case study on cellulitis
- 1. CASE PRESENTATIO N ON CELLULITIS PRESENTED BY: AKKI YAMUNASRIVALLI PHARM-D 3rd YR ROLL NO: 13 BROWNS COLLAGE OF PHARMACY
- 2. ŌĆó A 60 year old male patient admitted with the chief complaints of with swelling , heavy pain and tenderness in his left foot.
- 4. ŌĆóPATIENT NAME : XXXXX ŌĆóAGE : 60 yrs ŌĆóSEX : MALE ŌĆóIP NUMBER : 1698 ŌĆóDEPARTMENT :ORTHOPEDIC ŌĆóWEIGHT : 80 kgs
- 5. ŌĆó PAST MEDICAL HISTORY : NIL PAST MEDICATION HISTORY :NIL ŌĆó SOCIAL HISTORY SMOKER : NO ALCOHOL : YES MARITAL STATUS : MARRIED
- 7. VITAL SIGNS: DURATION DAY 1 DAY 2 DAY 3 TEMERATURE 102 100 100 BP 110/80 110/70 120/60 PULSE 83 82 88
- 8. PROVISIONAL DIAGNOSIS It might be a case of ŌĆ£CELLULITISŌĆØ developed due to in-present diabetis.
- 9. LAB INVESTIGATIONS PARAMETERS NORMAL VALUES OBSERVEDVALUES Haemoglobin M:14-16,F:13-15 11.2gm WBC COUNT 4000-11000cells/cmm 17,300cell/cmm DC: NEUTROPHILS 40-80% 82% ESINOPHILS 1-6% 7% BASOPHILS 1-2% 3% LYMPHOCYTES 20-40% 45% MONOCYTES 2-10% 15% BLOOD SUGAR: RBS 80-140 mg/dl 110mg/dl FBS 80-100mg/dl 90mg/dl PPBS 120-160mg/dl 140mg/dl
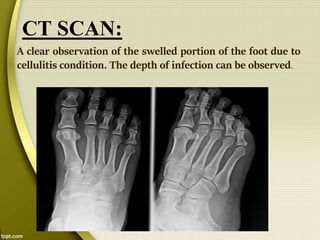
- 10. CT SCAN: A clear observation of the swelled portion of the foot due to cellulitis condition. The depth of infection can be observed.
- 11. DIAGNOSIS Based on CT-SCAN report and clinical manifestations, it is identified as ŌĆ£cellulitisŌĆØ 11
- 12. PLAN S.no DRUGS FREQUENCY DOSE Day 1 Day 2 Day 3 Day 4 1. Metrogyl (metranidazole) BD 500mg + + + + 2. Tramadol (ultram) BD 50mg + + + + 3. Voveran(diclofe nac sodium) BD 100gm + + + + 4. Taxim (cefataxime) BD 250mg + + + + 5. Rantac (rantidine) BD 150mg + + + + 6. Dicloxacillin BD 250mg + ŌłÆ + + 7. Ampicillin (omnipen) BD 500 ml + + + +
- 13. PHARMACISTS INTERVENTION: ŌĆóPatients should be encouraged to inspect their feet daily and to apply water-based moisturizer. ŌĆóElastic socks should be avoided, as they impair circulation . ŌĆóDo not take METROGYL if you are allergic to medicines containing metronidazole, any other nitroimidazole medicine. ŌĆóTRAMADOL should not be consumed if you have used alcohol, sedatives, tranquilizers, or narcotic medications within the past few hours. TRAMADOL can slow or stop your breathing, especially when you start using this medicine or whenever your dose is changed. Never take tramadol in larger amounts, or for longer than prescribed .
- 14. ŌĆóBefore taking AMPICILLIN, tell your doctor or pharmacist if you are allergic to it; or to PENICILLIN or CEPHALOSPORIN ANTIBIOTICS; or if you have any other allergies. This product may contain inactive ingredients, which can cause allergic reactions.
- 15. CELLULITIS ŌĆó Cellulitis is a bacterial infection involving Inflammation of subcutaneous connective tissue i.e. the inner layers of the skin. It specifically affects the dermis and the subcutaneous fat. ŌĆó The legs and face are the most common sites involved, though cellulitis can occur on any part of the body. ŌĆó The leg is typically affected following a break in the skin
- 16. ETIOLOGY: ’üČ Cellulitis is a condition caused by bacterial infection like Staphylococcus aureus (S. aureus) and Streptococcus pyogenes (S. pyogenes), or by a wide variety of exogenous bacteria. ’üČ Bacteria enter into the body in many ways: Broken skin, burns, insect bites, surgical incisions and intravenous (IV) catheters are all potential pathways.
- 17. ’üČ Many other bacteria causes cellulitis. ’üČHaemophilus influenza causes fascial cellulitis in young children. ’üČ Pasteurella multocida leads to cellulitis associated with animal bites, mostly those of cats. ’üČ Aeromonas hydrophila can cause an aggressive form of cellulitis in a laceration sustained in fresh water. ’üČ Gram-negative bacillary (rod) cellulitis, like P. aeruginosa, is common among hospitalized, immunocompromised patients and may have multidrug resistance.
- 18. ’üČWhen bacteria enters the skin, it leads to redness and swelling around the site of the infection. If the bacteria gets into the bloodstream or into the deeper layers of the skin, complications can occur. ’üČ Areas where the skin is dry and flaking, broken, or wounded are the most likely sites for bacteria to enter the body. ’üČInsect bites may also transmit bacteria that can cause a skin infection. ’üČ The pathophysiology of cellulitis commonly starts out affecting the lower leg. The infected skin may be red, swollen, and painful to the touch. The red rash area may get worse or spread over time. PATHOPHYSIOLOGY
- 19. ŌĆó Any condition that causes chronic skin disruption, such as eczema, can increase a skin infection. ŌĆóThe cellulitis can be made more severe by a weakened immune system caused by conditions such as diabetes or HIV. Chronic cellulitis can damage the lymphatic system and cause chronic swelling of the infected area. ŌĆóIn rare cases, the bacteria can spread to the fascial lining, a deep layer of skin tissue. This is a very severe complication and a medical emergency.
- 20. INFECTED FOOT WITH CELLULITIS ŌĆó Chronic stage of cellulitis left untreated causing heavy damage in the foot
- 21. CELLULITIS EFFECTING EYE An open wound in the eye causing cellulitis
- 22. CELLULITIS IN HAND An open wound in the hand causing cellulites due bacterial infection
- 23. SIGNS AND SYMPTOMS: ’üČPain and tenderness in the affected area. ’üČ Redness or inflammation on your skin. ’üČTight and swollen appearance of the skin. ’üČ A feeling of warmth in the affected area. ’üČ Fever.
- 24. RISK FACTORS: ’üČInjury. Any cut, fracture, burn gives bacteria an entry point. ’üČWeakened immune system. Conditions that weaken your immune system ŌĆö such as diabetes, leukemia and HIV/AIDS ŌĆö leave you more susceptible to infections. Certain medications, such as corticosteroids, also can weaken your immune system. ’üČSkin conditions. Skin disorders ŌĆö such as eczema, athlete's foot, chickenpox and shingles ŌĆö can cause breaks in the skin and give bacteria an entry point. ’üČChronic swelling of your arms or legs (lymphedema). Swollen tissue may crack, leaving your skin vulnerable to bacterial infection.
- 25. HISTORY OF CELLULITIS: People who previously had cellulitis, especially of the lower leg, may be more prone to develop it again. ŌĆóINTRAVENOUS DRUG USE: People who inject illegal drugs have a higher risk of developing cellulitis. ŌĆóOBESITY: Being overweight or obese increases your risk of developing cellulitis and having recurring episodes.
- 26. COMPLICATIONS: ’üČ Blood poisoning. ’üČ Abscesses. ’üČ Necrotising fasciitis. ’üČ And also meningitis.
- 27. DIAGNOSIS: ŌĆó The condition of cellulitis is diagnosed by using computerized tomography (CT scan). ŌĆó CT scan: CT is used to accurately differentiate between superficial cellulitis and deep cellulitis(cellulitis associated with deep-seated infection). ŌĆó In uncomplicated cellulitis, CT demonstrates skin thickening, septation of the subcutaneous fat, and thickening of the underlying superficial fascia.
- 28. Goals of treatment: ’üČGenerally the treatment of cellulitis is done based on the severity of infection. The treatment involves the following : ’üČWhen there is acute or early stage of cellulitis the patient is treated with the anti microbial therapy by giving a list of antibiotics and said to be used for one month and medication should be used until the prescribed medicines are finished. ’üČThe IV and IM treatment is given in the following conditions , ’üČ 1.If the infection is severe. ’üČ 2. If the patient have other medical problems
- 29. 3.If the effected person is very young or very old. 4.If the cellulitis involves areas close to important structures; for example, infection around the eye socket. DRUGS SPECIFICALLY USED: ’üČ DICLOXACILLIN- 250 mg (OR) CEPHALEXIN- 500 mg is given orally T.I.D in the acute infections. ’üČ Clindamycin or a macrolide (CLARITHROMYCIN OR AZITHROMYCIN) are reasonable alternatives in patients who are allergic to penicillin. ’üČ Usually, cellulitis is presumed to be due to staphylococci or streptococci infection and may be treated with CEFAZOLIN, CEFUROXIME, CEFTRIAXONE, NAFCILLIN, OR OXACILLIN
- 30. STANDARD TREATMENT DRUGS GENERIC NAME DOSAGE FREQUENCY Cefuroxime Zinacef 250mg BD IV Clindamycin Cleocin 300mg/50ml OD Levofloxacin Levaquin 500mg OD IV Doripenem Doribax 500mg OD