1. BLOOD Part 2.pptx
- 1. INTRODUCTION TO BLOOD DR LWIINDI
- 2. Section 2 Blood Cells and Hematoiesis ? Red blood cell ? White blood cell ? Platelet
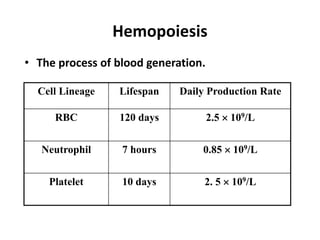
- 3. Hemopoiesis ? The process of blood generation. Cell Lineage Lifespan Daily Production Rate RBC 120 days 2.5 ? 109/L Neutrophil 7 hours 0.85 ? 109/L Platelet 10 days 2. 5 ? 109/L
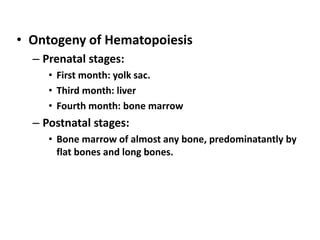
- 4. ? Ontogeny of Hematopoiesis ĻC Prenatal stages: ? First month: yolk sac. ? Third month: liver ? Fourth month: bone marrow ĻC Postnatal stages: ? Bone marrow of almost any bone, predominatantly by flat bones and long bones.
- 5. 0 2 3 4 5 6 7 8 9 1 100 100 birth 20 30 40 50 60 70 80 90 10 100 100 Yolk Sac Liver Bone morrow Spleen Lymph nodes Prenatal age (months) Postnatal age (years) Tibia Femur Ribs Sternum Vertebrate Hemopoitic activity (%) Proportion of Red Morrow (%)
- 7. Hematopoiesis: the formation of blood cells ? Hematopoiesis is the process that generates blood cells of all lineages. ? Calculations based on the blood volume and the level and half-life of each type of blood cell in the circulation indicate that each day an adult produces ~ 200 billion erythrocytes, 100 billion leukocytes, and 100 billion platelets. ? These rates can increase by a factor of 10 or more when the demand for blood cells increases
- 11. Growth and differentiation inducers (cytokines, hormones) for the formation of blood cells Ą ? Interleukin-3 (IL-3) promotes growth of most of the different types of stem cells ? Interleukin-7 (IL-7) - major cytokine in stimulating bone marrow stem cells to start down the path leading to the various lymphocytes (mostly B cells and T cells). ? Erythropoietin (EPO), produced by the kidneys, enhances the production of red blood cells ? Thrombopoietin (TPO/ megakaryocyte growth and development factor), assisted by Interleukin-11 (IL- 11), stimulates the production of megakaryocytes. Their fragmentation produces platelets.
- 12. ? Granulocyte-monocyte colony-stimulating factor (GM-CSF), as its name suggests, sends cells down the path leading to both those cell types. In due course, one path or the other is taken. ? - Under the influence of granulocyte colony- stimulating factor (GCSF), they differentiate into neutrophils. ? - Further stimulated by interleukin-5 (IL-5) they develop into eosinophils. ? - Stimulated by macrophage colony-stimulating factor (M-CSF) the granulocyte/macrophage progenitor cells differentiate into monocytes, the precursors of macrophages.
- 13. ERYTHROPOIESIS ? process of the origin, development and maturation of erythrocytes ? important changes occur: ĻC Decrease in RBC size (25 to 7.2um) ĻC Disappearance of nucleoli and nucleus ĻC Appearance of hemoglobin and change in staining properties ĻC Formation of biconcave disc shape
- 14. ERYTHROPOIESIS
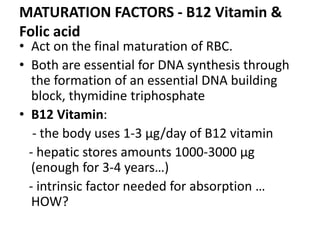
- 15. ERYTHROPOIESIS ? Factors necessary for hematopoiesis ĻC General stimulants ? Erythropoietin; Thyroxine; Other Hematopoietic growth factors; Vitamins (B, C, D, E) ĻC Maturations Factors ? B12 and Folic Acid. ĻC Substrates for Hb synthesis ? Amino acids, Iron, other minerals.
- 16. MATURATION FACTORS - B12 Vitamin & Folic acid ? Act on the final maturation of RBC. ? Both are essential for DNA synthesis through the formation of an essential DNA building block, thymidine triphosphate ? B12 Vitamin: - the body uses 1-3 ĶĖg/day of B12 vitamin - hepatic stores amounts 1000-3000 ĶĖg (enough for 3-4 yearsĄ) - intrinsic factor needed for absorption Ą HOW?
- 17. ? Vit. B12 & folic acid deficiency >> proliferation & maturation failure: - macrocytes (large, oval, fragile)> short life causes: ? atrophic gastric mucosa>> intrinsic factor deficiency> no B12 absorption (pernicious anemia) ? Dietary deficiency (who?) ? Ileal resection
- 18. Erythropoietin ? Glycoprotein, MW = 34.000, T1/2 = 6 - 9 hours ? Mechanism of action: Ąü the committment of stem cells to proerythroblasts Ąü the differentiation of erythroblastic stages ? Synthesized - 90% kidneys (renal tubular* epithelial cells?), the rest of 10% formed mainly in the liver ? - stimulus = renal hypoxia Ąü in EPO conc. after minutes to hours, with a maximum level after 24 h Ąü after 3 - 5 days: Ąü RBC number. 10 x ? - other non-renal hypoxia sensors act through E, NE, PG (+) EPO production
- 20. ? Regulation of erythropoietin control mechanismĄ ? Therapeutically used: 50 ĻC 300 U / kg, 3 times / week ? in kidneys diseases, transplant, anemia, pulmonary diseases, blood lossĄ
- 21. RED BLOOD CELLS
- 22. RED CELL COUNT ? Age It is higher in the newborn. ? Sex Cell count is relatively less in females ? Exercise During muscular exercise there is a slight temporary elevation of cell count. ? Diural variation It is slightly reduced during sleep. ? Altitude At higher altitudes the count is increased due to hypoxic state, which stimulates cell production. ? Emotional state There is increased secretion of adrenaline during excitement which increases the erythrocyte count.
- 23. ? Normal erythrocytes have a mean diameter of 7.2 microns and an average thickness of 2.2 microns. They contain about 65% water and the rest is made up of solid substances, out of which the haemoglobin constitutes 33%. ? Functions The main function of red blood cell is to transport oxygen and carbon dioxide. ? Life period The average life of an RBC is 120days. The old cells are destroyed in the spleen and liver. ? The physiological rise in RBC count is called polycythaemia. This can be observed in high altitudes.
- 24. ? Polycythaemia vera indicates the pathological condition of raised RBC count, which is seen in malignant condition of the red bone marrow. ? A decreased red cell count or subnormal haemoglobin level, when present is called anaemia.
- 25. HAEMOGLOBIN ? It is a chromoprotein and is red in color. Hb consists of a protein component globin and an iron containing pigment haem (porphyrin ring + iron) ? Iron exists in the ferrous form and each molecule of haemoglobin contains four iron atoms. Hb combines with the oxygen to form a loose reversible compound oxy-haemoglobin, which rapidly dissociates in the tissues to release oxygen. ? The formation and subsequent breakdown of oxyhaemoglobin is influenced by various factors which would be discussed later on in the chapter of respiration.
- 27. Hemoglobin Functions: ? Transports O2 ? Transports CO2 ? Acid-base Buffer
- 28. Hemoglobin ? Haemoglobin content of the blood ranges between 14 to 18 gm% and can be determined by haemoglobinometer. WHY??
- 29. Types Of Haemoglobin ? Normal HB ĻC HbA (ĶÁ2ĶÂ2); HbF (ĶÁ2ĶÃ2) ? Hemoglobinopathies ĻC HbS ĻC Thalassemias ? ĶÁ ? ĶĒ ? Abnormal derivates ĻC CarboxyHB (CO) ĻC MethHB (Fe3+)
- 30. Life Span of Red Cells and Fate of Haemoglobin ? The average life span of erythrocytes is 120 days. ? The cells are constantly broken down, primarily in the spleen and new cells are formed in the bone marrow. ? This helps to maintain a constant cell count. ? The fate of haemoglobin has been summarized below:
- 32. IRON METABOLISM ? The iron content of the body is about 4-5 mgm/kg of body weight. ? It is an essential constituent of haemoglobin, myoglobin, and respiratory enzymes and its main functions are the transport of oxygen to the tissues and cellular oxidative mechanism. ? The important sources of iron are liver, spleen, kidney and heart, but egg yolk, green leafy vegetables, nuts, dates and figs also contain iron in adequate quantities.
- 33. ? Absorption Normally very little of dietary iron (10%) is absorbed in the gastrointestinal tract. ? The organic ferric iron is converted into ferrous form by gastric acidity and iron absorption mainly occurs in the upper duodenum and depends upon the ferritin content of the intestinal mucosa. ? This is an iron-protein complex having 23% iron and a protein called apoferritin. ? This theory of absorption is known as Ą°mucosal block theoryĄą.
- 34. ? Transport, Utilization and Storage Iron combines with beta globulin and forms siderophilin or transferrin, which is the transport form of iron. ? In the tissues iron is released from siderophilin and it is utilized for the synthesis of haemoglobin, myoglobin and respiratory enzymes. ? Iron is stored in liver, spleen and intestinal mucosa. ? About 0.8% of the circulating RBC undergo disintegration daily and they liberate approximately 8gm, of haemoglobin which on degradation gives 25mgm of iron.
- 35. ? The bulk of it is used for the resynthesis of haemoglobin and the balance is stored. ? Excretion The efficiency of the utilization of the endogenous iron is high and only small quantities in the urine.
- 36. ANAEMIA ? It is due to the reduction of red blood cells or sub- normal level of haemoglobin which consequently affects the supply of oxygen to the tissues. ? Anaemia by itself is not a disease but a symptom of some underlying cause. ? Some of the common types of anaemia are: I. Nutritional anaemia due to a certain deficiency in the diet a. Pernicious anaemia due to Vit B12 deficiency . b. Megaloblastic anaemia due to lack of folic acid. c. Hypochromic anaemia as in iron deficiency.
- 37. II. Haemolytic anaemia resulting from excessive breakdown of RBC. It may be seen in the following conditions. a. Disease like malaria b. Sickle cell anaemia and thalassemia due to the presence of abnormal haemoglobin. III. Aplastic anaemia in which there is a suppression of bone marrow as in a. excessive use of certain drugs like sulpha drugs or chloramphenical. b. exposure to X-ray radiation. c. Malignant disease of the bone marrow.