Figure neuropsiquiatria__neuropsiquiatria__e__o.c.d.
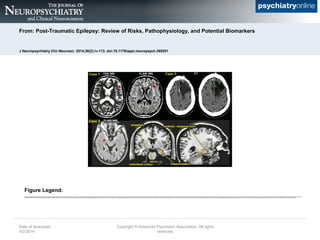
- 1. From: Post-Traumatic Epilepsy: Review of Risks, Pathophysiology, and Potential Biomarkers J Neuropsychiatry Clin Neurosci. 2014;26(2):iv-113. doi:10.1176/appi.neuropsych.260201 Post-traumatic epilepsy (PTE) can develop following traumatic brain injuries (TBIs) of all levels of severity, as illustrated by these three cases. Case 1: A 58-year-old man who experienced a mild TBI as a result of a roll over collision as a teenager. He developed generalized convulsions within five years from injury. MRI obtained after onset of PTE demonstrated a single 3 mm nonspecific gliotic focus in the left frontal white matter (arrow) that is well visualized on both T2 weighted (T2W) and FLAIR sequences. Case 2: A 49-year-old man with mesial temporal sclerosis secondary to TBI as a result of a recent fall from a ladder. The temporal horns of the lateral ventricles are colored red. Note the dilation of the tip of the right temporal horn due to volume loss in the surrounding temporal lobe structures. The basic anatomy of the medial temporal lobe is illustrated on coronal and sagittal MRI of a healthy individual. The hippocampus (yellow) and temporal horn of the lateral ventricle (red) are color-coded and adjacent structures are labeled. Case 3: A 66-year-old man who experienced a severe TBI because of a gunshot wound to the left frontal lobe when he was 19 years of age. He developed seizures within 2 years following this injury. His seizures are described as generalized stiffening of upper and lower extremities followed by convulsive activity. CT demonstrates chronic postoperative changes with a large area of encephalomalacia involving the left frontal lobe. Date of download: 9/2/2014 Copyright ┬® American Psychiatric Association. All rights reserved. Figure Legend: