infection. Management involves identifying the cause, monitoring for effects, and treating any issues through techniques like amniotomy, oxytocin infusion, pain relief, or cesarean delivery if needed to deliver the baby safely.Prolonged labour -gihs



Prolonged labour -gihsgangahealth
Ėý
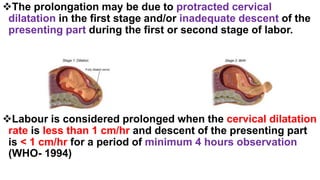
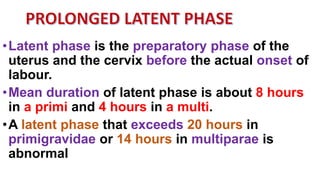
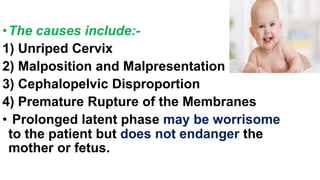
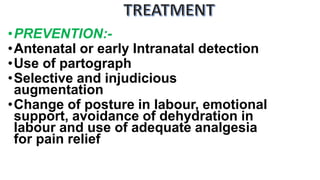
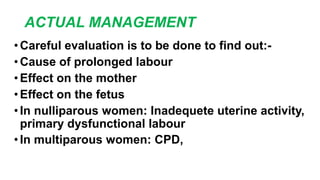
The document defines prolonged labour as when the first and second stages of labour last more than 18 hours total. It then discusses the phases of labour and outlines causes of prolonged labour including issues with uterine contractions, the cervix, pelvis, or baby. Diagnosis involves assessing cervical dilation and descent rates. Dangers to the mother and baby include hypoxia, infection, and trauma. Treatments include preventing issues with early monitoring, changing positions, hydration, and pain relief or interventions like amniotomy, oxytocin, or c-section depending on the stage and severity.Manual removal of placenta



Manual removal of placentajagadeeswari jayaseelan
Ėý
This document describes the procedure for manual removal of the placenta (MRP). MRP is performed when the placenta fails to deliver within 30 minutes of childbirth. It involves inserting fingers into the uterus to locate and detach the placenta from the uterine wall while supporting the fundus. Once detached, the placenta is withdrawn from the uterus while continuing to provide counter-traction. Oxytocin is administered to encourage uterine contraction and prevent hemorrhage. The placenta is examined for completeness and the uterus is checked for contraction to ensure the procedure was successful. Potential complications include shock, postpartum hemorrhage, puerperal sepsis, and inversion or hysterectomy.Precipitate labour



Precipitate labourBRITO MARY
Ėý
Precipitate labor is defined as labor with a combined duration of the first and second stages of less than two hours. It is more common in multiparous women and occurs due to hyperactive uterine contractions and diminished soft tissue resistance, allowing a dilation rate of 5 cm per hour or more. Risks for both mother and baby include lacerations, postpartum hemorrhage, uterine inversion or rupture, intracranial hemorrhage in the baby from rapid delivery without time for molding. Treatment involves hospitalizing women with a history of precipitate labor prior to delivery, suppressing contractions during labor, controlling delivery of the head, liberal episiotomy use, and inducing labor through membrane rupture and controlled deliveryVacuum delivery



Vacuum deliveryDr ABU SURAIH SAKHRI
Ėý
VACUUM DELIVERY - OBSTETRICS AND GYNAECOLOGY-
DEALS WITH THE DELIVERY OF HUMAN BABY BY VACUUM IN SPECIAL OBSTETRIC CONDITIONS.
VACUUM is an instrumental device designed to assist delivery by creating a vacuum between it and the fetal scalp.
Cord prolapse & cord presentation



Cord prolapse & cord presentationJasmi Manu
Ėý
Umbilical cord prolapse is a serious obstetric emergency where the umbilical cord precedes the fetus through the birth canal. It can be diagnosed by feeling the cord or detecting fetal heart abnormalities. Management involves manually lifting the presenting part off the cord, placing the mother in a position to relieve pressure on the cord, considering tocolysis to stop contractions, and delivering via the fastest route, typically an emergency c-section.Disorders of uterine contraction, precipitate labor, premature labor and prol...



Disorders of uterine contraction, precipitate labor, premature labor and prol...VANITASharma19
Ėý
1. Abnormal uterine contractions can cause prolonged and difficult labor and include conditions like uterine inertia with weak contractions, tetanic contractions with strong and frequent contractions, and uterine constriction rings.
2. Precipitate labor is characterized by very rapid labor progressing in less than 3 hours from the start of contractions and can risk maternal and neonatal complications without proper medical care and monitoring.
3. Preterm labor is defined as contractions strong enough to dilate the cervix occurring between 20-37 weeks gestation and can be predicted by fetal fibronectin levels in cervical secretions and ultrasound measurement of cervical length.Prolonged labour



Prolonged labourPriyanka Gohil
Ėý
subject: Obstetrics and Gynaecological Nursing. This topic contains Detail information about prolonged labour and it's managementProlonged labour



Prolonged labourSupriyaMahind
Ėý
Definition , Latent phase,prolonged latent phase , Causes, diagnosis first stage , second stage , treatment first stage ,second stage Cord prolapse



Cord prolapsePriyanka Gohil
Ėý
This topic contains definition, types, etiology, associated factors, diagnosis, management of cord prolapse.Screening of high risk pregnancy



Screening of high risk pregnancySanthosh Antony
Ėý
Screening and assessment of high-risk pregnancies involves identifying women at increased risk of complications through non-invasive tests like ultrasounds, NSTs and CSTs. Diagnostic tests then establish or rule out conditions and include invasive procedures like amniocentesis and cord blood sampling. Ultrasounds provide fetal images and assess growth while NSTs and CSTs monitor the fetal heart rate during rest and contractions. Amniocentesis analyzes amniotic fluid for genetic disorders while cord blood sampling draws fetal blood for similar tests when earlier methods were inconclusive. Both invasive procedures have a risk of miscarriage but can diagnose many conditions affecting the developing baby.Inversion of the uterus



Inversion of the uterusPriyanka Gohil
Ėý
Uterine inversion is a rare complication where the uterus turns inside out, and can be partial or complete. It occurs in around 1 in 20,000 deliveries and is usually acute and complete. There are three degrees - first involves dimpling of the fundus, second passes through the cervix into the vagina, and third is complete outside the vulva. Treatment involves urgent manual replacement or hydrostatic replacement under anesthesia to prevent shock, hemorrhage, infection and other complications. Proper management of the third stage of labor can prevent induced inversions.Uterine rupture



Uterine ruptureDeepa Mishra
Ėý
Uterine Rupture
Deepa Mishra
Assistant Professor (OBG)
Introduction
Uterine rupture is when the muscular wall of the uterus tears during pregnancy or childbirth
Symptoms while classically including increased pain, vaginal bleeding, or a change in contractions are not always present.
Disability or death of the mother or baby may result.
Definition
Uterine rupture is giving way of gravid uterus or dissolution in the continuity of uterine wall anytime after 28 weeks of gestation with or without expulsion of the fetus.
Incidence
Rates of uterine rupture during vaginal birth following one previous C-section, done by the typical technique, are estimated at 0.9%
Rates are greater among those who have had multiple prior C-sections or an atypical type of C-section.
ĖýIn those who do have uterine scarring, the risk during a vaginal birth is about 1 per 12,000
Risk of death of the baby is about 6%
Etiology
Risk Factors
Previous cesarean section
Myomectomy
Dysfunctional labor
Labor augmentation by oxytocin or prostaglandins
High parity
First pregnancy- very rare
Types of uterine rupture
Complete Rupture
All the layers including peritoneum are torn and the uterine contents escape into the peritoneal cavity.
Usually results in death
Incomplete Rupture
Visceral peritoneum is intact and usually the fetus remains in the uterine cavity
Sign & Symptoms
Uterine dehiscence and abdominal pain and vaginal bleeding
Deterioration of fetal heart rate
Loss of fetal station on manual vaginal exam
Hypovolemic shock due to intrabdominal bleeding
Chest pain between the scapulae, pain during inspiration due to irritation of blood below the perineum
Cessation of uterine contractions
Palpation of fetus outside the uterus
Signs of abdominal pregnancy
Post term pregnancy
Diagnosis
Signs of obstructed labor with dehydration, exhaustion, tachycardia raised temperature tonic contraction , pathological retraction ring
Absent fetal heart sound
On PV hot, dry vagina with a large caput over the presenting part
Prevention
Early diagnosis and management of CPD mal presentation and obstructed labor
Proper selection of cases for vaginal delivery
Carefull monitoring of oxytocin infusion specially in multipara
Avoid intra uterine manipulation no version in single fetus
Instrumental delivery after cervical dilatation
Immediate CS in obstructed labor
Hospital delivery for high risk cases
ECV should be avoided during general anaesthesia
Careful manual removal of placenta
Treatment
Resuscitation with adequate hydration and blood transfusion
Laprotomy
Hysterectomy
Repair
Complication
Rupture uterus with haemorrhage, shock and sepsis
Fetal loss is high in spontaneous and traumatic rupture
Mortality is low in LSCS scar rupture
INTRA UTERINE GROWTH RETARDATION



INTRA UTERINE GROWTH RETARDATIONAmrutha Ramakrishnan Nair
Ėý
This document summarizes information about intrauterine growth restriction (IUGR). It discusses normal fetal growth occurring in three stages: hyperplasia, hyperplasia and hypertrophy, and hypertrophy. Causes of IUGR include maternal, fetal, placental, and environmental factors. Maternal causes include medical conditions, malnutrition, smoking, and infections. Fetal causes include genetic abnormalities and infections. Placental causes include improper placentation and reduced blood flow. Clinical features of IUGR infants include a large head, thin skin, and scaphoid abdomen. Risk prediction methods include ultrasound and Doppler. Problems for IUGR infants include hypoxia, hypoglycemia, and immunological and metabolic issues. Management$ Breast engorgement $



$ Breast engorgement $Godwin Pangler
Ėý
This is a topic Breast engorgement which helps in your studies and very precise and understandable. Malposition and malpresentations



Malposition and malpresentationsKushal kumar
Ėý
This document discusses fetal positioning and presentations during labor and delivery. It begins by defining non-vertex presentations including breech, face, brow, transverse, and compound. It then discusses the causes of non-vertex presentations and describes the different positions including occiput posterior. The document provides details on assessing various positions through abdominal and vaginal exams. It concludes by outlining the management of different non-vertex positions, including allowing natural rotation, augmentation of labor, operative vaginal delivery, or caesarean section if needed.Vacuum Delivery



Vacuum Deliverysunil kumar daha
Ėý
Please find the power point on Vacuum delivery. I tried to present it on understandable way and all the contents are reviewed by experts and from very reliable references. Thank youECLAMPSIA



ECLAMPSIASnehlata Parashar
Ėý
This document provides information about eclampsia, including its definition, incidence, types, etiology, risk factors, pathophysiology, clinical features, stages of convulsions, investigations, and management. Eclampsia is a life-threatening complication of pregnancy characterized by hypertension, edema, proteinuria, and convulsions. It is most common in developing countries and rural areas. Risk factors include advanced maternal age, primigravid status, pre-existing hypertension, and family history. Management involves controlling seizures, delivering the baby, providing fluid and magnesium sulfate therapy, and monitoring the patient.Premature labour



Premature labourBalkeej Sidhu
Ėý
Premature labor is defined as labor that begins before 37 weeks of gestation. Approximately 10% of deliveries occur prematurely. While the exact cause is unknown in many cases, risk factors include previous preterm births, infections, chronic illnesses, multiple pregnancies, and short cervical length. Management involves attempts to delay labor with bed rest and tocolytic drugs to allow for corticosteroid administration to improve fetal lung maturity. After delivery, neonatal care focuses on preventing complications like respiratory distress through gentle resuscitation measures.Retained placenta



Retained placentakrishnasagar1910
Ėý
A retained placenta occurs when the placenta is not expelled from the uterus within 30 minutes of childbirth. Risk factors include previous retained placentas, uterine injuries or surgeries, preterm births, induced labor, and multiple pregnancies. Causes can include failure of the placenta to separate fully from the uterine wall or abnormal placenta attachments like placenta accreta. Treatment involves controlled cord traction, manual removal in the operating room if needed, or hysterectomy for deeply embedded placentas. Complications can be life-threatening bleeding, infections, or shock if not properly managed.Abnormal placenta



Abnormal placentaSrujaniDash1
Ėý
Knowledge on variations of abnormal placenta helps you to detect abnormal placenta and take necessary action in clinical settings.Ectopic pregnancy



Ectopic pregnancyOM VERMA
Ėý
An ectopic pregnancy occurs when a fertilized egg implants and grows outside the uterus, usually in one of the fallopian tubes. This is a medical emergency that requires prompt treatment to stop potentially life-threatening bleeding. Most ectopic pregnancies occur in the fallopian tubes. While the incidence of ectopic pregnancy is rising due to increased rates of pelvic inflammatory disease, early diagnosis and treatment have reduced maternal death and illness.............FORCEPS DELIVERY............



............FORCEPS DELIVERY............Rashmi Goswami
Ėý
Forceps are the instrument which are used to extract the fetal head. There are different types of instrument shown in this slide. Indications and contraindications to use this Instrument.Abnormalities of placenta and cord obg



Abnormalities of placenta and cord obgjagan _jaggi
Ėý
Has a velamentous insertion of the cord (the umbilical cord inserts abnormally into the fetal membranes, instead of the center of the placenta) Has placenta previa (a low-lying placenta that covers part or all of the cervix) or certain other placental abnormalities.Physiology and Mangement of 2nd stage labour



Physiology and Mangement of 2nd stage labourjagadeeswari jayaseelan
Ėý
This document discusses the physiology and management of the second stage of labor. It defines the second stage as beginning with full cervical dilation and ending with delivery of the fetus. Key points include: the second stage has two phases - propulsive and expulsive; normal duration is 2 hours for primiparous and 30 minutes for multiparous women; physiological changes include descent, uterine contractions, membrane rupture, and soft tissue displacement; management aims for a normal delivery with minimal maternal effects and early detection of abnormalities. Assessment includes monitoring contractions, descent, fetal heart rate, and progressing through the mechanisms of labor.Iugr



IugrJay Sanap
Ėý
Intrauterine growth restriction (IUGR) refers to poor growth of a baby in the womb. It can be caused by poor maternal nutrition, lack of oxygen to the fetus, or other maternal/placental/fetal factors. IUGR babies are small for their gestational age and classified as symmetrical or asymmetrical. Symmetrical IUGR involves reduced cell number and affects all organs, while asymmetrical IUGR involves cellular hypertrophy and disproportionately affects the body. IUGR increases risks for the baby including hypoglycemia, respiratory issues, and long term health problems. Management depends on severity and includes improving nutrition, bed rest, and timing of delivery.Hyperemesis Gravidarum - Disorder of Pregnancy



Hyperemesis Gravidarum - Disorder of PregnancyJaice Mary Joy
Ėý
Hyperemesis Gravidarum is a severe form of vomiting during pregnancy that can negatively impact a mother's health. It affects 0.3-3% of pregnancies and is the most common cause of hospitalization in the first trimester. Risk factors include young or older age, prior history, and multiple pregnancies. Complications can include dehydration, nutritional deficiencies, and problems for the fetus like growth restriction. Treatment involves hospitalization, IV fluids, electrolyte monitoring, antiemetics, and nutritional supplementation. Nursing care focuses on resolving complications through rehydration and nutrition while addressing emotional concerns.Puerperal sepsis



Puerperal sepsisShaells Joshi
Ėý
This document discusses puerperal infection, which refers to infections occurring after childbirth. It aims to define puerperal infection, describe common causative organisms and risk factors, explain the pathology and diagnostic process, and outline prevention and management strategies. Puerperal infection morbidity affects 2-10% of patients and is higher after cesarean deliveries. Improved obstetric care and antibiotics have reduced rates. The uterus is the most common infection site. Symptoms, treatment with antibiotics and rest, and surgical drainage for abscesses are discussed. Urinary tract infections are another common postpartum complication, caused by bacteria and associated with catheterization and bladder changes. Diagnosis and treatment focus on urinalysisProlonged labour.ppt learn about is risk factors, complications, management



Prolonged labour.ppt learn about is risk factors, complications, managementMallikaNelaturi
Ėý
students learn about management of prolonged laborAbnormal Labour.pptx



Abnormal Labour.pptxMoahmeddahirabdhulla
Ėý
This document discusses prolonged labor, obstructed labor, and dystocia caused by fetal anomalies. Prolonged labor is defined as the combined first and second stage of labor exceeding 18 hours. It can be caused by issues with cervical dilation, fetal descent, uterine contractions, or pelvic and fetal factors. Obstructed labor occurs when descent is arrested due to a mechanical obstruction in the birth canal or fetus. This can lead to exhaustion, dehydration, acidosis, and infection for the mother. Fetal risks include hypoxia, infection, head molding issues, and increased need for operative delivery. Prevention focuses on identifying risk factors. Treatment involves evaluating the cause and deciding between augmentation, assisted delivery, or C-More Related Content
What's hot (20)
Prolonged labour



Prolonged labourSupriyaMahind
Ėý
Definition , Latent phase,prolonged latent phase , Causes, diagnosis first stage , second stage , treatment first stage ,second stage Cord prolapse



Cord prolapsePriyanka Gohil
Ėý
This topic contains definition, types, etiology, associated factors, diagnosis, management of cord prolapse.Screening of high risk pregnancy



Screening of high risk pregnancySanthosh Antony
Ėý
Screening and assessment of high-risk pregnancies involves identifying women at increased risk of complications through non-invasive tests like ultrasounds, NSTs and CSTs. Diagnostic tests then establish or rule out conditions and include invasive procedures like amniocentesis and cord blood sampling. Ultrasounds provide fetal images and assess growth while NSTs and CSTs monitor the fetal heart rate during rest and contractions. Amniocentesis analyzes amniotic fluid for genetic disorders while cord blood sampling draws fetal blood for similar tests when earlier methods were inconclusive. Both invasive procedures have a risk of miscarriage but can diagnose many conditions affecting the developing baby.Inversion of the uterus



Inversion of the uterusPriyanka Gohil
Ėý
Uterine inversion is a rare complication where the uterus turns inside out, and can be partial or complete. It occurs in around 1 in 20,000 deliveries and is usually acute and complete. There are three degrees - first involves dimpling of the fundus, second passes through the cervix into the vagina, and third is complete outside the vulva. Treatment involves urgent manual replacement or hydrostatic replacement under anesthesia to prevent shock, hemorrhage, infection and other complications. Proper management of the third stage of labor can prevent induced inversions.Uterine rupture



Uterine ruptureDeepa Mishra
Ėý
Uterine Rupture
Deepa Mishra
Assistant Professor (OBG)
Introduction
Uterine rupture is when the muscular wall of the uterus tears during pregnancy or childbirth
Symptoms while classically including increased pain, vaginal bleeding, or a change in contractions are not always present.
Disability or death of the mother or baby may result.
Definition
Uterine rupture is giving way of gravid uterus or dissolution in the continuity of uterine wall anytime after 28 weeks of gestation with or without expulsion of the fetus.
Incidence
Rates of uterine rupture during vaginal birth following one previous C-section, done by the typical technique, are estimated at 0.9%
Rates are greater among those who have had multiple prior C-sections or an atypical type of C-section.
ĖýIn those who do have uterine scarring, the risk during a vaginal birth is about 1 per 12,000
Risk of death of the baby is about 6%
Etiology
Risk Factors
Previous cesarean section
Myomectomy
Dysfunctional labor
Labor augmentation by oxytocin or prostaglandins
High parity
First pregnancy- very rare
Types of uterine rupture
Complete Rupture
All the layers including peritoneum are torn and the uterine contents escape into the peritoneal cavity.
Usually results in death
Incomplete Rupture
Visceral peritoneum is intact and usually the fetus remains in the uterine cavity
Sign & Symptoms
Uterine dehiscence and abdominal pain and vaginal bleeding
Deterioration of fetal heart rate
Loss of fetal station on manual vaginal exam
Hypovolemic shock due to intrabdominal bleeding
Chest pain between the scapulae, pain during inspiration due to irritation of blood below the perineum
Cessation of uterine contractions
Palpation of fetus outside the uterus
Signs of abdominal pregnancy
Post term pregnancy
Diagnosis
Signs of obstructed labor with dehydration, exhaustion, tachycardia raised temperature tonic contraction , pathological retraction ring
Absent fetal heart sound
On PV hot, dry vagina with a large caput over the presenting part
Prevention
Early diagnosis and management of CPD mal presentation and obstructed labor
Proper selection of cases for vaginal delivery
Carefull monitoring of oxytocin infusion specially in multipara
Avoid intra uterine manipulation no version in single fetus
Instrumental delivery after cervical dilatation
Immediate CS in obstructed labor
Hospital delivery for high risk cases
ECV should be avoided during general anaesthesia
Careful manual removal of placenta
Treatment
Resuscitation with adequate hydration and blood transfusion
Laprotomy
Hysterectomy
Repair
Complication
Rupture uterus with haemorrhage, shock and sepsis
Fetal loss is high in spontaneous and traumatic rupture
Mortality is low in LSCS scar rupture
INTRA UTERINE GROWTH RETARDATION



INTRA UTERINE GROWTH RETARDATIONAmrutha Ramakrishnan Nair
Ėý
This document summarizes information about intrauterine growth restriction (IUGR). It discusses normal fetal growth occurring in three stages: hyperplasia, hyperplasia and hypertrophy, and hypertrophy. Causes of IUGR include maternal, fetal, placental, and environmental factors. Maternal causes include medical conditions, malnutrition, smoking, and infections. Fetal causes include genetic abnormalities and infections. Placental causes include improper placentation and reduced blood flow. Clinical features of IUGR infants include a large head, thin skin, and scaphoid abdomen. Risk prediction methods include ultrasound and Doppler. Problems for IUGR infants include hypoxia, hypoglycemia, and immunological and metabolic issues. Management$ Breast engorgement $



$ Breast engorgement $Godwin Pangler
Ėý
This is a topic Breast engorgement which helps in your studies and very precise and understandable. Malposition and malpresentations



Malposition and malpresentationsKushal kumar
Ėý
This document discusses fetal positioning and presentations during labor and delivery. It begins by defining non-vertex presentations including breech, face, brow, transverse, and compound. It then discusses the causes of non-vertex presentations and describes the different positions including occiput posterior. The document provides details on assessing various positions through abdominal and vaginal exams. It concludes by outlining the management of different non-vertex positions, including allowing natural rotation, augmentation of labor, operative vaginal delivery, or caesarean section if needed.Vacuum Delivery



Vacuum Deliverysunil kumar daha
Ėý
Please find the power point on Vacuum delivery. I tried to present it on understandable way and all the contents are reviewed by experts and from very reliable references. Thank youECLAMPSIA



ECLAMPSIASnehlata Parashar
Ėý
This document provides information about eclampsia, including its definition, incidence, types, etiology, risk factors, pathophysiology, clinical features, stages of convulsions, investigations, and management. Eclampsia is a life-threatening complication of pregnancy characterized by hypertension, edema, proteinuria, and convulsions. It is most common in developing countries and rural areas. Risk factors include advanced maternal age, primigravid status, pre-existing hypertension, and family history. Management involves controlling seizures, delivering the baby, providing fluid and magnesium sulfate therapy, and monitoring the patient.Premature labour



Premature labourBalkeej Sidhu
Ėý
Premature labor is defined as labor that begins before 37 weeks of gestation. Approximately 10% of deliveries occur prematurely. While the exact cause is unknown in many cases, risk factors include previous preterm births, infections, chronic illnesses, multiple pregnancies, and short cervical length. Management involves attempts to delay labor with bed rest and tocolytic drugs to allow for corticosteroid administration to improve fetal lung maturity. After delivery, neonatal care focuses on preventing complications like respiratory distress through gentle resuscitation measures.Retained placenta



Retained placentakrishnasagar1910
Ėý
A retained placenta occurs when the placenta is not expelled from the uterus within 30 minutes of childbirth. Risk factors include previous retained placentas, uterine injuries or surgeries, preterm births, induced labor, and multiple pregnancies. Causes can include failure of the placenta to separate fully from the uterine wall or abnormal placenta attachments like placenta accreta. Treatment involves controlled cord traction, manual removal in the operating room if needed, or hysterectomy for deeply embedded placentas. Complications can be life-threatening bleeding, infections, or shock if not properly managed.Abnormal placenta



Abnormal placentaSrujaniDash1
Ėý
Knowledge on variations of abnormal placenta helps you to detect abnormal placenta and take necessary action in clinical settings.Ectopic pregnancy



Ectopic pregnancyOM VERMA
Ėý
An ectopic pregnancy occurs when a fertilized egg implants and grows outside the uterus, usually in one of the fallopian tubes. This is a medical emergency that requires prompt treatment to stop potentially life-threatening bleeding. Most ectopic pregnancies occur in the fallopian tubes. While the incidence of ectopic pregnancy is rising due to increased rates of pelvic inflammatory disease, early diagnosis and treatment have reduced maternal death and illness.............FORCEPS DELIVERY............



............FORCEPS DELIVERY............Rashmi Goswami
Ėý
Forceps are the instrument which are used to extract the fetal head. There are different types of instrument shown in this slide. Indications and contraindications to use this Instrument.Abnormalities of placenta and cord obg



Abnormalities of placenta and cord obgjagan _jaggi
Ėý
Has a velamentous insertion of the cord (the umbilical cord inserts abnormally into the fetal membranes, instead of the center of the placenta) Has placenta previa (a low-lying placenta that covers part or all of the cervix) or certain other placental abnormalities.Physiology and Mangement of 2nd stage labour



Physiology and Mangement of 2nd stage labourjagadeeswari jayaseelan
Ėý
This document discusses the physiology and management of the second stage of labor. It defines the second stage as beginning with full cervical dilation and ending with delivery of the fetus. Key points include: the second stage has two phases - propulsive and expulsive; normal duration is 2 hours for primiparous and 30 minutes for multiparous women; physiological changes include descent, uterine contractions, membrane rupture, and soft tissue displacement; management aims for a normal delivery with minimal maternal effects and early detection of abnormalities. Assessment includes monitoring contractions, descent, fetal heart rate, and progressing through the mechanisms of labor.Iugr



IugrJay Sanap
Ėý
Intrauterine growth restriction (IUGR) refers to poor growth of a baby in the womb. It can be caused by poor maternal nutrition, lack of oxygen to the fetus, or other maternal/placental/fetal factors. IUGR babies are small for their gestational age and classified as symmetrical or asymmetrical. Symmetrical IUGR involves reduced cell number and affects all organs, while asymmetrical IUGR involves cellular hypertrophy and disproportionately affects the body. IUGR increases risks for the baby including hypoglycemia, respiratory issues, and long term health problems. Management depends on severity and includes improving nutrition, bed rest, and timing of delivery.Hyperemesis Gravidarum - Disorder of Pregnancy



Hyperemesis Gravidarum - Disorder of PregnancyJaice Mary Joy
Ėý
Hyperemesis Gravidarum is a severe form of vomiting during pregnancy that can negatively impact a mother's health. It affects 0.3-3% of pregnancies and is the most common cause of hospitalization in the first trimester. Risk factors include young or older age, prior history, and multiple pregnancies. Complications can include dehydration, nutritional deficiencies, and problems for the fetus like growth restriction. Treatment involves hospitalization, IV fluids, electrolyte monitoring, antiemetics, and nutritional supplementation. Nursing care focuses on resolving complications through rehydration and nutrition while addressing emotional concerns.Puerperal sepsis



Puerperal sepsisShaells Joshi
Ėý
This document discusses puerperal infection, which refers to infections occurring after childbirth. It aims to define puerperal infection, describe common causative organisms and risk factors, explain the pathology and diagnostic process, and outline prevention and management strategies. Puerperal infection morbidity affects 2-10% of patients and is higher after cesarean deliveries. Improved obstetric care and antibiotics have reduced rates. The uterus is the most common infection site. Symptoms, treatment with antibiotics and rest, and surgical drainage for abscesses are discussed. Urinary tract infections are another common postpartum complication, caused by bacteria and associated with catheterization and bladder changes. Diagnosis and treatment focus on urinalysisSimilar to Prolonged labour (20)
Prolonged labour.ppt learn about is risk factors, complications, management



Prolonged labour.ppt learn about is risk factors, complications, managementMallikaNelaturi
Ėý
students learn about management of prolonged laborAbnormal Labour.pptx



Abnormal Labour.pptxMoahmeddahirabdhulla
Ėý
This document discusses prolonged labor, obstructed labor, and dystocia caused by fetal anomalies. Prolonged labor is defined as the combined first and second stage of labor exceeding 18 hours. It can be caused by issues with cervical dilation, fetal descent, uterine contractions, or pelvic and fetal factors. Obstructed labor occurs when descent is arrested due to a mechanical obstruction in the birth canal or fetus. This can lead to exhaustion, dehydration, acidosis, and infection for the mother. Fetal risks include hypoxia, infection, head molding issues, and increased need for operative delivery. Prevention focuses on identifying risk factors. Treatment involves evaluating the cause and deciding between augmentation, assisted delivery, or C-Prolonged and obstructed labour



Prolonged and obstructed labourSREEVIDYA UMMADISETTI
Ėý
This document describes prolonged and obstructed labor. It defines prolonged labor as when the first and second stages of labor last more than 18 hours total. Obstructed labor occurs when there is poor or no progress despite strong contractions, usually due to issues with the fetus (fault in passenger) or birth canal (fault in passage). Causes include cephalopelvic disproportion, malpositions, big baby, or contracted pelvis. Diagnosis involves assessing cervical dilation rate and fetal descent rate with a partograph. Treatment depends on the stage of labor affected and may include oxytocics, analgesics, assisted delivery, or C-section. Complications can be serious for both mother and baby if not resolved.abnormallabour-130512231046-phpapp02 (2).pptx



abnormallabour-130512231046-phpapp02 (2).pptxMohammad Naik
Ėý
This document discusses abnormal labor and its management. It defines normal labor and describes abnormalities such as dystocia. Abnormal labor can be caused by issues with the cervix, uterus, maternal pelvis, or fetus. Types of abnormal labor include protraction disorders, arrest disorders, and dysfunctional labor. Management depends on the type and stage of abnormality and may include amniotomy, oxytocin administration, operative vaginal delivery, or cesarean section. Close monitoring of labor progress is important to diagnose abnormalities early to guide management.Abnormal labour



Abnormal labourAreesha Khanzada
Ėý
This document discusses abnormal labour, defined as failure to meet defined milestones and time limits for normal labour. It can be caused by issues with uterine contractions (power), the birth canal (passages), or the fetus (passenger). Types of abnormal labour include slow progress/protraction disorders, arrest of progress/arrest disorders, and precipitate labour. Management involves assessing for causes, supporting labour through hydration and pain relief, and potentially augmenting contractions, assisting delivery, or performing a caesarean section if needed for fetal wellbeing. Complications of abnormal labour include increased risk of cesarean, fetal distress, and postpartum hemorrhage.UNCOORDINATED UTERINE ACTION in obstetrics and gynecological



UNCOORDINATED UTERINE ACTION in obstetrics and gynecologicalThangamjayarani
Ėý
I. Prolonged labor is defined as labor lasting longer than 18-24 hours. It can occur when there are issues with uterine contractions (fault in power), the size and shape of the pelvis (fault in passage), or position of the baby (fault in passenger).
II. Precipitate labor is when the first and second stages are less than two hours. It is more common in multiparous women and can be caused by factors like a small baby in a favorable position or strong uterine contractions.
III. Management of prolonged labor involves careful evaluation, correcting dehydration, and definitive treatments like amniotomy, oxytocin infusion, or cesarean section if vaginal delivery isAbnormal+labour



Abnormal+labourRuth Nwokoma
Ėý
This document discusses abnormal labor and its management. It defines normal labor and describes abnormal labor as a difficult labor pattern that deviates from typical progression. Abnormal labor can be caused by issues with the cervix, uterus, maternal pelvis, or fetus. It further outlines the stages of labor and describes factors that can contribute to prolonged latent phase, dysfunctional labor, and dystocia. The management of abnormal labor may include amniotomy, oxytocin administration, operative vaginal delivery, or cesarean section depending on the specific issues present and labor progression. Close monitoring of labor and timely interventions are important to properly manage abnormal labor.prolonged labor.pptx obg seminar 4th year



prolonged labor.pptx obg seminar 4th yearMonikaKosre
Ėý
1) Prolonged labor is defined as labor lasting over 20 hours for first time mothers and over 14 hours for mothers who have previously given birth. It can be caused by issues like malpresentation, cephalopelvic disproportion, or problems with uterine contractions.
2) Signs of prolonged labor include exhaustion, dehydration, high pulse rate, and potential fetal distress. It increases risks for both mother and baby.
3) Management of prolonged labor involves identifying the cause, giving the mother fluids and pain relief, monitoring progress and fetal wellbeing, and potentially assisting delivery or performing a C-section if vaginal delivery is not possible or safe.poor progress of labour



poor progress of labourDR. Kumar Markandu
Ėý
The document discusses poor progress of labor, which is a leading cause of cesarean sections, especially in first-time mothers. It defines the different stages of labor and describes disorders that can cause delayed progress, such as a prolonged latent phase, dysfunctional labor, or secondary arrest. The document provides guidance on assessing labor progress and outlines management strategies, including one-on-one care, hydration, pain relief, mobilization, amniotomy, and oxytocin augmentation when indicated to help improve labor outcomes.Obstructed labor and uterine rupture



Obstructed labor and uterine ruptureAkeFid
Ėý
This document discusses obstructed labor and uterine rupture. It defines obstructed labor as when the fetus cannot progress through the birth canal despite strong contractions due to an insurmountable barrier. Causes include cephalopelvic disproportion and pelvic abnormalities. Uterine rupture is a full thickness tear of the uterus, which can occur in women with prior uterine scars. Risk factors, signs and symptoms, management including emergency surgery, and complications are described for both conditions. Prevention focuses on antenatal care, monitoring labor, and avoiding risky practices like fundal pressure.More from Babitha Mathew (6)
Anemia during pregnancy/types/causes/prevention and management



Anemia during pregnancy/types/causes/prevention and managementBabitha Mathew
Ėý
It's normal to have mild anemia when you are pregnant. But you may have more severe anemia from low iron or vitamin levels or from other reasons. Anemia can leave you feeling tired and weak. If it is severe but goes untreated, it can increase your risk of serious complications like preterm deliveryAdolescent pregnancy



Adolescent pregnancyBabitha Mathew
Ėý
eenage pregnancy, also known as adolescent pregnancy, is pregnancy in a female under the age of 20. Pregnancy can occur with sexual intercourse after the start of ovulation, which can be before the first menstrual period (menarche) but usually occurs after the onset of periods.Abruptio placentae ppt



Abruptio placentae pptBabitha Mathew
Ėý
A serious pregnancy complication in which the placenta detaches from the womb (uterus).
Placental abruption occurs when the placenta detaches from the inner wall of the womb before delivery. The condition can deprive the baby of oxygen and nutrients.
Symptoms include vaginal bleeding, stomach pain and back pain in the last 12 weeks of pregnancy.
Depending on the degree of placental separation and how close the baby is to full-term, treatment may include bed rest or a Caesarean (C-section).Antenatal exercise



Antenatal exerciseBabitha Mathew
Ėý
Antenatal exercises aim at improving the physical and psychological well-being of an expected mother for labor and preventing pregnancy-induced pathologies by various physical means. It generally includes low impact aerobic exercises and stretching exercises.Antenatal care /objectives/history collection abdominal examination



Antenatal care /objectives/history collection abdominal examinationBabitha Mathew
Ėý
Antenatal care is the care you get from healthcare professionals to ensure you have a healthy pregnancy. It includes information on services and support to make choices right for you. Antenatal care will include regular appointments with a midwife, ultrasound scans and screening tests for you and your baby.Antenatal assessment physical well being /introduction and methods



Antenatal assessment physical well being /introduction and methodsBabitha Mathew
Ėý
The tests used to monitor fetal health include fetal movement counts, the nonstress test, biophysical profile, modified biophysical profile, contraction stress test, and Doppler ultrasound exam of the umbilical artery.Recently uploaded (20)
MORPHOLOGICAL FEATURES OF PNEUMONIA.....



MORPHOLOGICAL FEATURES OF PNEUMONIA.....maheenmazhar021
Ėý
This presentation provides a detailed exploration of the morphological and microscopic features of pneumonia, covering its histopathology, classification, and clinical significance. Designed for medical students, pathologists, and healthcare professionals, this lecture differentiates bacterial vs. viral pneumonia, explains lobar, bronchopneumonia, and interstitial pneumonia, and discusses diagnostic imaging patterns.
ðĄ Key Topics Covered:
â
Normal lung histology vs. pneumonia-affected lung
â
Morphological changes in lobar, bronchopneumonia, and interstitial pneumonia
â
Microscopic features: Fibroblastic plugs, alveolar septal thickening, inflammatory cell infiltration
â
Stages of lobar pneumonia: Congestion, Red hepatization, Gray hepatization, Resolution
â
Common causative pathogens (Streptococcus pneumoniae, Klebsiella pneumoniae, Mycoplasma, etc.)
â
Clinical case study with diagnostic approach and differentials
ðŽ Who Should Watch?
This is an essential resource for medical students, pathology trainees, and respiratory health professionals looking to enhance their understanding of pneumoniaâs morphological aspects.MALE REPRODUCTIVE PHYSIOLOGY up load.pptx



MALE REPRODUCTIVE PHYSIOLOGY up load.pptxYIHENEW CHALLIE LIYEW
Ėý
Male animal reproductive physiology including sexual maturity ,reproductive hormone ,sperm production Op-eds and commentaries 101: U-M IHPI Elevating Impact series



Op-eds and commentaries 101: U-M IHPI Elevating Impact seriesKara Gavin
Ėý
A slide set about writing opinion and commentary pieces, created for the University of Michigan Institute for Healthcare Policy and Innovation in Jan. 2025Description of Beta thalassemia its cause and management.



Description of Beta thalassemia its cause and management.KIMS
Ėý
All about Beta Thalassemia etiology , pathology , manifestation and treatment & prevention..physiology 1 T3T4 & Jaundice & capillary circulation ØģØĪاŲ.pptx



physiology 1 T3T4 & Jaundice & capillary circulation ØģØĪاŲ.pptxamralmohammady27
Ėý
ŲŲ ØđŲØŊŲ ŲاØĻ ØŠŲØĻ ØĢŲ ؊اØĻŲØŠ ŲاŲ
power point show
ŲŲŲŲØđŲ ØŽØŊا ŲŲ Ų
ØąØ§ØŽØđØĐ ØģØąŲØđØĐ ŲŲŲØĐ Ø§ŲاŲ
ØŠØاŲ
ŲاŲŲŲ ŲŲØŊØą ŲØđŲ
Ų Øا؎ØĐ ŲØđŲ
ŲŲا
ŲØīŲØąØ§ ŲŲØŊŲØŠŲØąØĐ ŲŲاŲ ØđŲŲ ØŠØŽŲ
ŲØđØĐ ØĢØģØĶŲØĐ Ø§ŲØĻŲŲMLS 208 - UNIT 4 A - Tissue Processing - ETANDO AYUK - SANU 1 - Secured.pdf



MLS 208 - UNIT 4 A - Tissue Processing - ETANDO AYUK - SANU 1 - Secured.pdfEswatini Medical Christian University - EMCU / Southern Nazarene University - SANU
Ėý
The course covers the steps undertaken from tissue collection, reception, fixation,
sectioning, tissue processing and staining. It covers all the general and special
techniques in histo/cytology laboratory. This course will provide the student with the
basic knowledge of the theory and practical aspect in the diagnosis of tumour cells
and non-malignant conditions in body tissues and for cytology focusing on
gynaecological and non-gynaecological samples.Macafem Reviews 2024 - Macafem for Menopause Symptoms



Macafem Reviews 2024 - Macafem for Menopause SymptomsMacafem Supplement
Ėý
At Macafem, we provide 100% natural support for women navigating menopause. For over 20 years, we've helped women manage symptoms, and in 2024, we're proud to share their heartfelt experiences.BIOMECHANICS OF THE MOVEMENT OF THE SHOULDER COMPLEX.pptx



BIOMECHANICS OF THE MOVEMENT OF THE SHOULDER COMPLEX.pptxdrnidhimnd
Ėý
The shoulder complex acts as in coordinated fashion to provide the smoothest and greatest range of motion possible of the upper limb.
Combined motion of GH and ST joint of shoulder complex helps in:
Distribution of motion between other two joints.
Maintenance of glenoid fossa in optimal position.
Maintenance of good length tension
Although some amount of glenohumeral motion may occur while the other shoulder articulations remain stabilized, movement of the humerus more commonly involves some movement at all three shoulder joints.
Acute & Chronic Inflammation, Chemical mediators in Inflammation and Wound he...



Acute & Chronic Inflammation, Chemical mediators in Inflammation and Wound he...Ganapathi Vankudoth
Ėý
A complete information of Inflammation, it includes types of Inflammation, purpose of Inflammation, pathogenesis of acute inflammation, chemical mediators in inflammation, types of chronic inflammation, wound healing and Inflammation in skin repair, phases of wound healing, factors influencing wound healing and types of wound healing.Pharm test bank- 12th lehne pharmacology nursing class



Pharm test bank- 12th lehne pharmacology nursing classkoxoyav221
Ėý
A pediatric nursing course is designed to prepare nursing students to provide specialized care for infants, children, and adolescents. The course integrates developmental, physiological, and psychological aspects of pediatric health and illness, emphasizing family-centered care. Below is a detailed breakdown of what you can expect in a pediatric nursing course:
1. Course Overview
Focuses on growth and development, health promotion, and disease prevention.
Covers common pediatric illnesses and conditions.
Emphasizes family dynamics, cultural competence, and ethical considerations in pediatric care.
Integrates clinical skills, including medication administration, assessment, and communication with children and families.
2. Key Topics Covered
A. Growth and Development
Neonates (0-28 days): Reflexes, feeding patterns, thermoregulation.
Infants (1 month - 1 year): Milestones, immunization schedule, nutrition.
Toddlers (1-3 years): Language development, toilet training, injury prevention.
Preschoolers (3-5 years): Cognitive and social development, school readiness.
School-age children (6-12 years): Psychosocial development, peer relationships.
Adolescents (13-18 years): Puberty, identity formation, risk-taking behaviors.
B. Pediatric Assessment
Head-to-toe assessment in children (differences from adults).
Vital signs (normal ranges vary by age).
Pain assessment using age-appropriate scales (FLACC, Wong-Baker, Numeric).
C. Pediatric Disease Conditions
Respiratory disorders: Asthma, bronchiolitis, pneumonia, cystic fibrosis.
Cardiac conditions: Congenital heart defects, Kawasaki disease.
Neurological disorders: Seizures, meningitis, cerebral palsy.
Gastrointestinal disorders: GERD, pyloric stenosis, intussusception.
Endocrine conditions: Diabetes mellitus type 1, congenital hypothyroidism.
Hematologic disorders: Sickle cell anemia, hemophilia, leukemia.
Infectious diseases: Measles, mumps, rubella, chickenpox.
Mental health concerns: Autism spectrum disorder, ADHD, eating disorders.
D. Pediatric Pharmacology
Medication administration (oral, IV, IM, subcutaneous).
Weight-based dosing calculations (mg/kg).
Common pediatric medications (antibiotics, analgesics, vaccines).
Parenteral nutrition and fluid management.
E. Pediatric Emergency & Critical Care
Pediatric Advanced Life Support (PALS) basics.
Recognizing signs of deterioration (early vs. late signs).
Shock, dehydration, respiratory distress management.
F. Family-Centered Care & Communication
Parental involvement in care decisions.
Therapeutic communication with children at different developmental stages.
Cultural considerations in pediatric care.
G. Ethical and Legal Issues in Pediatric Nursing
Informed consent for minors.
Mandatory reporting of abuse and neglect.
Palliative care and end-of-life considerations in pediatrics.
3. Clinical Component
Hands-on experience in pediatric hospital units, clinics, or community settings.
Performing assessments and interventions under supervision.
Case study discFlag Screening in Physiotherapy Examination.pptx



Flag Screening in Physiotherapy Examination.pptxBALAJI SOMA
Ėý
Flag screening is a crucial part of physiotherapy assessment that helps in identifying medical, psychological, occupational, and social barriers to recovery. Recognizing these flags ensures that physiotherapists make informed decisions, provide holistic care, and refer patients appropriately when necessary. By integrating flag screening into practice, physiotherapists can optimize patient outcomes and prevent chronicity of conditions.Non-Invasive ICP Monitoring for Neurosurgeons



Non-Invasive ICP Monitoring for NeurosurgeonsDhaval Shukla
Ėý
This presentation delves into the latest advancements in non-invasive intracranial pressure (ICP) monitoring techniques, specifically tailored for neurosurgeons. It covers the importance of ICP monitoring in clinical practice, explores various non-invasive methods, and discusses their accuracy, reliability, and clinical applications. Attendees will gain insights into the benefits of non-invasive approaches over traditional invasive methods, including reduced risk of complications and improved patient outcomes. This comprehensive overview is designed to enhance the knowledge and skills of neurosurgeons in managing patients with neurological conditions.
Invasive systems are commonly used for monitoring intracranial pressure (ICP) in traumatic brain injury (TBI) and are considered the gold standard. The availability of invasive ICP monitoring is heterogeneous, and in low- and middle-income settings, these systems are not routinely employed due to high cost or limited accessibility. The aim of this presentation is to develop recommendations to guide monitoring and ICP-driven therapies in TBI using non-invasive ICP (nICP) systems.
Diabetic Ketoacidosis (DKA) & Its Management Protocol



Diabetic Ketoacidosis (DKA) & Its Management ProtocolDr Anik Roy Chowdhury
Ėý
Dr. Anik Roy Chowdhury
MBBS, BCS(Health), DA, MD (Resident)
Department of Anesthesiology, ICU & Pain Medicine
Shaheed Suhrawardy Medical College Hospital (ShSMCH)HUMAN SEXUALITY AND SEXUAL RESPONCE CYCLE



HUMAN SEXUALITY AND SEXUAL RESPONCE CYCLEdaminipatel37
Ėý
It is all about topic of obg for new semester students Renal Physiology - Regulation of GFR and RBF



Renal Physiology - Regulation of GFR and RBFMedicoseAcademics
Ėý
1. Explain the physiological control of glomerular filtration and renal blood flow
2. Describe the humoral and autoregulatory feedback mechanisms that mediate the autoregulation of renal plasma flow and glomerular filtration rate
MLS 208 - UNIT 4 A - Tissue Processing - ETANDO AYUK - SANU 1 - Secured.pdf



MLS 208 - UNIT 4 A - Tissue Processing - ETANDO AYUK - SANU 1 - Secured.pdfEswatini Medical Christian University - EMCU / Southern Nazarene University - SANU
Ėý
Acute & Chronic Inflammation, Chemical mediators in Inflammation and Wound he...



Acute & Chronic Inflammation, Chemical mediators in Inflammation and Wound he...Ganapathi Vankudoth
Ėý









![Abnormal pregnancy and labour 2024 [Autosaved].pdf](https://cdn.slidesharecdn.com/ss_thumbnails/abnormalpregnancyandlabour2024autosaved-250205172802-595407a0-thumbnail.jpg?width=560&fit=bounds)




