3. ABOUT COAGULANT AND ANTICOAGULANT.pptx
- 1. COAGULANTS & ANTICOAGULANTS Dr. Santosh Kumar Panda
- 2. COAGULANTS âĒ Haemostasis (arrest of blood loss) and blood coagulation involve complex interactions between the injured vessel wall, platelets and coagulation factors. âĒ These are substances which promote coagulation, and are indicated in haemorrhagic states. Fresh whole blood or plasma provide all the factors needed for coagulation and are the best therapy for deficiency of any clotting factor; also they act immediately. Other drugs used to restore haemostasis are: 1. Vitamin K âĒ K1 (from plants, fat-soluble) : Phytonadione (Phylloquinone) âĒ K3 (synthetic) âFat-soluble : Menadione, Acetomenaphthone âWater-soluble : Menadione sod. Bisulfate, Menadione Sod. diphosphate 2. Miscellaneous âĒ Fibrinogen (human) âĒ Antihaemophilic factor âĒ Desmopressin âĒ Adrenochrome monosemicarbazone âĒ Rutin, Ethamsylate
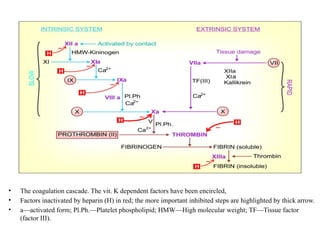
- 3. âĒ The coagulation cascade. The vit. K dependent factors have been encircled, âĒ Factors inactivated by heparin (H) in red; the more important inhibited steps are highlighted by thick arrow. âĒ aâactivated form; Pl.Ph.âPlatelet phospholipid; HMWâHigh molecular weight; TFâTissue factor (factor III).
- 4. VITAMIN K ï§ It is a fat-soluble dietary principle required for the synthesis of clotting factors. Action: ï§ Vit K acts as a cofactor at a late stage in the synthesis by liver of coagulation proteinsâ prothrombin, factors VII, IX and X. Utilization: ï§ Fat-soluble forms of vit K are absorbed from the intestine via lymph and require bile salts for absorption ï§ Water-soluble forms are absorbed directly into portal blood. ï§ An active transport process in the jejunum has been demonstrated for K1, while K2 and K3 are absorbed by simple diffusion.
- 5. DEFICIENCY: ï§ Deficiency of vit K occurs due to liver disease, obstructive jaundice, malabsorption, long-term antimicrobial therapy which alters intestinal flora. However, deficient diet is rarely responsible. The most important manifestation is bleeding tendency due to lowering of the levels of prothrombin and other clotting factors in blood. ï§ Haematuria is usually first to occur; other common sites of bleeding are g.i.t., nose and under the skin. USES: âĒ Dietary deficiency âĒ Prolonged antimicrobial therapy âĒ Obstructive jaundice âĒ Liver diseases âĒ New born âĒ Overdose of oral anticoagulants.
- 6. LOCAL HAEMOSTATICS âĒ External bleeding is usually stopped by manual pressure, cotton-gauze pressure pack or by suturing. âĒ Control of bleeding may be aided by local haemostatics (styptics) that are substances used to stop bleeding from a local and approachable site. They are particularly effective on oozing surfaces, e.g. tooth socket, abrasions, etc. âĒ Absorbable materials like fibrin (prepared from human plasma and dryed as sheet or foam), gelatin foam, oxidized cellulose (as strips which can be cut and placed in the wound) provide a meshwork which activates the clotting mechanism and checks bleeding. Left in situ these materials are absorbed in 1â4 weeks and generally cause no foreign body reaction. âĒ Thrombin obtained from bovine plasma may be applied as dry powder or freshly prepared solution to the bleeding surface in haemophiliacs. âĒ Vasoconstrictors like 0.1% Adr solution may be soaked in sterile cotton gauze and packed in the bleeding tooth socket or nose. âĒ Astringents such as tannic acid or metallic salts are occasionally applied for bleeding gums, bleeding piles etc.
- 7. ANTICOAGULANTS âĒ These are drugs used to reduce the coagulability of blood. They may be classified into: 1- Used in vivo A. Parenteral anticoagulants âĒ (i) Indirect thrombin inhibitors: Heparin, Low molecular weight heparins, Fondaparinux, Danaparoid âĒ (ii) Direct thrombin inhibitors: Lepirudin, Bivalirudin, Argatroban B. Oral anticoagulants âĒ (i) Coumarin derivatives: Bishydroxycoumarin (dicumarol), Warfarin sod, Acenocoumarol (Nicoumalone), âĒ (ii) Indandione derivative: Phenindione. âĒ (iii) Direct factor Xa inhibitors: Rivaroxaban âĒ (iv) Oral direct thrombin inhibitor: Dabigatran etexilate 2- Used in vitro âĒ A. Heparin: 150 U to prevent clotting of 100 ml blood. âĒ B. Calcium complexing agents: Sodium citrate- Sodium citrate: 1.65 g for 350 ml of blood; used to keep blood in the fluid state for transfusion; âĒ Sodium oxalate:10 mg for 1 ml blood, Sodium edetate: 2 mg for 1 ml blood- used in blood taken for investigations.
- 8. HEPARIN Heparin is a non-uniform mixture of straight chain mucopolysaccharides with MW 10,000 to 20,000. It contains polymers of two sulfated disaccharide units: D-glucosamine-Liduronic acid and D-glucosamine-Dglucuronic acid. ACTIONS: âĒ 1. Anticoagulant Heparin is a powerful and instantaneously acting anticoagulant, effective both in vivo and in vitro. It acts indirectly by activating plasma antithrombin III (AT III, a serine proteinase inhibitor). The heparin-AT III complex then binds to clotting factors of the intrinsic and common pathways (Xa, IIa, IXa, XIa, XIIa and XIIIa) and inactivates them, but not factor VIIa operative in the extrinsic pathway. âĒ 2. Antiplatelet Heparin in higher doses inhibits platelet aggregation and prolongs bleeding time. âĒ 3. Lipaemia clearing Injection of heparin clears turbid post-prandial lipaemic. ADVERSE EFFECTS: âĒ Bleeding due to overdoses âĒ Thrombocytopenia âĒ Reversible alopecia âĒ Osteoporosis âĒ Hypersensitivity reactions.
- 9. CONTRAINDICATIONS: âĒ 1. Bleeding disorders, history of heparin induced thrombocytopenia. âĒ 2. Severe hypertension (risk of cerebral haemorrhage), threatened abortion, piles, g.i. ulcers âĒ 3. Subacute bacterial endocarditis (risk of embolism), large malignancies (risk of bleeding) tuberculosis (risk of hemoptysis). âĒ 4. Ocular and neurosurgery, lumbar puncture. âĒ 5. Chronic alcoholics, cirrhosis, renal failure. âĒ 6. Aspirin and other antiplatelet drugs should be used very cautiously during heparin therapy. HEPARIN ANTAGONIST: âĒ Protamine sulfate: It is a strongly basic, low molecular weight protein obtained from the sperm of certain fish. Given i.v. it neutralises heparin weight for weight, i.e. 1 mg is needed for every 100 U of heparin.
- 10. ORALANTICOAGULANTS Action and mechanism: âĒ Warfarin and its congeners act as anticoagulants only in vivo, not in vitro. This is so because they act indirectly by interfering with the synthesis of vit K dependent clotting factors in liver. They apparently behave as competitive antagonists of vit K and lower the plasma levels of functional clotting factors in a dose-dependent manner. USE OF ANTICOAGULANTS: âĒ 1- Deep vein thrombosis (DVT) and pulmonary embolism (PE). âĒ 2- Myocardial infarction (MI). âĒ 3. Unstable angina. âĒ 4. Rheumatic heart disease; Atrial fibrillation (AF) âĒ 5. Cerebrovascular disease âĒ 6. Vascular surgery, prosthetic heart valves, retinal vessel thrombosis, extra corporeal circulation, haemodialysis.
- 11. THANK YOU