Complement regulation
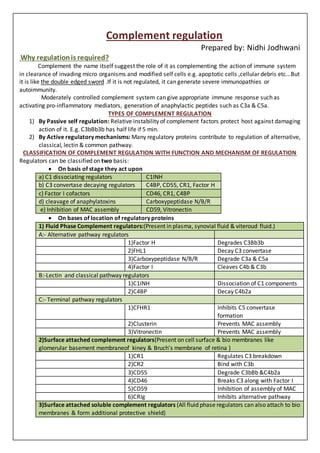
- 1. Complement regulation Prepared by: Nidhi Jodhwani Why regulationis required? Complement the name itself suggest the role of it as complementing the action of immune system in clearance of invading micro organisms and modified self cells e.g. apoptotic cells ,cellular debris etc...But it is like the double edged sword .If it is not regulated, it can generate severe immunopathies or autoimmunity. Moderately controlled complement system can give appropriate immune response such as activating pro-inflammatory mediators, generation of anaphylactic peptides such as C3a & C5a. TYPES OF COMPLEMENT REGULATION 1) By Passive self regulation: Relative instability of complement factors protect host against damaging action of it. E.g. C3bBb3b has half life if 5 min. 2) By Active regulatory mechanisms: Many regulatory proteins contribute to regulation of alternative, classical, lectin & common pathway. CLASSIFICATION OF COMPLEMENT REGULATION WITH FUNCTION AND MECHANISM OF REGULATION Regulators can be classified on two basis: ï· On basis of stage they act upon a) C1 dissociating regulators C1INH b) C3 convertase decaying regulators C4BP, CD55, CR1, Factor H c) Factor I cofactors CD46, CR1, C4BP d) cleavage of anaphylatoxins Carboxypeptidase N/B/R e) Inhibition of MAC assembly CD59, Vitronectin ï· On bases of location of regulatory proteins 1) Fluid Phase Complement regulators:(Present in plasma, synovial fluid & viteroud fluid.) A:- Alternative pathway regulators 1)Factor H Degrades C3Bb3b 2)FHL1 Decay C3 convertase 3)Carboxypeptidase N/B/R Degrade C3a & C5a 4)Factor I Cleaves C4b & C3b B:-Lectin and classical pathway regulators 1)C1INH Dissociation of C1 components 2)C4BP Decay C4b2a C:- Terminal pathway regulators 1)CFHR1 Inhibits C5 convertase formation 2)Clusterin Prevents MAC assembly 3)Vitronectin Prevents MAC assembly 2)Surface attached complement regulators(Present on cell surface & bio membranes like glomerular basement membraneof kiney & Bruchâs membrane of retina ) 1)CR1 Regulates C3 breakdown 2)CR2 Bind with C3b 3)CD55 Degrade C3bBb &C4b2a 4)CD46 Breaks C3 along with Factor I 5)CD59 Inhibition of assembly of MAC 6)CRIg Inhibits alternative pathway 3)Surface attached soluble complement regulators (All fluid phase regulators can also attach to bio membranes & form additional protective shield)
- 2. VARIOUS DISEASES CAN OCCUR IN HUMANS AS THE OUTCOME OF DEFECT IN COMPLEMENT REGULATION As the complement regulation is important in protection of host cell along with removal of invading micro organisms, any disturbance in this regulation can result into host cell damage and accumulation of immune debris. Some of them are described below:- 1) Hereditary angioedema: ï· Affected regulator:C1INH ï· Function of regulator: Dissociation of C1 complement ï· Ratio: occurs 1 in 1000 ï· Pathophysiology: Leads to excessive production of vasoactive mediators -Results into tissue swelling and extracellular fluid accumulation -Abdominal pain and upper respiratory track pain 2) aHUS (atypical Haemolytic Uremia): ï· Affected regulator: Factor H, Factor I ï· Function of regulator:Degrade C3 convertase ï· Pathophysiology: Antibody against Factor H produced which binds with C terminal of Factor H -No degradation of C3 convertase -More C3 cleavage results into more C3a production(anaphylatoxin) -Damage to kidney 3)AMD (Age relatedMacular Degeneration): ï· Affected regulator: Factor H ï· Function of regulator: Degrade C3 convertase ï· Pathophysiology: No Factor H because of defect in gene coding for that factor -No degradation of C3 convertase -More C3 cleavage results into more C3a production(anaphylatoxin) -Severe inflammation results into vasodialation -Accumulation of exudates in center of retina -Blurred central vision 4)MPGN type II(Membrane Proliferative GlomeruloNephritis type II) OR DDD (Dense Deposit Disease) ï· Affected regulator: Factor H ï· Function of regulator: Degrade C3 convertase ï· Pathophysiology: Uncontrolled complement activation -Excess C3 convertase -Excess of C3 cleavage results into overproduction of C3a -C3a deposits on glomerular basement-membrane of kidney & Bruchâs membrane of retina. 5)SLE(systemic lupus erythematosus): An auto immune disease in which more amount of immune- complexes are generated and defect in regulation can result into defective clearance of these complexes thus local chronic inflammation occurs. Referance:1)Complement regulators and inhibitory proteins;Peter F. Zipfel and ChristineSkera,2009 Macmillan Publishers Limited. 2) OEWN, PUNT, SANFORD; Kuby Immunology; seventh edition;2013; W.H. Freeman and company; New York 3)Wikipedia.org