2-General Examination of nursing MSS.pptx
- 1. General Examination of the Musculoskeletal System Prepared by Dr. Ruqaya Al-Kathiry Head of the Medical Department in UST Medicine is learned at the bedside and not in the classroomŌĆØ Sir William Osler (1849-1919)
- 3. Dynamic tests are difficult to describe in pictures & text so ask an experienced clinician to check your technique. Practise examining as many joints as possible to become familiar with NL appearances & ranges of movement. General Principles: Ask ŌĆō Look ŌĆō Feel ŌĆō Move ’é¦ After taking the Hx ŌåÆ observe, palpate & move. ’é¦ Always expose the joint above & below the one in question. ’é¦ Compare one limb with the opposite side. ’é¦ Examine the overall appearance for pallor, rash, skin tightening & hair changes. ’é¦ Look at the skin, SC tissues & bony outline of each area. ’é¦ Before palpating, ask the pt which area is painful or tender. ’é¦ Feel for warmth, swelling, stability & deformity. ’é¦ Assess if a deformity is reducible or fixed. ’é¦ Assess active before passive movement. Do not cause the pt additional pain. ’é¦ In suspected systemic dis, examine all joints and fully examine all systems. ’é¦ Use standard terminology to describe joint limb positions & movement. Always describe movements from the neutral position. Commonly used terms are: o Flexion: bending at a joint from the neutral position o Extension: straightening a joint back to the neutral position o Hyperextension: movement beyond the NL neutral position because of a torn lig. or underlying ligamentous laxity, e.g. Ehlers-Danlos $ PHYSICAL EXAMINATION
- 4. o Adduction: movement towards the midline of the body (finger adduction is movement towards the axis of the limb) o Abduction: movement away from the midline. ’é¦ Describe the position of a limb because of joint/bone deformity: o Valgus: the distal part deviates away from the midline o Varus: the distal part deviates towards the midline. Equipment: You need a: ŌĆó Tape measure ŌĆó Tendon hammer ŌĆó Goniometer (protractor for measuring the range of joint movement) ŌĆó Stethoscope ŌĆó Blocks for assessing leg length discrepancy General Examination: Skin, nail & soft tissue ABNL Findings: Skin & related struct. are the most common sites of ass. lesions. ŌĆó Psoriasis may be hidden (U, natal cleft, scalp). Nail changes: fine or coarse pits in nail, onycholysis, thickening and ridging. ŌĆó Rash of SLE is induced by UV light exposure.
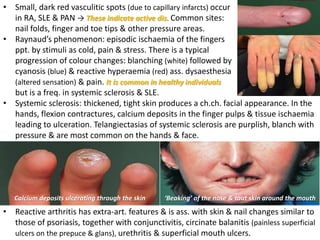
- 5. ŌĆó Small, dark red vasculitic spots (due to capillary infarcts) occur in RA, SLE & PAN ŌåÆ These indicate active dis. Common sites: nail folds, finger and toe tips & other pressure areas. ŌĆó RaynaudŌĆÖs phenomenon: episodic ischaemia of the fingers ppt. by stimuli as cold, pain & stress. There is a typical progression of colour changes: blanching (white) followed by cyanosis (blue) & reactive hyperaemia (red) ass. dysaesthesia (altered sensation) & pain. It is common in healthy individuals but is a freq. in systemic sclerosis & SLE. ŌĆó Systemic sclerosis: thickened, tight skin produces a ch.ch. facial appearance. In the hands, flexion contractures, calcium deposits in the finger pulps & tissue ischaemia leading to ulceration. Telangiectasias of systemic sclerosis are purplish, blanch with pressure & are most common on the hands & face. ŌĆśBeakingŌĆÖ of the nose & taut skin around the mouth Calcium deposits ulcerating through the skin ŌĆó Reactive arthritis has extra-art. features & is ass. with skin & nail changes similar to those of psoriasis, together with conjunctivitis, circinate balanitis (painless superficial ulcers on the prepuce & glans), urethritis & superficial mouth ulcers.
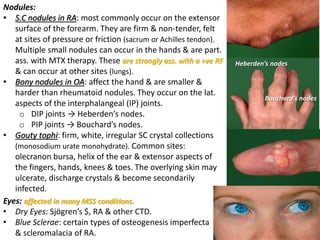
- 6. Nodules: ŌĆó S.C nodules in RA: most commonly occur on the extensor surface of the forearm. They are firm & non-tender, felt at sites of pressure or friction (sacrum or Achilles tendon). Multiple small nodules can occur in the hands & are part. ass. with MTX therapy. These are strongly ass. with a +ve RF & can occur at other sites (lungs). ŌĆó Bony nodules in OA: affect the hand & are smaller & harder than rheumatoid nodules. They occur on the lat. aspects of the interphalangeal (IP) joints. o DIP joints ŌåÆ HeberdenŌĆÖs nodes. o PIP joints ŌåÆ BouchardŌĆÖs nodes. ŌĆó Gouty tophi: firm, white, irregular SC crystal collections (monosodium urate monohydrate). Common sites: olecranon bursa, helix of the ear & extensor aspects of the fingers, hands, knees & toes. The overlying skin may ulcerate, discharge crystals & become secondarily infected. HeberdenŌĆÖs nodes BouchardŌĆÖs nodes Eyes: affected in many MSS conditions. ŌĆó Dry Eyes: Sj├ČgrenŌĆÖs $, RA & other CTD. ŌĆó Blue Sclerae: certain types of osteogenesis imperfecta & scleromalacia of RA.
- 7. General Features of Systemic Involvement: ŌĆó Wt loss, Muscle loss, Fever & LAP
- 8. Examination Sequence: Perform SchirmerŌĆÖs tear test to Dx keratoconjunctivitis sicca. Ō¢Ā Hook a small strip of notched blotting paper ~40 mm long over the lower eyelid while the pt looks upwards. The notch is ~5 mm from one end of the strip & is where the strip is bent over the eyelid. Ō¢Ā Ask the pt to close the eye. Ō¢Ā Wait for exactly 5mins, then remove the strip. Ō¢Ā Measure the distance that tears travel down the strip with a millimetre rule: >15mm = NL 5ŌĆō15 mm = equivocal <5 mm = ABNL ABNL findings ŌĆó Conjunctivitis ŌåÆ reactive arthritis. ŌĆó Ōåō tear production with ŌĆśdry eyesŌĆÖ (keratoconjunctivitis sicca) ŌåÆ conjunctivitis & blepharitis (inflam. of the eyelids) ŌåÆ Sj├ČgrenŌĆÖs $ & as 2ary changes in RA & other CTD. ŌĆó Scleritis & episcleritis ŌåÆ RA & psoriatic arthritis. ŌĆó Ant. uveitis (iritis) ŌåÆ ~25% of pts with ankylosing spondylitis & reactive arthritis but is asymp. in juvenile idiopathic arthritis (JIA), so ophthalmological assessment is essential if JIA is suspected. ŌĆó The sclerae are blue in certain types of osteogenesis imperfecta & in the scleromalacia of long-standing RA.
- 9. Medicine is learned at the bedside and not in the classroomŌĆØ Sir William Osler (1849-1919) THANK YOU FOR YOUR ATTENDANCE