Psvt
- 3. Case scenario ÔÇó 71 year old female arrives in ED with palpitations and dizziness. ÔÇó Rhythm strip in your hand but not sure what exactly strip shows????. ÔÇó Do u need to act now? ÔÇó How do you work on whats happening?
- 4. Initial approach ÔÇó Stable or unstable ÔÇó Wide or narrow ÔÇó Regular or irregular
- 5. First things first ÔÇó If unstable ÔÇó And tachyarrythmia is cause of instability ÔÇó Think cardioversion first and diagnosis second
- 6. Narrow complex tachycardias ÔÇ┬┘│ı░ı▓§ÔÇØ
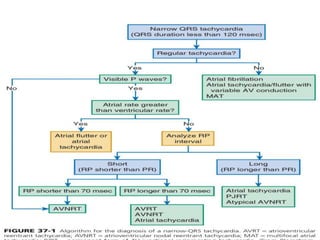
- 7. ´ü▒ NCT - QRS DURATION LESS THAN 120 ms. ´ü▒ In general if QRS is narrow the ventricle is being activated via normal his-purkinjie system thus origin of tachycardia is supraventicular. ´ü▒ SVT with concurrent bundle branch block or intraventricular conduction defect can produce WCT despite supraventricular originÔǪÔǪ.
- 8. NARROW COMPLEX TACHYCARDIAS:SVT ÔÇó REGULAR OR IRREGULAR. ÔÇó ÔÇ£PÔÇØ WAVE OR NO ÔÇ£PÔÇØ WAVE. ÔÇó R-P DISTANCE : LONG OR SHORT
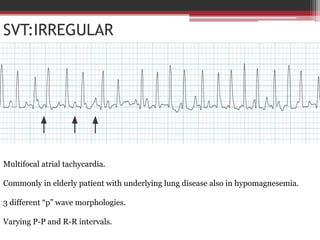
- 10. SVT:IRREGULAR
- 11. SVT:IRREGULAR Irregular undulation of ECG baseline (coarse/medium/fine) Irr.irregular ventricular rhythm
- 12. SVT:IRREGULAR: NO P WAVES:AF ÔÇó Multiple causes including electrolyte disturbanc,structural heart disease, cardiac surgery,ÔÇ£loneÔÇØ. ÔÇó Atrial rhythm rapid,irregular with low amplitude fibrillary waves,no isoelectric period. ÔÇó Usually a reentrant circuit within the atria: ocasionally a single ectopic focus suitable for ablation. ÔÇó Treat the cause : duration known rate control DCCV to convert to sinus rhythm
- 13. SVT:IRREGULAR Multifocal atrial tachycardia. Commonly in elderly patient with underlying lung disease also in hypomagnesemia. 3 different ÔÇ£pÔÇØ wave morphologies. Varying P-P and R-R intervals.
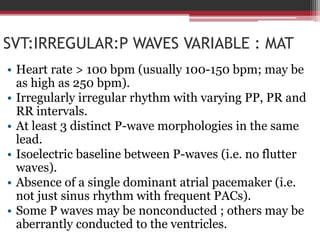
- 14. SVT:IRREGULAR:P WAVES VARIABLE : MAT ÔÇó Heart rate > 100 bpm (usually 100-150 bpm; may be as high as 250 bpm). ÔÇó Irregularly irregular rhythm with varying PP, PR and RR intervals. ÔÇó At least 3 distinct P-wave morphologies in the same lead. ÔÇó Isoelectric baseline between P-waves (i.e. no flutter waves). ÔÇó Absence of a single dominant atrial pacemaker (i.e. not just sinus rhythm with frequent PACs). ÔÇó Some P waves may be nonconducted ; others may be aberrantly conducted to the ventricles.
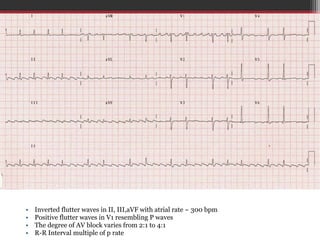
- 15. ÔÇó Inverted flutter waves in II, III,aVF with atrial rate ~ 300 bpm ÔÇó Positive flutter waves in V1 resembling P waves ÔÇó The degree of AV block varies from 2:1 to 4:1 ÔÇó R-R Interval multiple of p rate
- 16. SVT:IRREGULAR:P WAVES:ATRIAL FLUTTER WITH VARIABLE BLOCK ÔÇó P waves at 300bpm or close to ÔÇó Usually d/t re-entry rhythm localised to rt.atrium which generates impulses at rate of 300bpm. ÔÇó The ventricular rate is frequently 150bpm due to 2:1 block with in av node. ÔÇó Ventricular rate may be irregular if the conduction is variable(i.e: if 2:1 alternating with 3:1/4:1). ÔÇó Saw tooth appearance. ÔÇó Narrow negative flutter waves in inferior leads.
- 17. SVT : IRREGULAR: SUMMARY ÔÇó NO P WAVES,NO ISOELECTRIC BASELINE = AF. ÔÇó VARYING P MORPHOLOGY AND P-R,P-P = MAT ÔÇó FLUTTER WAVES SEEN = AFL WITH VARIABLE BLOCK
- 18. NCT ÔÇó NCT can be Ôû½ Irregular Ôû½ Regular ÔÇó Irregular Ôû½ Atrial fibrillation Ôû½ Atrial flutter with variable block Ôû½ MAT
- 20. SVT: REGULAR : LOOK FOR- ÔÇó A:V RATIO ÔÇó P WAVE MORPHOLOGY ÔÇó UPRIGHT OR INVERTED ÔÇó R-P DISTANCE ÔÇó Ps hiding in QRS , ST , T WAVES ÔÇó V1 BEST FOR STUDYING P WAVE
- 21. A: V ratio NCTs with A : V ratio >1 ÔÇó Atrial tachycardia ÔÇó Atrial flutter ÔÇó Some rare cases of AVNRT with 2 : 1 block, usually in the His bundle
- 22. ATRIAL TACHYCARDIA Atrial rate > 100 bpm. P wave morphology is abnormal when compared with sinus P wave due to ectopic origin. 3 ectopics p waves should be identical There is usually an abnormal P-wave axis (e.g. inverted in the inferior leads II, III and aVF)
- 23. ATRIAL TACHYCARDIA ÔÇó Usually due to single ectopic focus. ÔÇó The underlying mechanism can involve reentry, triggered activity or increased automaticity. ÔÇó May be paroxysmal or sustained. ÔÇó Multiple causes including digoxin toxicity, atrial scarring, catecholamine excess, congenital abnormalities; may be idiopathic. ÔÇó Sustained atrial tachycardia may rarely be seen and can progress to tachycardia-induced cardiomyopathy
- 24. SVT:REGULAR: A:V > 1 ÔÇó ATRIAL FLUTTER
- 25. ÔÇó NCTs with A : V ratio = 1 Ôû½ Comprise a large and heterogeneous group Ôû½ AVNRT Ôû½ AVRT Ôû½ AT Ôû½ Automatic junctional tachycardia. A: V ratio
- 26. RP INTERVAL ÔÇó The location of the P wave on the ECG is best described by the RP and PR intervals. ÔÇó The tachycardias with short RP intervals have a reentrant mechanism that utilizes the fast pathway of the circuit for retrograde conduction. ÔÇó This causes the P wave on the ECG to appear closer to the terminal portion of the preceding QRS than to the beginning of the following QRS or the P wave is masked within the preceding QRS complex. ÔÇó The long RP tachycardias have either a reentrant mechanism that utilizes a slow pathway of the circuit for retrograde conduction or they have an automatic mechanism.
- 27. R-P interval in cases with 1 : 1 A: V ratio ÔÇó Absence of a visible P wave: Ôû½ AVNRT ÔÇó NCTs with a short R-P interval (P wave in the first one-third of the R-R interval): Ôû½ SLOW FAST AVRT, AVNRT (especially in patients >50 years old) ÔÇó Intermediate R-P interval NCTs (P wave in middle one-third of the R-R interval) : Ôû½ AVNRT (ÔÇ£slow-slowÔÇØ) and AT are more common than AVRT ÔÇó Long R-P NCTs : Ôû½ ATs predominate AVNRT is of the less common ÔÇ£fast-slowÔÇØ variety
- 29. SHORT RP SVT:A:V 1:1 1. SLOW-FAST AVNRT ÔÇó No apparent retrograde p wave:50% psuedo R^ in V1 or psuedo S in inferior leads (RP<70ms)
- 31. AVNRT: MECHANISM ÔÇó If a premature atrial contraction (PAC)arrives while the fast pathway is still refractory, the electrical impulse will be directed solely down the slow pathway. ÔÇó By the time the premature impulse reaches the end of the slow pathway, the fast pathway is no longer refractory hence the impulse is permitted to recycle retrogradely up the fast pathway. ÔÇó This creates a circus movement whereby the impulse continually cycles around the two pathways, activating the Bundle of His anterogradely and the atria retrogradely.The short cycle length is responsible for the rapid heart rate. ÔÇó This is the most common type of re-entrant circuit and is termed Slow-Fast AVNRT
- 32. SHORT RP SVT:A:V 1:1 ÔÇó Orthodromic AVRT : 70MS<RP<PR. ÔÇó Uncommon: AT with PR prolongation: the presence of favours AT.
- 34. LONG RP SVT 1. FAST-SLOW AVNRT (ATYPICAL) positive p waves in v1 and negative p wavses in inferior leads. 2.Orthodromic AVRT using slow Aps (ATYPICAL) 3. AT with normal PR interval. 4.SANRT,INAPPROPRIATE ST