2.plastic surgery
- 1. PLASTIC SURGERY Dr. Jalal Ali Hassan Plastic Surgeon 18th April 2013
- 2. PLASTIC SURGERY: Plastic surgery is defined as repair or reconstruction of lost, injured or deformed parts of the body chiefly by transfer of tissue. The term plastic concerns molding and reshaping of tissues and comes from the Greek Plasticos (that may be molded). The tissues are moved or reshaped by two fundamental methods (Grafts and Flaps). A Graft is a piece of tissue that is moved without its blood supply. A Flap is a piece of tissue that is moved maintaining its blood supply and is not reliant on the recipient site for its vascularity.
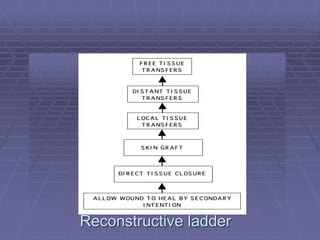
- 3. Priorities in reconstruction With any defect it is important to recognize that the most important priority is to achieve primary healing. The purpose of reconstructive procedures is to avoid the adverse consequences of healing by second intention in term of delay and poor function. If one can achieve quiet primary healing and thereby restore the patient to function superior result in terms of appearance will usually result. Where these aims cannot be achieved by direct closure of a wound a more complex technique is selected from the reconstructive ladder. Planning and selection are central to the practice of plastic surgery. Priorities in plastic surgery 1-Healing 2-Function 3-Cosmetic
- 5. SKIN GRAFT: Free grafts are tissues which are completely detached from the body before it is transplanted to other host bed. DONOR AREA RECIPIENT AREA. Free grafts commonly used in plastic surgery are: 1-Skin graft 2-Fat graft 3-Bone graft 4-Cartilage graft 5-Tendon graft 6-Nerve graft 7-Composite graft
- 6. Anatomy of SkinAnatomy of Skin SSGSSG FSGFSG
- 10. Donor site
- 11. Skin graft on electrical dermatome
- 12. Mesh machine
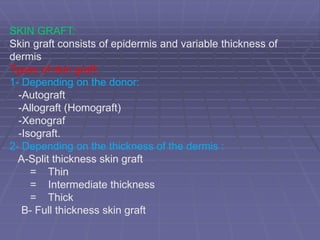
- 15. SKIN GRAFT: Skin graft consists of epidermis and variable thickness of dermis Types of skin graft: 1- Depending on the donor: -Autograft -Allograft (Homograft) -Xenograf -Isograft. 2- Depending on the thickness of the dermis : A-Split thickness skin graft = Thin = Intermediate thickness = Thick B- Full thickness skin graft
- 16. Cla ssifica tion : âĒAccording to their donor sites & thickness: Thin intermediate. Thick Xenograft AllograftAllograft
- 17. INDICATIONS OF SKIN GRAFT: 1-Skin loss: - Post âtraumatic - Post surgical - pathological process e.g venous ulcer - Extensive burn 2- Mucosal loss: - After excision of leukopakic patch in oral cavity - vaginal a genesis .
- 18. Contraindications: 1- Avascular recipient areas : - Cortical bone without periosteum - Cartilage without perichondrim - Tendon without paratenon BRIDGING PHENOMENON 2- Infection : a- heavily infected wound with copious discharge(100 000 bact./ gram of tissue). b- Infection by Beta haemolytic streptococcus
- 20. ï§ Causes of skin graft failure: 1. Haematoma (Most common) 2. Inadequate graft fixation; too tight or too loose. 3. Misjudgment of vascularity (poor bed) 4. Bacterial contamination( infection) 5. Technical error upside down graft 6. Dependent position of lower extremity
- 21. Clinical differences between healthy and unhealthy granulation tissue Healthy granulation Unhealthy granulation 1- Slough absent Present 2- Discharge Minimal, mainly serous Copious serosanguinous or Purulent 3- Color Pink or red Yellowish red 4- Surface Granular Glazed, slimy 5- Marginal epithelium Healthy and grows Unhealthy and does towards centre not grow towards centre 6- Skin grafting Support skin grafting can not support skin grafting 7- Odor no bad odor Bad odor
- 22. Healthy granulation tissue Unhealthy granulation tissue
- 23. Process of take: The process of revascularization and reattachment (fibrin anchorage) of skin graft to the recipient area is called TAKE of the graft. Factors influencing take of the graft: Various factors which influence the take of the graft are: 1- Graft factors: a- Thickness of the graft: b- Vascularity of donor area: c- Delay in application of harvested graft : d- Meshing.
- 24. 2- Graft bed factors : are a- Vascularity b- Infection : c- Necrotic tissue : d- Irradiated graft bed : 3- Environmental factors : a- Close contact: between graft and recipient bed b- Immobile contact : Any shearing force break the vascular link up. c- Inadequate venous and lymphatic drainage : 4- Immunogenic factors : Allograft and Xenograft induces a rejection reaction .
- 25. Sheet grafts: provide a superior aesthetic benefit and should always be used on the face and hands. Meshed grafts: Advantages: Disadvantages:
- 26. Meshed graft or sheet graft : Advantages Lager area Contours irregular surface Drain blood & exudates Increase edges_______reepithilialization Disadvantages Much of wound heal 2*______contracture Cobble stone appearance Sheet Graft Joint Hands face
- 30. Differences between split skin graft and full thickness skin graft Full thickness graft Split skin graft 1-Consists of epidermis and Thickness consists of epidermis Full thickness of dermis and variable thickness of dermis 2-Instruments: šÝšÝßĢ 31 3-Donor areas: šÝšÝßĢ 13 4-Donor area healing 5- Recipient area: 6-Graft contraction 7-Colour change 8- Resistance to trauma: 9- Hair growth