Git.pptx
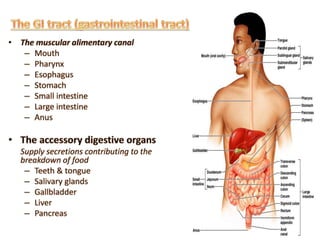
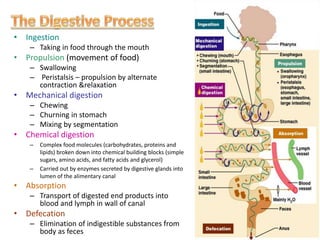
- 3. ŌĆó Ingestion ŌĆō Taking in food through the mouth ŌĆó Propulsion (movement of food) ŌĆō Swallowing ŌĆō Peristalsis ŌĆō propulsion by alternate contraction &relaxation ŌĆó Mechanical digestion ŌĆō Chewing ŌĆō Churning in stomach ŌĆō Mixing by segmentation ŌĆó Chemical digestion ŌĆō Complex food molecules (carbohydrates, proteins and lipids) broken down into chemical building blocks (simple sugars, amino acids, and fatty acids and glycerol) ŌĆō Carried out by enzymes secreted by digestive glands into lumen of the alimentary canal ŌĆó Absorption ŌĆō Transport of digested end products into blood and lymph in wall of canal ŌĆó Defecation ŌĆō Elimination of indigestible substances from body as feces
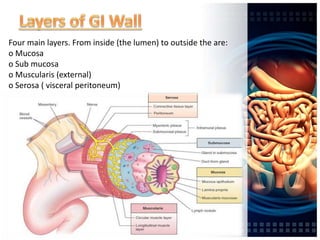
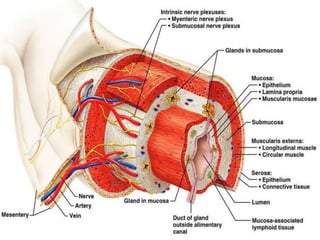
- 4. Four main layers. From inside (the lumen) to outside the are: o Mucosa o Sub mucosa o Muscularis (external) o Serosa ( visceral peritoneum)
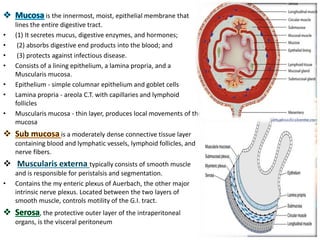
- 5. is the innermost, moist, epithelial membrane that lines the entire digestive tract. ŌĆó (1) It secretes mucus, digestive enzymes, and hormones; ŌĆó (2) absorbs digestive end products into the blood; and ŌĆó (3) protects against infectious disease. ŌĆó Consists of a lining epithelium, a lamina propria, and a Muscularis mucosa. ŌĆó Epithelium - simple columnar epithelium and goblet cells ŌĆó Lamina propria - areola C.T. with capillaries and lymphoid follicles ŌĆó Muscularis mucosa - thin layer, produces local movements of the mucosa is a moderately dense connective tissue layer containing blood and lymphatic vessels, lymphoid follicles, and nerve fibers. ’üČ typically consists of smooth muscle and is responsible for peristalsis and segmentation. ŌĆó Contains the my enteric plexus of Auerbach, the other major intrinsic nerve plexus. Located between the two layers of smooth muscle, controls motility of the G.I. tract. , the protective outer layer of the intraperitoneal organs, is the visceral peritoneum
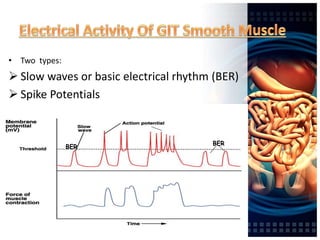
- 7. ŌĆó Two types: ’āś Slow waves or basic electrical rhythm (BER) ’āś Spike Potentials BER BER
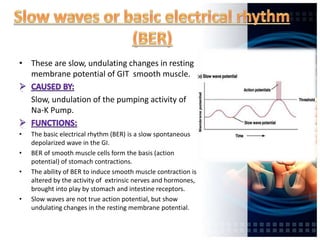
- 8. ŌĆó These are slow, undulating changes in resting membrane potential of GIT smooth muscle. Slow, undulation of the pumping activity of Na-K Pump. ŌĆó The basic electrical rhythm (BER) is a slow spontaneous depolarized wave in the GI. ŌĆó BER of smooth muscle cells form the basis (action potential) of stomach contractions. ŌĆó The ability of BER to induce smooth muscle contraction is altered by the activity of extrinsic nerves and hormones, brought into play by stomach and intestine receptors. ŌĆó Slow waves are not true action potential, but show undulating changes in the resting membrane potential.
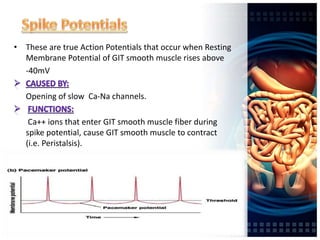
- 9. ŌĆó These are true Action Potentials that occur when Resting Membrane Potential of GIT smooth muscle rises above -40mV Opening of slow Ca-Na channels. Ca++ ions that enter GIT smooth muscle fiber during spike potential, cause GIT smooth muscle to contract (i.e. Peristalsis).
- 10. ’üČ Under normal conditions, the resting membrane potential averages about -56 mill volts, but multiple factors can change this level. When the potential becomes less negative, which is called depolarization of the membrane, the muscle fibers become more excitable. When the potential becomes more negative, which is called hyper polarization, the fibers become less excitable.
- 11. ŌĆó (1) stretching of the muscle, ŌĆó (2) stimulation by acetylcholine, ŌĆó (3) stimulation by parasympathetic nerves that secrete acetylcholine at their endings, and ŌĆó (4) stimulation by several specific gastrointestinal hormones. ŌĆó (1) the effect of nor epinephrine or epinephrine on the fiber membrane and ŌĆó (2) stimulation of the sympathetic nerves that secrete mainly nor epinephrine at their endings.
- 12. ŌĆó Smooth muscle contraction occurs in response to entry of calcium ions into the muscle fiber. Calcium ions, acting through a calmodulin control mechanism, activate the myosin filaments in the fiber, causing attractive forces to develop between the myosin filaments and the actin filaments, thereby causing the muscle to contract. ŌĆó The slow waves do not cause calcium ions to enter the smooth muscle fiber (only sodium ions). Therefore, the slow waves by themselves usually cause no muscle contraction. Instead, it is during the spike potentials, generated at the peaks of the slow waves, that significant quantities of calcium ions do enter the fibers and cause most of the contraction.
- 13. ŌĆó Some smooth muscle of the gastrointestinal tract exhibits tonic contraction as well as or instead of rhythmical contractions. ’āś Tonic contraction is continuous, not associated with the basic electrical rhythm of the slow waves but often lasting several minutes or even hours. The tonic contraction often increases or decreases in intensity. ’āś Tonic contractions (continued)- Caused by: ’üČ Continuous repetitive spike potential ’üČ Hormonal effects ’üČ Continuous entry of Ca
- 14. 1. Enteric Nervous System 2. Autonomic Nervous System 3. Sensory Nervous System
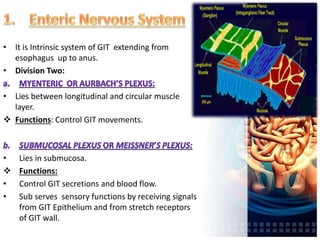
- 15. ŌĆó It is Intrinsic system of GIT extending from esophagus up to anus. ŌĆó Division Two: ŌĆó Lies between longitudinal and circular muscle layer. ’üČ Functions: Control GIT movements. ŌĆó Lies in submucosa. ’üČ Functions: ŌĆó Control GIT secretions and blood flow. ŌĆó Sub serves sensory functions by receiving signals from GIT Epithelium and from stretch receptors of GIT wall.
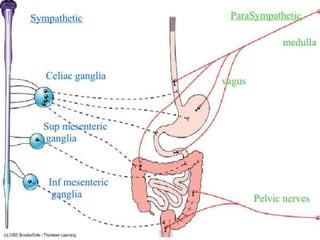
- 16. ŌĆó Activity is control by sympathetic and parasympathetic nervous system. Vagus Nerve innervates GIT from esophagus up to proximal 2/3 of transverse colon. Pelvic Parasympathetic Nerve:(S2-S4)Innervates GIT from distal 1/3 of transverse colon. Increase peristalsis and tone. Relaxes Sphincters. Increase digestive secretions.
- 18. : ŌĆó Preganglionic sympathetic originate in T5 TO L2 segment of spinal cord, Pass thru sympathetic chain, synapse with ŌĆó post ganglionic neuron in celiac and mesenteric and hypo gastric ganglia. Postganglionic fibers innervates in GIT. ŌĆó Decrease peristalsis and tone ŌĆó Contract sphincters ŌĆó Decrease digestive secretion
- 19. ’āś Sensory nerve endings originate in the gastrointestinal epithelium or gut wall and send afferent fibers to both plexuses of the enteric system, as well as (1) to the prevertebral ganglia of the sympathetic nervous system, (2) to the spinal cord, and (3) in the Vagus nerves all the way to the brain stem. ’āś These sensory nerves can elicit local reflexes within the gut wall itself and still other reflexes that are relayed to the gut from either the prevertebral ganglia or the basal regions of the brain.
- 20. ŌĆó Two types of movements occur in the gastrointestinal tract: 1. Mixing movements: ( Segmentation Contraction) 2. Propulsive movements: (Peristalsis)
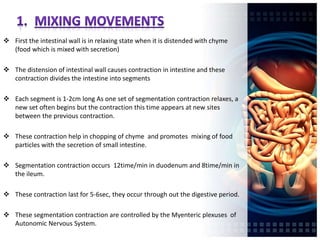
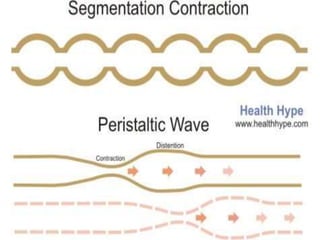
- 21. ’üČ First the intestinal wall is in relaxing state when it is distended with chyme (food which is mixed with secretion) ’üČ The distension of intestinal wall causes contraction in intestine and these contraction divides the intestine into segments ’üČ Each segment is 1-2cm long As one set of segmentation contraction relaxes, a new set often begins but the contraction this time appears at new sites between the previous contraction. ’üČ These contraction help in chopping of chyme and promotes mixing of food particles with the secretion of small intestine. ’üČ Segmentation contraction occurs 12time/min in duodenum and 8time/min in the ileum. ’üČ These contraction last for 5-6sec, they occur through out the digestive period. ’üČ These segmentation contraction are controlled by the Myenteric plexuses of Autonomic Nervous System.
- 23. ’āś Chyme is propelled or pushed through small intestine by peristaltic waves. ’āś These waves are produced and response to stretch .This is called Myenteric Reflex. ’āś They occur in any part of small intestine and move at a velocity of 0.2-2cm/sec. They usually dies off after travel this distance. ’āś From here it starts a new peristalsis state and move a chyme in forward direction, thus several peristaltic waves occur one after the other and push the small intestine contents at the distal end of the small intestine. ’āś Therefore due to the slow movement of peristalsis waves usually 3-5hours are required for passage of chyme from pyrolysis to the ileocecal valve. ’āś These peristaltic wave don't occur alone but are superimposed upon segmental movement of small intestine. Thus both segmental and peristalsis movements occurs simultaneously.