5. National PMTCT Module 3 Session 1 2014.ppt
- 1. Nov 2010 National Centre for AIDS and STD Control Module 3 Session 1 Option B+ : Life-long Antiretroviral Therapy (ART) for PMTCT
- 2. Nov 2010 National Centre for AIDS and STD Control Session 1 Objectives • Describe about the Option B+ ( life-long ARV therapy (ART) for Prevention of Mother to Child Transmission) along with its advantages. • List criteria for starting pregnant women and breastfeeding mothers on life-long ARV therapy (ART). • List the recommended ARV drugs for lifelong ART
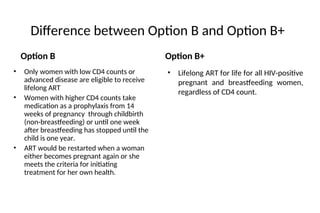
- 3. Difference between Option B and Option B+ Option B • Lifelong ART for life for all HIV-positive pregnant and breastfeeding women, regardless of CD4 count. Option B+ • Only women with low CD4 counts or advanced disease are eligible to receive lifelong ART • Women with higher CD4 counts take medication as a prophylaxis from 14 weeks of pregnancy through childbirth (non-breastfeeding) or until one week after breastfeeding has stopped until the child is one year. • ART would be restarted when a woman either becomes pregnant again or she meets the criteria for initiating treatment for her own health.
- 4. Nov 2010 National Centre for AIDS and STD Control Option B+ (Life-long ARV Therapy) • Option B+ provides all HIV-positive pregnant or breastfeeding women with antiretroviral drugs to prevent mother-to-child transmission. • A triple-drug regimen should be taken throughout pregnancy, delivery, breastfeeding and continue for life, regardless of CD4 count or clinical stage.
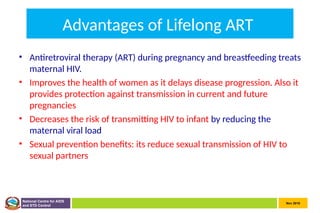
- 5. Nov 2010 National Centre for AIDS and STD Control Advantages of Lifelong ART • Antiretroviral therapy (ART) during pregnancy and breastfeeding treats maternal HIV. • Improves the health of women as it delays disease progression. Also it provides protection against transmission in current and future pregnancies • Decreases the risk of transmitting HIV to infant by reducing the maternal viral load • Sexual prevention benefits: its reduce sexual transmission of HIV to sexual partners
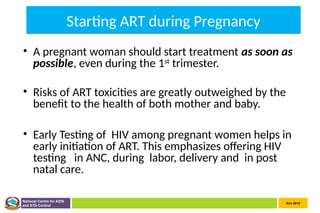
- 6. Nov 2010 National Centre for AIDS and STD Control Starting ART during Pregnancy • A pregnant woman should start treatment as soon as possible, even during the 1st trimester. • Risks of ART toxicities are greatly outweighed by the benefit to the health of both mother and baby. • Early Testing of HIV among pregnant women helps in early initiation of ART. This emphasizes offering HIV testing in ANC, during labor, delivery and in post natal care.
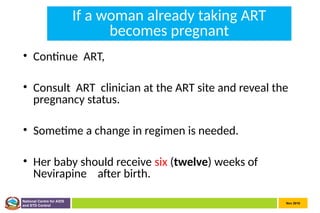
- 7. Nov 2010 National Centre for AIDS and STD Control If a woman already taking ART becomes pregnant • Continue ART, • Consult ART clinician at the ART site and reveal the pregnancy status. • Sometime a change in regimen is needed. • Her baby should receive six (twelve) weeks of Nevirapine after birth.
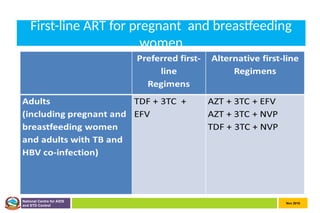
- 8. Nov 2010 National Centre for AIDS and STD Control First-line ART for pregnant and breastfeeding women
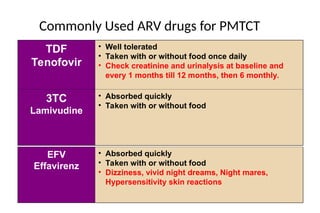
- 9. Commonly Used ARV drugs for PMTCT TDF Tenofovir • Well tolerated • Taken with or without food once daily • Check creatinine and urinalysis at baseline and every 1 months till 12 months, then 6 monthly. 3TC Lamivudine • Absorbed quickly • Taken with or without food EFV Effavirenz • Absorbed quickly • Taken with or without food • Dizziness, vivid night dreams, Night mares, Hypersensitivity skin reactions
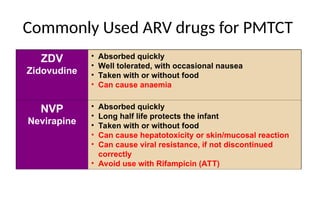
- 10. Commonly Used ARV drugs for PMTCT ZDV Zidovudine • Absorbed quickly • Well tolerated, with occasional nausea • Taken with or without food • Can cause anaemia NVP Nevirapine • Absorbed quickly • Long half life protects the infant • Taken with or without food • Can cause hepatotoxicity or skin/mucosal reaction • Can cause viral resistance, if not discontinued correctly • Avoid use with Rifampicin (ATT)
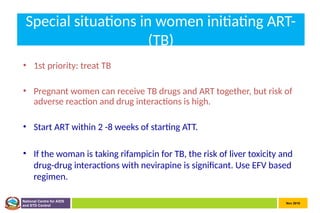
- 11. Nov 2010 National Centre for AIDS and STD Control Special situations in women initiating ART- (TB) • 1st priority: treat TB • Pregnant women can receive TB drugs and ART together, but risk of adverse reaction and drug interactions is high. • Start ART within 2 -8 weeks of starting ATT. • If the woman is taking rifampicin for TB, the risk of liver toxicity and drug-drug interactions with nevirapine is significant. Use EFV based regimen.
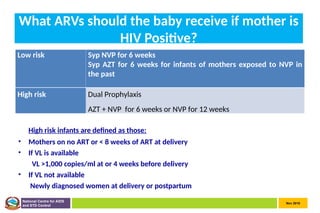
- 12. Nov 2010 National Centre for AIDS and STD Control What ARVs should the baby receive if mother is HIV Positive? High risk infants are defined as those: • Mothers on no ART or < 8 weeks of ART at delivery • If VL is available VL >1,000 copies/ml at or 4 weeks before delivery • If VL not available Newly diagnosed women at delivery or postpartum Low risk Syp NVP for 6 weeks Syp AZT for 6 weeks for infants of mothers exposed to NVP in the past High risk Dual Prophylaxis AZT + NVP for 6 weeks or NVP for 12 weeks
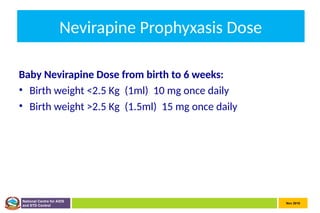
- 13. Nov 2010 National Centre for AIDS and STD Control Nevirapine Prophyxasis Dose Baby Nevirapine Dose from birth to 6 weeks: • Birth weight <2.5 Kg (1ml) 10 mg once daily • Birth weight >2.5 Kg (1.5ml) 15 mg once daily
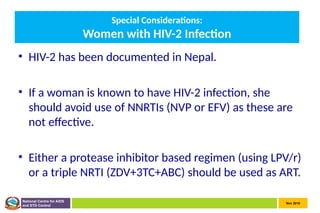
- 14. Nov 2010 National Centre for AIDS and STD Control Special Considerations: Women with HIV-2 Infection • HIV-2 has been documented in Nepal. • If a woman is known to have HIV-2 infection, she should avoid use of NNRTIs (NVP or EFV) as these are not effective. • Either a protease inhibitor based regimen (using LPV/r) or a triple NRTI (ZDV+3TC+ABC) should be used as ART.
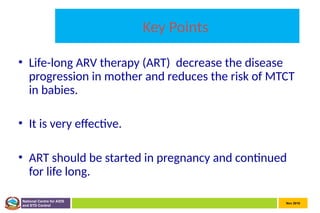
- 15. Nov 2010 National Centre for AIDS and STD Control Key Points • Life-long ARV therapy (ART) decrease the disease progression in mother and reduces the risk of MTCT in babies. • It is very effective. • ART should be started in pregnancy and continued for life long.
Editor's Notes
- #4: ARVs decrease the amount of virus in the mother’s blood, not only delays disease progression but also lowers chance of HIV transmission to her infant
- #8: Once-daily fixed – dose combination of TDF + 3TC + EFV is recommended as first line preferred ART in pregnant and breastfeeding women including pregnant women in the first trimester
- #12: For breastfeeding infants, available data suggest that maternal triple ARV prophylaxis started in pregnancy and continued during breastfeeding is efficacious in reducing HIV transmission and infant death. The panel placed a high value on providing an intervention that would allow safer breastfeeding practices for as long as the child is exposed to breast milk. The choice of 6 weeks for infant NVP prophylaxis relates to immunization visit timing and timing for early infant diagnosis. The helps to reduce the number of visits that the family must make to the health facility.