SUTURING.ppt
- 1. Suturing
- 2. • Suture:- any thread or strand which brings the opposite surfaces together • Purpose: – To replace the tissue layers and wound edges in passive approximation assisting in healing. – To limit the size of wound and therefore reduce the chances of contamination and infection
- 3. Classification of sutures • Absorbable and non absorbable • Polyfilamentous and monofilametous • Synthetic and natural • Coated and uncoated
- 4. • Absorbable suture materials include the original catgut as well as the newer synthetics polyglycolic acid , polylactic acid, polydioxanone, and caprolactone. • They are broken down by various processes including hydrolysis (polyglycolic acid) and proteolytic enzymatic degradation. • Depending on the material, the process can be from ten days to eight weeks. • They are used in patients who cannot return for suture removal, or in internal body tissues. • In both cases, they will hold the body tissues together long enough to allow healing, but will disintegrate so that they do not leave foreign material or require further procedures. • Occasionally, absorbable sutures can cause inflammation and be rejected by the body rather than absorbed.
- 5. • Non-absorbable sutures are made of special silk or the synthetics polypropylene, polyester or nylon. • Stainless steel wires are commonly used in orthopedic surgery and for sternal closure in cardiac surgery. • These may or may not have coatings to enhance their performance characteristics. • Non-absorbable sutures are used either on skin wound closure, where the sutures can be removed after a few weeks, or in stressful internal environments where absorbable sutures will not suffice. • Non-absorbable sutures often cause less scarring because they provoke less immune response, and thus are used where cosmetic outcome is important. • They must be removed after a certain time, or left permanently.
- 6. • Catgut (rarely used now) – Derived from sheep intestinal mucosa – Poor tensile strength – Poor knot security – Quickly absorbed within 4-5 days – High tissue reactivity (absorbed by proteolysis) • Chromic acid treated catgut (Mild Chromic Gut) – Tensile strength more than that of cat gut – Moderate tissue reactivity (absorbed by proteolysis) – Poor knot security
- 7. • Polyglycolide or Polyglycolic acid (PGA) is a biodegradable, thermoplastic polymer and the simplest linear, aliphatic polyester. • It can be prepared starting from glycolic acid by means of poly-condensation or ring-opening polymerization. • PGA has been known since 1954 as a tough fiber- forming polymer. • Owing to its hydrolytic instability, however, its use has initially been limited. • Currently polyglycolide and its copolymers(poly-lactic- co-glycolic acid) with lactic acid, poly(glycolide-co- caprolactone) with ε-caprolactone, and poly (glycolide- co-trimethylene carbonate) with trimethylene carbonate) are widely used as a material for the synthesis of absorbable sutures and are being evaluated in the biomedical field.
- 8. Degradation • Polyglycolide is characterized by hydrolytic instability owing to the presence of the ester linkage in its backbone. • The degradation process is erosive and appears to take place in two steps during which the polymer is converted back to its monomer glycolic acid: first water diffuses into the amorphous (non-crystalline) regions of the polymer matrix, cleaving the ester bonds; the second step starts after the amorphous regions have been eroded, leaving the crystalline portion of the polymer susceptible to hydrolytic attack • Upon collapse of the crystalline regions the polymer chain dissolves.
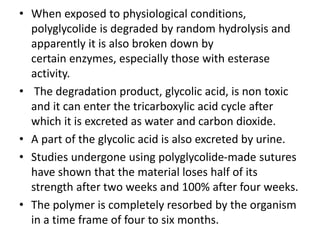
- 9. • When exposed to physiological conditions, polyglycolide is degraded by random hydrolysis and apparently it is also broken down by certain enzymes, especially those with esterase activity. • The degradation product, glycolic acid, is non toxic and it can enter the tricarboxylic acid cycle after which it is excreted as water and carbon dioxide. • A part of the glycolic acid is also excreted by urine. • Studies undergone using polyglycolide-made sutures have shown that the material loses half of its strength after two weeks and 100% after four weeks. • The polymer is completely resorbed by the organism in a time frame of four to six months.
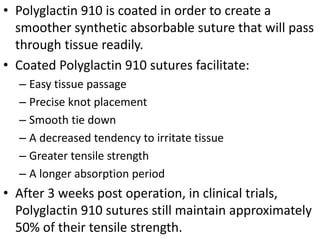
- 10. • Polyglactin 910 is coated in order to create a smoother synthetic absorbable suture that will pass through tissue readily. • Coated Polyglactin 910 sutures facilitate: – Easy tissue passage – Precise knot placement – Smooth tie down – A decreased tendency to irritate tissue – Greater tensile strength – A longer absorption period • After 3 weeks post operation, in clinical trials, Polyglactin 910 sutures still maintain approximately 50% of their tensile strength.
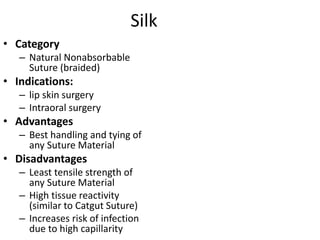
- 11. Silk • Category – Natural Nonabsorbable Suture (braided) • Indications: – lip skin surgery – Intraoral surgery • Advantages – Best handling and tying of any Suture Material • Disadvantages – Least tensile strength of any Suture Material – High tissue reactivity (similar to Catgut Suture) – Increases risk of infection due to high capillarity
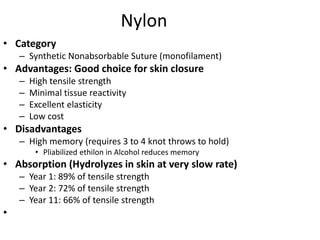
- 12. Nylon • Category – Synthetic Nonabsorbable Suture (monofilament) • Advantages: Good choice for skin closure – High tensile strength – Minimal tissue reactivity – Excellent elasticity – Low cost • Disadvantages – High memory (requires 3 to 4 knot throws to hold) • Pliabilized ethilon in Alcohol reduces memory • Absorption (Hydrolyzes in skin at very slow rate) – Year 1: 89% of tensile strength – Year 2: 72% of tensile strength – Year 11: 66% of tensile strength •
- 13. • Prolene is a synthetic, monofilament, nonabsorbable polypropylene suture. • It is indicated for skin closure and general soft tissue approximation and ligation. • Its advantages include high tensile strength, minimal tissue reactivity, and slipperiness (allowing easy removal from tissues). • Disadvantages include high plasticity, high expense, and difficulty of use compared to standard nylon sutures. • A ball-and-stick model of polypropylene. • Composed of an isotactic crystalline stereoisomer of polypropylene, Prolene sutures are intended to be durable and long lasting. • They are dyed blue, allowing for easy visibility against skin and when operating. • It is composed of a single filament. • A polypropylene mesh is also marketed under the name Prolene by Ethicon. • It is used for repairing hernias and other injuries to the fascia.
- 15. Needles • Traumatic needles are needles with holes or eyes which are supplied to the hospital separate from their suture thread. • The suture must be threaded on site, as is done when sewing at home. • Atraumatic needles with sutures comprise an eyeless needle attached to a specific length of suture thread. • The suture manufacturer swages the suture thread to the eyeless atraumatic needle at the factory. • There are several advantages to having the needle pre-mounted on the suture. • The doctor or the nurse or odp does not have to spend time threading the suture on the needle. • More importantly, the suture end of a swaged needle is smaller than the needle body. • In traumatic needles with eyes, the thread comes out of the needle's hole on both sides. • When passing through the tissues, this type of suture rips the tissue to a certain extent, thus the name traumatic • . Nearly all modern sutures feature swaged atraumatic needles.
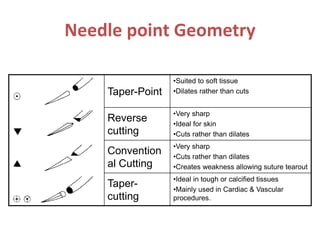
- 16. Needle point Geometry Taper-Point •Suited to soft tissue •Dilates rather than cuts Reverse cutting •Very sharp •Ideal for skin •Cuts rather than dilates Convention al Cutting •Very sharp •Cuts rather than dilates •Creates weakness allowing suture tearout Taper- cutting •Ideal in tough or calcified tissues •Mainly used in Cardiac & Vascular procedures.
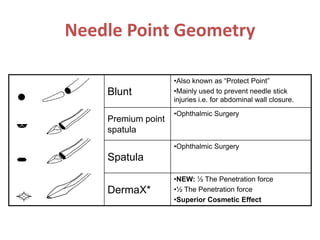
- 17. Needle Point Geometry Blunt •Also known as “Protect Point” •Mainly used to prevent needle stick injuries i.e. for abdominal wall closure. Premium point spatula •Ophthalmic Surgery Spatula •Ophthalmic Surgery DermaX* •NEW: ½ The Penetration force •½ The Penetration force •Superior Cosmetic Effect
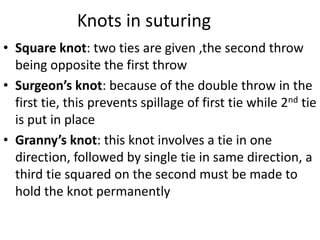
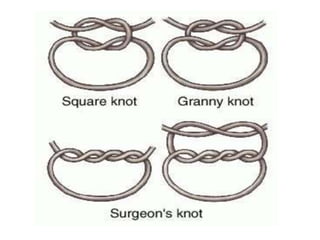
- 19. Knots in suturing • Square knot: two ties are given ,the second throw being opposite the first throw • Surgeon’s knot: because of the double throw in the first tie, this prevents spillage of first tie while 2nd tie is put in place • Granny’s knot: this knot involves a tie in one direction, followed by single tie in same direction, a third tie squared on the second must be made to hold the knot permanently
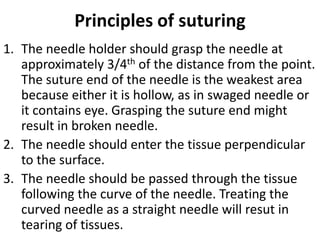
- 21. Principles of suturing 1. The needle holder should grasp the needle at approximately 3/4th of the distance from the point. The suture end of the needle is the weakest area because either it is hollow, as in swaged needle or it contains eye. Grasping the suture end might result in broken needle. 2. The needle should enter the tissue perpendicular to the surface. 3. The needle should be passed through the tissue following the curve of the needle. Treating the curved needle as a straight needle will resut in tearing of tissues.
- 22. 4. The suture should be placed equidistance from the incision on both sides at an equal depth. However in cases where tissue edges to be sutured at different levels, passage of suture closer to the edge of lower side and farther from edge of higher side will tend to approximate the levels. Another method involves passage of the suture at an equal distance from wound margins on both sides but deeper into the tissue on the lower side and more superficially on higher side. 5. If one tissue is free and other is fixed then the needle should pass from free to fixed side. 6. If one tissue side is thinner than the other the needle should be passed from thinner to thicker side
- 23. 7. If one tissue plane is deeper than the other then the needle should pass fromdeeper to superficial side. 8. The distance that needle is passed into the tissues should be greater than the distance from the tissue edge. This will ensure a degree of tissue eversion which is desirable to counter scar contracture. 9. The tissue should not be closed under tension, since they will either tear or necrose around the suture. If tension is present the tissue layer should be undermined to relieve it. 10. The suture should be tied sa that tissue edged are merely approximated no blanched.
- 24. 11. The knot should not be placed over the incision line. 12. Suture should be placed approximately 3-4mm apart. If placed too closely they strangulate the tissue and interfere with escape of inflammatory exudates. Closer spaced sutures are indicated in areas of muscular activity such as tongue or areas of increased tension. 13. Sometimes extra tissue may be present on one side of incision and cause a dog ear formation during wound closure. Extending the length of incision to hide excess will produce an unsatisfactory result.
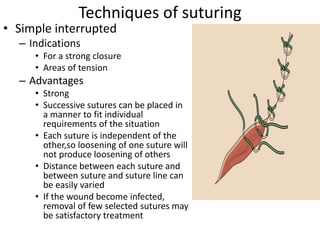
- 25. Techniques of suturing • Simple interrupted – Indications • For a strong closure • Areas of tension – Advantages • Strong • Successive sutures can be placed in a manner to fit individual requirements of the situation • Each suture is independent of the other,so loosening of one suture will not produce loosening of others • Distance between each suture and between suture and suture line can be easily varied • If the wound become infected, removal of few selected sutures may be satisfactory treatment
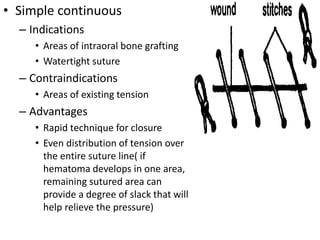
- 26. • Simple continuous – Indications • Areas of intraoral bone grafting • Watertight suture – Contraindications • Areas of existing tension – Advantages • Rapid technique for closure • Even distribution of tension over the entire suture line( if hematoma develops in one area, remaining sutured area can provide a degree of slack that will help relieve the pressure)
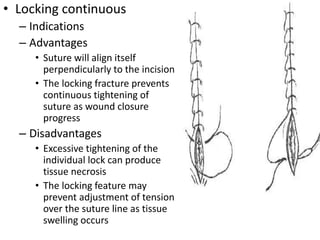
- 27. • Locking continuous – Indications – Advantages • Suture will align itself perpendicularly to the incision • The locking fracture prevents continuous tightening of suture as wound closure progress – Disadvantages • Excessive tightening of the individual lock can produce tissue necrosis • The locking feature may prevent adjustment of tension over the suture line as tissue swelling occurs
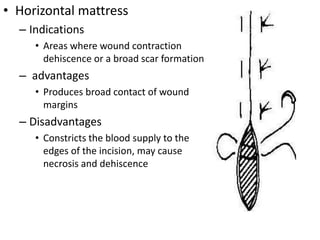
- 28. • Horizontal mattress – Indications • Areas where wound contraction dehiscence or a broad scar formation – advantages • Produces broad contact of wound margins – Disadvantages • Constricts the blood supply to the edges of the incision, may cause necrosis and dehiscence
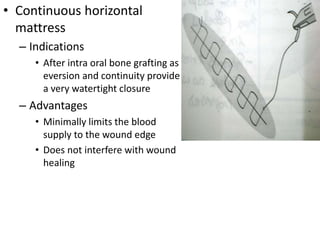
- 29. • Continuous horizontal mattress – Indications • After intra oral bone grafting as eversion and continuity provide a very watertight closure – Advantages • Minimally limits the blood supply to the wound edge • Does not interfere with wound healing
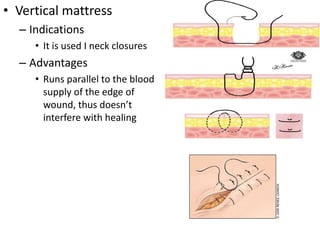
- 30. • Vertical mattress – Indications • It is used I neck closures – Advantages • Runs parallel to the blood supply of the edge of wound, thus doesn’t interfere with healing
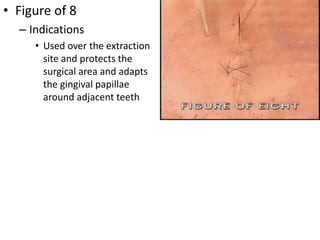
- 31. • Figure of 8 – Indications • Used over the extraction site and protects the surgical area and adapts the gingival papillae around adjacent teeth
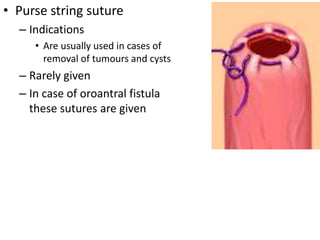
- 32. • Purse string suture – Indications • Are usually used in cases of removal of tumours and cysts – Rarely given – In case of oroantral fistula these sutures are given
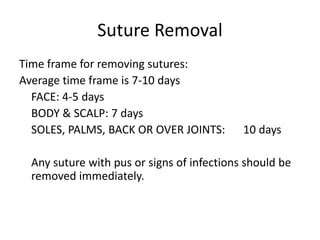
- 33. Suture Removal Time frame for removing sutures: Average time frame is 7-10 days FACE: 4-5 days BODY & SCALP: 7 days SOLES, PALMS, BACK OR OVER JOINTS: 10 days Any suture with pus or signs of infections should be removed immediately.
- 34. Suture Removal 1. Clean with hydrogen peroxide to remove any crusting or dried blood 2. Using the tweezers, grasp the knot and snip the suture below the knot, close to the skin 3. Pull the suture line through the tissue- in the direction that keeps the wound closed - and place on a 4x4
- 35. Suture Removal Once all sutures have been removed, count the sutures The number of sutures needs to match the number indicated in the patient's health record
- 36. Thank YOU