Abdominl Tuberculosis imaging features.pptx
- 1. IMAGING IN ABDOMINAL TUBERCULOSIS By Dr. Gayathri Moderator: Dr.Anjani
- 2. ŌĆó Tuberculosis can affect any organ system, particularly in immunocompromised individuals. ŌĆó It can be divided into 1) Pulmonary 2) Extrapulmonary. ŌĆó Lungs are the primary involved organs and abdominal involvement occurs in about 11-12% of patients with extra-pulmonary tuberculosis.
- 3. ŌĆó The abdominal presentation may involve different structures such as gastrointestinal tract, genitourinary tract, solid organs (liver, spleen, pancreas), gallbladder, aorta and its branches, peritoneum and lymph nodes, frequently with concomitant involvement of those organs
- 4. ETIOLOGY ŌĆó Primary infection from M. tuberculosis ŌĆó Abdominal TB is usually secondary to pulmonary TB ŌĆó CXR normal in 2/3 of patients with abdominal TB.Only 15% have active pulmonary disease . ŌĆó Other sources of abdominal infection with TB 1)Swallowing infected material. 2)Hematogenous spread from active or latent infection 3)Direct extension from infected tissues
- 5. CLINICAL FEATURES: Often presents with fever, weight loss, abdominal pain , anorexia, distension, lump, constipation and diarrhoea. Complications include obstruction, perforation, fistula formation and hemorrhage. May or may not have evidence of pulmonary TB Negative chest radiograph or negative tuberculin skin test does not exclude extrapulmonary TB
- 6. CLASSIFICATION OF ABDOMINAL TUBERCULOSIS a) Peritoneal tuberculosis b) Lymph node tuberculosis c) Gastrointestinal tuberculosis d) Tb of solid viscera
- 7. IMAGING FEATURES ŌĆó Often no evidence of lung disease (CXR or CT can be normal) LYMPHADENOPATHY (TUBERCULOUS LYMPHADENITIS) -Can range from increased number of normal-sized nodes to massively enlarged conglomerate nodal masses,Mesenteric and peripancreatic lymph nodes most commonly involved -Multiple groups often affected simultaneously -Enlarged, necrotic nodes with hypoattenuating centers and hyperattenuating enhancing rims on CT (40-60%)ŌĆōCharacteristic of caseous necrosis -Mixed-attenuation nodes are also possible -Nodes calcify with healing: TB probably most common cause of mesenteric nodal calcification
- 11. TUBERCULOSIS (TB) PERITONITIS : ŌĆó 3 imaging patterns: Wet, dry, and fibrotic fixed ŌĆó Wet type: Large amount of free or loculated ascites, which is usually complex with septations and fibrinous strands (and higher than water density due to protein/cellular content) ŌĆó Dry type: Mesenteric and omental thickening, fibrous adhesions, and caseous nodules ŌĆó Fibrotic fixed: Discrete masses in omentum with matted loops of bowel and frequent loculated ascites ŌŚŗDistinguishing TB peritonitis from carcinomatosis can be difficult, but carcinomatosis more likely to demonstrate discrete implants or omental caking (while peritoneum more often smoothly thickened in TB)
- 15. GI TB ŌĆó Ileocecal region affected in 90% of casesŌĆōCommon site due to presence of significant lymph tissue and stasis of bowel contents in that location (with close contact of bacilli with bowel mucosa) ŌĆó Cecum and terminal ileum are usually contracted (cone-shaped cecum) with asymmetric wall thickening of ileocecal valve and medial cecum and gaping ileocecal valve
- 16. ŌĆó Regional inflammation is common, but prominent vasa recta engorgement and increased vascularity associated with Crohn disease (also on differential diagnosis) not usually present ŌĆó Over time, cecum becomes gradually smaller and irregular in shape as result of scarring ŌĆó Regional lymphadenopathy with central caseation is frequent clue to correct diagnosis ŌŚŗ Involvement of stomach and proximal small bowel is rare, but any portion of GI tract can be involved ŌĆó Stomach: Often affects antrum and distal body, simulating peptic ulcer disease
- 17. The pathological forms of GI TB includes: ŌĆó Hypertrophic form (10 %) ŌĆó Ulcero ŌĆō proliferative form (30 %) ŌĆó Ulcerative form (60 %)
- 18. SIGNS ON BARIUM STUDY ŌĆó Fleischner sign ŌĆó Stierlin sign ŌĆó String sign ŌĆó Pulled up ceacum
- 21. PANCREATIC TB ŌĆó TB can very rarely manifest as mass, mimicking cancer (caseated peripancreatic nodes involving pancreas) ŌĆó Hypoenhancing mass (usually pancreatic head) typically without pancreatic duct dilatation or vascular invasion
- 23. RENAL TB ŌĆó Usually unilateral (75%) ŌĆó Earliest finding is papillary necrosis (usually involving upper pole), particularly evident on delayed excretory phase CT images or intravenous urography (uncommonly utilized in modern setting) ŌĆó Over time, fibrosis and stricturing of collecting system can lead to asymmetric caliectasis
- 24. ŌĆó Involvement of parenchyma can manifest as focal, wedge-shaped areas of low attenuation, multiple small, hypodense nodules, or discrete renal abscess ŌŚŗ In chronic stage, kidney appears atrophic and markedly irregular with cortical thinning, volume loss, and calcification (autonephrectomy or "putty" kidney) ŌĆó Kidney usually nonfunctional at this stage without contrast excretion
- 29. URETERAL TB ŌĆó Usually secondary to renal TB ŌĆó Filling defects may be seen in ureter on delayed excretory phase images due to sloughed papillae or debris secondary to renal infection/papillary necrosis ŌĆó Thickened ureteral wall with strictures most common in distal 1/3 of ureter ŌĆó Chronically can appear as corkscrew or beaded ureter due to multiple fibrotic strictures
- 31. URINARY BLADDER TB ŌĆó Tuberculous cystitis manifests as decreased bladder volume with wall thickening, ulceration, filling defects and calcifications in bladder wall ŌĆó Severe cases with profuse scarring result in small, irregular, and calcified bladder.
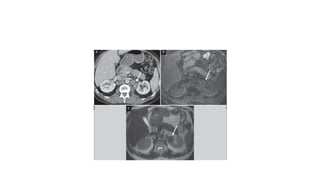
- 33. ADRENAL TB Acute: Enlarged adrenals (often appears as discrete, centrally necrotic adrenal mass) Chronic: Small adrenals with dots of calcification and low signal on all MR sequences
- 35. FEMALE GENITAL TB ŌĆó Most commonly involves fallopian tubes (in 94% of cases) and endometrium and can be cause of infertility ŌĆó Most often appears as bilateral hydrosalpinx (or pyosalpinx) with fallopian tubes appearing irregular and nodular (with sites of stenosis and scarring) ŌĆó Endometrium can appear thickened and heterogeneous with internal calcification and distorted shape as result of adhesions and scarring
- 37. MALE GENITAL TB ŌĆó Most often involves seminal vesicles or prostate gland with testicular involvement much less common ŌĆó Can resemble pyogenic abscess ┬▒ calcification ŌĆó TB prostatitis on prostate MR resembles other causes of prostatitis with band-like or geographic T2 hypointensity and mild restricted diffusion and mild early
- 39. HEPATIC AND SPLENIC TB ŌĆó Micronodular patternŌĆōInnumerable tiny nodules (< 2 mm), which are most often hypodense on CT and hyperechoic on USŌĆōMay simply appear as hepatomegaly/splenomegaly on CT (with individual lesions not visible) ŌĆó Macronodular patternŌĆōFewer large nodules, which frequently demonstrate central necrosisŌĆōHypodense on CT with ill-defined margins and gradual development of calcifications in more chronic stages ŌĆó TB and histoplasmosis are most common causes of calcified granulomasŌĆōT1 hypointense and T2 hyperintense on MR with rim enhancement
- 42. ŌĆóTHANK YOU