2019 Autoimmune Investor Market Opportunity
- 1. BUSINESS OPPORTUNITIES IN AUTOIMMUNE, CHRONIC INFLAMMATORY AND IMMUNO-INFLAMMATORY DISEASES 1 A huge, but largely invisible unmet need; therefore, untapped market opportunity. CIID disease right now is a new frontier--like cancer was 50 years ago. But unlike cancer, chronic autoimmune/immuno-inflammatory diseases are not viewed as a category, but are scattered over multiple medical specialties, hiding the size of the problem, which is at least equal to cancer, and likely larger. Those investors and entrepreneurs who can see across the silos and scattered rare diseases can address a large unmet need and TAM.
- 2. Autoimmune disease prevalence in U.S. is greater than cancer or heart disease. Not captured in public health statistics, scattered across multiple specialties and body parts, underdiagnosed and misdiagnosed. Growing economic burden costing the U.S. healthcare system billions of dollars in slow diagnosis, costly drugs, and lost work. Huge, growing untapped market Incidence/Prevalence underreported Skyrocketing costs WHY AUTOIMMUNE DISEASE NOW? A large, growing and neglected part of the well-recognized chronic disease epidemic is caused by autoimmune and related inflammatory diseases. In total the 80 - 150 individual autoimmune diagnosis add up to prevalence and costs at least as much as cancer, and because of poor statistics, probably even bigger. While attention is focused on other chronic diseases, AIID prevalence and costs continue to grow, with slow diagnosis, costly drugs and lost productivity particular pain points.
- 3. 3 TODAYʼS BURDEN OF CHRONIC DISEASE 7 of 10 deaths each year are due to chronic disease (2). 133 million Americans suffer from at least one chronic disease (1). 71% of healthcare $ went to treating people with one or more chronic medical conditions in 2014. (3) 38% of chronic disease patients have at least one autoimmune disease.* *Estimate based on the number of Americans with a chronic disease and number of Americans with an autoimmune disease. Let’s frame autoimmune within the context of a growing epidemic of chronic disease in the US. Cancer, diabetes, heart disease, kidney disease, lung disease & obesity, are well-known chronic disease categories attracting digital health investment to launch companies. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5876976/ 133 million people in US have at least one chronic disease. 24-50M have one or more diagnosed autoimmune conditions, but this number is not robust, and given underdiagnosis, likely also low. So 18-37% of the chronic disease group have an AI Dx. AIIDs are comorbid with many other higher-prevalence chronic conditions: e.g., diabetes, obesity, heart & kidney disease, depression & anxiety. https://www.cdc.gov/chronicdisease/resources/infographic/chronic-diseases.htm
- 4. 4 23-50 million Americans with autoimmune diseases (5) 78% of patients with autoimmune diseases are women (6) 16% of US population 25% increase THE INVISIBLE EPIDEMIC OF (AUTO)IMMUNITY have at least one autoimmune disease (7) in likelihood of acquiring more than one autoimmune disease (8) Even using the inadequate 2009 NIH/CDC statistics (only 24 diseases!), total autoimmune prevalence is clearly as large as cancer or heart disease (depending on definitions). It’s likely higher prevalence than cancer.
- 5. CHANGING DEFINITIONS OF CHRONIC INFLAMMATORY DISEASE 5 Immune-Mediated Inflammatory Disease: New research in genomics and microbiomics suggests grouping conditions with dysfunctions in inflammatory pathways (4). Immuno-Inflammatory Diseases Chronic inflammation in the absence of infection, presumably innate immune system dysfunctions. Autoimmune Diseases Dysfunctions of the acquired immune system, typically where immune cells damage normal cells and tissues. Psoriasis RA IBD Thyroid SLE One reason the size of the epidemic is understated is that our understanding of immunological diseases is rapidly changing, and scientific terminology remains in flux. Over the 10 years that we have been researching, various broader definitions have been proposed: chronic inflammatory disease is an umbrella concept, with classic autoimmune diseases a sub-category capturing diseases of the acquired immune system and a new category: immuno-inflammatory diseases encompassing syndromes and conditions that may be innate immune system dysfunctions. Various terms are used in the scientific literature: Chronic Inflammatory Disease (CID) or Chronic ImmunoInflammatory (CIID) or Autoimmune Inflammatory Disease AIID. Genomics is giving us a new lens to look at the spectrum of inflammatory disease, which ranges from classic autoimmune disease like lupus (SLE) to diseases where inflammation predominates like IBD.
- 6. 6 RISING INCIDENCE AND PREVALENCE OF (AUTO)IMMUNE DISEASES However, as we dug through the WWW, it’s easy to see that not only is there a significant prevalence burden (and not just in the US), but that it is increasing worldwide. Since these data are generally extrapolated from limited sets looking at the better-known diseases (type 1 diabetes, RA, lupus, Psoriasis, celiac, IBD) they have limitations. However, when one totals up the individual disease prevalence and costs, these rapidly exceed the top-down estimates. It’s clear the problem is understated and growth not well tracked.
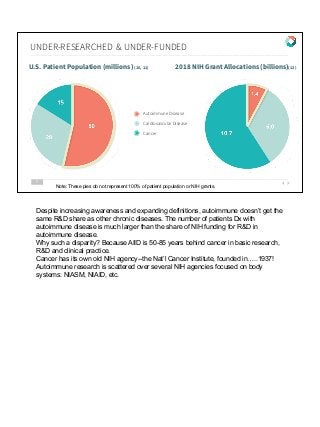
- 7. UNDER-RESEARCHED & UNDER-FUNDED 7 U.S. Patient Population (millions) (10, 11) 2018 NIH Grant Allocations (billions)(12) Autoimmune Disease Cardiovascular Disease Cancer Note: These pies do not represent 100% of patient population or NIH grants. Despite increasing awareness and expanding definitions, autoimmune doesn’t get the same R&D share as other chronic diseases. The number of patients Dx with autoimmune disease is much larger than the share of NIH funding for R&D in autoimmune disease. Why such a disparity? Because AIID is 50-85 years behind cancer in basic research, R&D and clinical practice. Cancer has its own old NIH agency--the Nat’l Cancer Institute, founded in…..1937! Autoimmune research is scattered over several NIH agencies focused on body systems: NIASM, NIAID, etc.
- 8. 8 THE GROWING COST BURDEN OF AUTOIMMUNE U.S. Spending on Specialty Medicines for Autoimmune Diseases Biologic Drugs for Autoimmune Disorders (BDAIDs) has highest forecasted category growth, estimated to increase by 90% Per Member Per Month spend by 2022 (13). . This is the most visible impact of autoimmune disease on the health care system: Care can be expensive, especially specialty biologics that must be used chronically, and have been constantly going up in price, leading to huge pharmacy costs. Medical costs can be big, too, not only more frequent clinician visits, but also flare-triggered emergencies and hospitalizations, sometimes surgery (IBD, RA). Employers may also measure productivity costs: absenteeism, presenteeism, medical leaves of absence, disability & lost employment. Costs borne by patients, which are generally not captured in the statistics. - Co-pays for Rx and medical visits. - Slow, missed or misdiagnosis - Multiple doctor visits, waits for specialists, transportation & childcare costs. Quality of life, caretakers, other hard to quantify costs.
- 9. SLOW DIAGNOSIS & MISDIAGNOSIS 80-100+ different types of autoimmune diseases (14) 3-5 years to diagnosis (15) 5 doctors for accurate disease diagnosis (16) misdiagnosis Still too frequent For example, average rate of misdiagnosis is 10% for MS & 7.5% for IBD (17) (18). Early, accurate diagnosis is generally recognized as essential to better management of chronic diseases. We do not have that now in autoimmune. Missed or delayed diagnosis: failure to detect a disease or diagnosing it later in progression. Misdiagnosis: diagnosing a disease that is not there or the wrong diagnosis. On average, autoimmune patients wait 3-5 years and see 4-5 different doctors (many of those scarce specialists) for a diagnosis. Many reasons: early symptoms are vague and systemic (fatigue, rash, fever, aches). But most diagnoses depend on hallmark tissue damage, like joint inflammation, skin lesions or neurological symptoms. Waiting until these symptoms appear is still usual, even though disease progresses towards more irreversible damage. PCPs may not be educated to consider autoimmune diseases, so do not refer patients to specialists early in their journeys. Even when they do, the shortage of specialists means that many patients wait months to get their first appointment. Then follows a series of blood labs and/or imaging tests and maybe referrals to more specialists. Lack of coordination contributes to slow and missed diagnosis. Patients are mostly responsible for coordinating their own care, finding appointments, childcare & transportation, taking time off work, all a burden for those with typical symptoms of
- 10. fatigue and exhaustion. Remember, diagnoses are maps of disease, collections of signs & symptoms, not real biological categories. Multiple autoimmune diagnoses in the same patient (~25% of AIID pts) point to underlying systemic dysfunction affecting multiple tissues & organs. But siloed clinical care means that 3 or 4 specialists may manage one patient’s diseases; specialists who may not communicate with each other at all!
- 11. - Misaligned incentives: costly to treat, costly to delay treatment - Multiple physician visits, specialists, coordination - Slow diagnosis, missed or misdiagnoses - Lost productivity: absenteeism, presenteeism, unemployment - Quality of life: limited activity, pain & fatigue, mental illness, financial hardship - TCOC not seen by payers: missing employment, caretaker costs, QoL, disability - Complex ecosystem of means Rx pricing is irrational, bad market feedback - Administrative burden is a costly annoyance to every stakeholder. 10 PAYER - EMPLOYER - PROVIDER - PHARMA - PATIENT PAIN POINTS All this adds up to a major problem for employers, payers and providers, one that is probably underestimated. But the pain points are different for each stakeholder group. Payers want to reduce costs, using UM, PBM, step-therapy, prior approvals and other tactics that slow or impede care. They also only bear the Rx & medical costs and are indifferent to indirect costs & productivity. They do not see TCOC. Employers, especially those with one plans, do see productivity (absenteeism, presenteeism, accommodations, disability) and some indirect costs as well as Rx & medical usage. Providers want to practice to the best of their ability, but FFS incentivizes them to do more procedures, rather than holistically manage chronic patients. Time-constrained clinicians often prescribe a drug and see the patient annually, rather than pursue unreimbursed NPI & lifestyle efforts that could complement or reduce drug use. Pharma/life science wants to maximize drug revenue and profits, block competition, even if that doesn’t improve outcomes. They lack companion diagnostics that might better match costly drugs to the right patients and monitor outcomes. Patients want as much care as possible at the lowest cost to them; many cannot afford high co-pays on biologics. They bear the burden of indirect costs (care
- 12. coordination, EMR recon, childcare, caretakers, transportation, accommodations). Losing a job through disability can mean losing continuity of care or being unable to continuing paying. These conflicting goals are a big reason for the ever-growing costs of US healthcare with seemingly little improvement in outcomes.
- 13. 11 FRAGMENTED CARE IS WASTEFUL, COSTLY, FRUSTRATING CURRENT MODEL OF CARE: Lack of coordination between practitioners forces patients to seek multiple specialists on their own. Lifestyle factors such as exercise, nutrition and sleep are not addressed in most conventional medical practices. Specifically, an area of unmet need that may be low-hanging fruit is to improve care coordination. Multiple specialists mean patients mostly do their own coordination (not captured in costs!), from finding providers to making appointments, paying for transportation, childcare and time off work. These multiple specialists are not a team, either. It’s usually up to the patient to make sure history & medical records get to the next doctor, and rarely do any of these specialists confer with each other. This causes not only inconvenience and effort for sick patients, but also may lead to polypharmacy, conflicting medications or other problems. Add a psychologist, nutritionist, PT/exercise, sleep specialist, who may not be covered by payers, and patients (or their caretakers) become managers of their own care. Most conventional providers, from PCPs to internists to GI, rheum & other specialists, do not address lifestyle factors, in part because there is no reimbursement pathway, but also because these interventions have only recently migrated from functional medical practice to conventional care.
- 14. 12 CONNECTING THE DOTS - PATIENT-CENTERED CARE 1ST STEP TO BETTER CARE: Put patients at the center Bring all aspects of care TO them. Digital tools can enable better collaboration among specialists and increase coordination between lifestyle modifications and medical care. So it would be a major step to provide better coordination to patients, with providers connected to each other by more than passing EHRs along the referral path. Digital technology can help here, not only mobile electronic communications, but remote monitoring and telemedicine. Smart watches, smart phones, telemedicine can connect specialists with patients and each other, building a multidisciplinary clinical care team that can share data (including -omics), collaborate on care plans and communicate with patients between in-person visits. Such multidisciplinary care teams already practice in B&M: e.g. Allegheny Health’s autoimmune center of excellence. But they have limited geographic reach, many patients cannot travel to them, and they have not yet adopted digital communications. Much less telemedicine, in an integrated way.
- 15. 13 OPPORTUNITIES TO ADDRESS UNMET NEEDS Digital coordination and communication, EHRs, telemedicine, wearables, etc. Workplace/employer-sponsored digital therapeutics, coaching, monitoring. Personalized diagnostics & monitoring, lifestyle interventions (e.g., diet, probiotics, etc.) Genomics, Microbiomics, drug discovery & development, companion diagnostics. Population health, data analytics, data sharing. 1. Offer coaching, coordination, monitoring and digital therapeutics to plan members stratified by risk. 2. Personalized diagnostic & monitoring tools to enable lifestyle & behavior changes. 3. Biomarkers and digital biomarkers to better match drugs to patients, monitor response, track outcomes. 4. Use digital IT to better coordinate care, offer 24/7 communication channels, support telemedicine, deploy remote devices, etc. 5. Use population analytics to find and address high-risk members who may not even be aware that they are sick so they can be diagnosed faster before disease progression.
- 16. IBD Coaching EHR/PHR Telemedicine Wearables Genomics Microbiomics Data Analytics MONITORING/DIAGNOSTICS MICROBIOME THERAPEUTICS DIGITAL Digital health business models can help bring together aspects of care that are currently fragmented. Lab diagnostics and biomarkers (blood, imaging, digital) are a weak point in autoimmune, as seen in slow Dx, difficulty matching patients to drugs, low response rates (30%), tapering, switching and breakthrough meds. Genetics & microbiomics are not yet a standard part of clinical care, even though these are important mediators of autoimmune disease and might provide clues for early detection, even prevention.
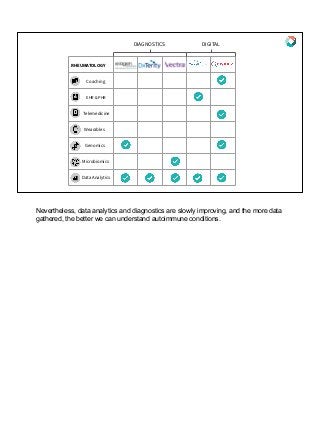
- 17. RHEUMATOLOGY Coaching EHR & PHR Telemedicine Wearables Genomics Microbiomics Data Analytics DIAGNOSTICS DIGITAL Nevertheless, data analytics and diagnostics are slowly improving, and the more data gathered, the better we can understand autoimmune conditions.
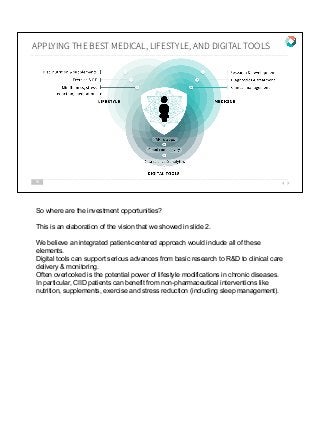
- 18. 16 APPLYING THE BEST MEDICAL, LIFESTYLE, AND DIGITAL TOOLS So where are the investment opportunities? This is an elaboration of the vision that we showed in slide 2. We believe an integrated patient-centered approach would include all of these elements. Digital tools can support serious advances from basic research to R&D to clinical care delivery & monitoring. Often overlooked is the potential power of lifestyle modifications in chronic diseases. In particular, CIID patients can benefit from non-pharmaceutical interventions like nutrition, supplements, exercise and stress reduction (including sleep management).
- 19. 17 AN AUTOIMMUNE NETWORK - A FUTURE VISION OF CARE FUTURE BIG PICTURE: Applying data, personalized genomics and microbiomics to unite the best of conventional, integrative and digital medicine, patients can network with coaches, specialists to amplify their own efforts to manage, even prevent, their chronic inflammatory disease(s.) A more complete view of our vision of future care…. This requires interoperable EHRs, asynchronous digital communication between providers and patients through phone apps, wearables and remote monitoring devices, as well as virtual visits and 24/7 patient support. This can empower patients to be more engaged and involved with their own lifelong chronic disease management, without having to coordinate everything themselves. And providers can act more like an interdisciplinary team, communicating with each other as well as the patient.
- 20. 18 MARKET CHALLENGES Incomplete scientific understanding of causes, biology, and epidemiology. Silo fragmentation across research, diagnosis, and care. Slow Dx, misDx, late intervention, costly treatments, poor outcomes, side effects, non-adherence. Poor quality of life, reduced productivity, employer costs, no prevention. So what is preventing us from reaching the vision? Autoimmune is trapped in multiple silos, from research to care delivery; awareness is slowly increasing, but not as fast as the growing unmet need. This impedes scientific understanding of the common elements in CIIDs. Cancer is 50-85 years ahead of autoimmune as a research field. Large number of drugs in development but little understanding of how to match costly drugs to the patients that will respond. Specialists see the individual disease, not the patient as a whole. This all leads to slower and less accurate diagnosis, late interventions. Ultimately, we should aim to improve quality of life & productivity and even find ways to delay or prevent active disease.
- 21. 19 CAPTURING POTENTIAL VALUE - DIRECT & INDIRECT COSTS Launching companies that can demonstrate a positive ROI to sell their solutions to payers/payviders/employers means finding the right patient subpopulation (analysis), careful data collection, using TCOC and the complete burden of AIIDs to find ways to improve outcomes while slowing or even reducing costs. Companies should use analytics to demonstrate value within target populations.
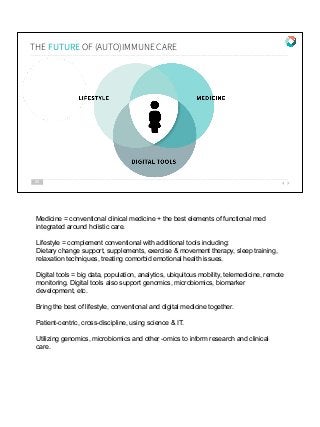
- 22. THE FUTURE OF (AUTO)IMMUNE CARE 20 Medicine = conventional clinical medicine + the best elements of functional med integrated around holistic care. Lifestyle = complement conventional with additional tools including: Dietary change support, supplements, exercise & movement therapy, sleep training, relaxation techniques, treating comorbid emotional health issues. Digital tools = big data, population, analytics, ubiquitous mobility, telemedicine, remote monitoring. Digital tools also support genomics, microbiomics, biomarker development, etc. Bring the best of lifestyle, conventional and digital medicine together. Patient-centric, cross-discipline, using science & IT. Utilizing genomics, microbiomics and other -omics to inform research and clinical care.
- 23. 1 Coordinate care with technology assistance (telemedicine, scheduling apps to bridge silos and reduce hand-offs). Support diagnostics via AI or algorithms to differentiate classic autoimmune diseases from inflammatory syndromes & conditions. CENTER OF EXCELLENCE CARE BUNDLE TO CAPTURE VALUE Guide treatment via algorithms and processes: picking best drugs quickly at lower total cost of disease management. Holistic disease management, not just med adherence & appointments: sleep, physical therapy, pain, exercise, fatigue, diet, supplements. 2 3 4 Today’s brick & mortar Centers of Excellence provide a model of multidisciplinary care (e.g., Allegheny Autoimmune), but have not yet adopted digital tools like telehealth to help them with care coordination and patient communication or to scale beyond their regional reach. Can this model be virtualized?
- 24. 22 VIRTUAL CENTER OF EXCELLENCE VISION OF THE FUTURE A B C Integrate alternative modalities, especially diet/nutrition, PT, sleep, psychological support, self-care. Apply genomics, microbiomics & biomarkers for better Dx and treatment matching. Support patients to increase productivity, decrease absenteeism, work more easily, QoL, life/work balance. 22 D Early detection, even prediction: population and genomics analyses, better biomarkers, awareness campaigns for payers, practices & patients. The future vision will include additional elements from advances in science and technology. A virtual center of excellence could serve distant patients and scale to serve more.
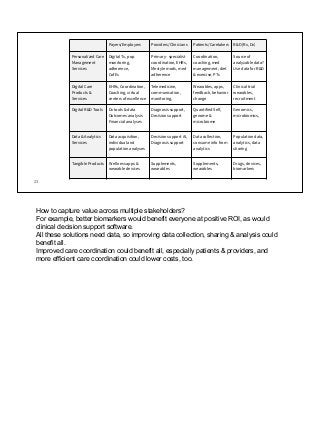
- 25. 23 Payers/Employers Providers/Clinicians Patients/Caretakers R&D (Rx, Dx) Personalized Care Management Services Digital Tx, pop monitoring, adherence, CofEs Primary - specialist coordination, EHRs, lifestyle mods, med adherence Coordination, coaching, med management, diet & exercise, PTs Source of analyzable data? Use data for R&D Digital Care Products & Services EHRs, Coordination, Coaching, virtual centers of excellence Telemedicine, communication, monitoring, Wearables, apps, feedback, behavior change Clinical trial wearables, recruitment Digital R&D Tools Dx tools & data Outcomes analysis Financial analyses Diagnosis support, Decision support Quantified Self, genome & microbiome Genomics, microbiomics, Data & Analytics Services Data acquisition, individual and population analyses Decision support AI, Diagnosis support Data collection, consume info from analytics Population data, analytics, data sharing Tangible Products Wellness apps & wearable devices Supplements, wearables Supplements, wearables Drugs, devices, biomarkers How to capture value across multiple stakeholders? For example, better biomarkers would benefit everyone at positive ROI, as would clinical decision support software. All these solutions need data, so improving data collection, sharing & analysis could benefit all. Improved care coordination could benefit all, especially patients & providers, and more efficient care coordination could lower costs, too.
- 26. Raghupathi, Wullianallur, and Viju Raghupathi. “An Empirical Study of Chronic Diseases in the United States: A Visual Analytics Approach to Public Health.” International Journal of Environmental Research and Public Health, vol. 15, no. 3, 2018, p. 431., doi:10.3390/ijerph15030431. 1. 133 million Americans... Centers for Disease Control and Prevention. The Power to Prevent, The Call to Control. (2009) Accessed at http://www.cdc.gov/chronicdisease/resources/publications/AAG/chronic.html 2. 7 out of 10 deaths... Gerteis J, Izrael D, Deitz D, LeRoy L, Ricciardi R, Miller T, Basu J. Multiple Chronic Conditions Chartbook. Cdc-pdf AHRQ Publications No, Q14-0038. Rockville, MD: Agency for Healthcare Research and Quality; 2014. Accessed November 18, 2014 3. 71% of healthcare dollars... Kuek, A., et al. “Immune-Mediated Inflammatory Diseases (IMIDs) and Biologic Therapy: a Medical Revolution.” Postgraduate Medical Journal, vol. 83, no. 978, 2007, pp. 251–260., doi:10.1136/pgmj.2006.052688. 4. Immune Mediated Inflammatory Disease https://pixabay.com/en/skyscraper-glass-facade-offices-418189
- 27. https://www.aarda.org/news-information/statistics/ 5. 23-50 million Americans Fairweather, Delisa, et al. “Sex Differences in Autoimmune Disease from a Pathological Perspective.” The American Journal of Pathology, vol. 173, no. 3, 2008, pp. 600–609., doi:10.2353/ajpath.2008.071008. 6. 78% of patients Kuek, A., et al. “Immune-Mediated Inflammatory Diseases (IMIDs) and Biologic Therapy: a Medical Revolution.” Postgraduate Medical Journal, vol. 83, no. 978, 2007, pp. 251–260., doi:10.1136/pgmj.2006.052688. 7. Immune Mediated Inflammatory Disease Cojocaru, M, et al. “Multiple Autoimmune Syndrome.” Journal of Clinical MEdicine, vol. 5, no. 2, Apr. 2010. 8. 25% increase in likelihood Kuek, A., et al. “Immune-Mediated Inflammatory Diseases (IMIDs) and Biologic Therapy: a Medical Revolution.” Postgraduate Medical Journal, vol. 83, no. 978, 2007, pp. 251–260., doi:10.1136/pgmj.2006.052688. 9. 23-50 million Americans https://pixabay.com/en/skyscraper-glass-facade-offices-418189
- 28. “Cancer Treatment: Survivor Facts & Figures.” American Cancer Society, www.cancer.org/research/cancer-facts-statistics/survivor-facts-figures.html. 10. Population with cancer https://ftp.cdc.gov/pub/Health_Statistics/NCHS/NHIS/SHS/2017_SHS_Table_A-1.pdf 11. Population with heart disease https://report.nih.gov/categorical_spending.aspx 12. 2018 NIH Grant Allocation https://www.iqvia.com/-/media/iqvia/pdfs/institute-reports/medicines-use-and-spending-shifts-in-the-us-in-2014.pdf 13. Increase in Specialty Spending https://www.aarda.org/news-information/statistics/#1488234345468-3bf2d325-1052 14. 80-100+ Autoimmune Diseases https://pixabay.com/en/skyscraper-glass-facade-offices-418189
- 29. ● https://www.aarda.org/who-we-help/patients/women-and-autoimmunity/#1481574903922-68688035-6be6 ● https://www.benaroyaresearch.org/blog/post/diagnosing-autoimmune-diseases 15. 3-5 years to diagnosis https://www.aarda.org/who-we-help/patients/women-and-autoimmunity/#1481574903922-68688035-6be6 16. 5 doctors to diagnosis Solomon, Andrew J, and Brian G Weinshenker. “Misdiagnosis of Multiple Sclerosis: Frequency, Causes, Effects, and Prevention.” Current Neurology and Neuroscience Reports, vol. 13, no. 403, 20 Oct. 2013, link.springer.com/article/10.1007/s11910-013-0403-y. 17. Multiple Sclerosis Misdiagnosis Lee, Ho-Su, et al. “Change in the Diagnosis of Inflammatory Bowel Disease: a Hospital-Based Cohort Study from Korea.” Intestinal Research, vol. 14, no. 3, 27 June 2016, www.ncbi.nlm.nih.gov/pmc/articles/PMC4945530/. 18. IBD Misdiagnosis https://pixabay.com/en/skyscraper-glass-facade-offices-418189
- 31. END 29
- 32. 30 ABOUT US Bonnie Feldman DDS, MBA â—Ź Retired dentist â—Ź Wall Street analyst â—Ź Autoimmune patient & advocate â—Ź Investor Relations â—Ź Digital Health (early adopter and expert) Ellen M Martin MBA â—Ź Biopharma strategy & marcomm â—Ź PR & IR virtual agency â—Ź Finance & marketing â—Ź IT for healthcare â—Ź Devices & medtech â—Ź Autoimmune caretaker
- 33. Lack of awareness of the growing incidence and prevalence of chronic inflammatory diseases is near-universal, despite their huge economic burden and impact on population health. Therefore, this invisible epidemic represents a huge, growing, and untapped market opportunity. With a patient-centered focus on digital health platforms, we work with entrepreneurs to improve research, diagnosis, treatment and lifestyle management for chronic inflammatory diseases. From SXSW- themes of Femtech investing, #metoo, #timeisup -the invisibility of the chronic inflammatory diseases epidemic deferentially affects women, and more research focus is needed on women and woc to address this neglect. Make contact page a separate slide