Abnormal labour.pptx
- 1. ABNORMAL LABOR DR.DEEPEKA.T.S.M.S(OBG)., MRCOG(U.K).,FELLOW IN REPRODUCTIVE MEDICINE SENIOR RESIDENT, DEPARTMENT OF OBSTETRICS AND GYNECOLOGY, SNIMS.
- 2. â—¦ DYSTOCIA â—¦ ABNORMALITIES OF THE EXPULSIVE FORCES â—¦ PREMATURELY RUPTURED MEMBRANES AT TERM â—¦ PRECIPITOUS LABOR AND DELIVERY â—¦ FETOPELVIC DISPROPORTION â—¦ FACE PRESENTATION â—¦ BROW PRESENTATION â—¦ TRANSVERSE LIE â—¦ COMPOUND PRESENTATION â—¦ COMPLICATIONS WITH DYSTOCIA
- 3. DYSTOCIA ◦ Dystocia literally means difficult labor and is characterized by abnormally slow labor progress. ◦ Causes are grouped into three distinct categories. Mechanistically, these simplify into abnormalities of the powers—poor uterine contractility and maternal expulsive effort; of the passenger—the fetus; and of the passage—the pelvis and lower reproductive tract. ◦ These three groups act singly or in combination to produce dysfunctional labor
- 4. Some Causes of Dystocia in Term Vertex Singletons
- 6. ABNORMALITIES OF THE EXPULSIVE FORCES Types of Uterine Dysfunction â—¦ Uterine contractions are needed to dilate the cervix and to expel the fetus. A contraction is initiated by spontaneous action potentials in the membrane of smooth muscle cells. Unlike the heart, a single pacemaker or its site remain unresolved (Young, 2018). â—¦ Resulting uterine contractions in normal labor show a rising and falling gradient of myometrial activity (Reynolds, 1951). â—¦ Normal spontaneous contractions can exert pressures approximating 60 mm Hg (Hendricks, 1959). Even so, the lower limit of contraction pressure required to dilate the cervix is 15 mm Hg (Caldeyro-Barcia, 1950).
- 7. â—¦ In abnormal labor, two physiological types of uterine dysfunction may develop. â—¦ In the more common hypotonic uterine dysfunction, basal tone is normal and uterine contractions have a normal gradient pattern (synchronous). However, pressure during a contraction is insufficient to dilate the cervix. â—¦ In the second type, hypertonic uterine dysfunction or incoordinate uterine dysfunction, either basal tone is elevated appreciably or the pressure gradient is distorted.
- 8. Risk Factors for Uterine Dysfunction â—¦ Neuraxial analgesia â—¦ Chorioamnionitis â—¦ A higher station at the onset of labor â—¦ maternal age â—¦ Maternal obesity l
- 9. Labor Disorders â—¦ Latent-phase Prolongation â—¦ Uterine dysfunction can in turn lead to labor abnormalities (Table 23-2).First, the latent phase may be prolonged, which is defined as >20 hours in the â—¦ nullipara and >14 hours in the multipara
- 11. PREMATURELY RUPTURED MEMBRANES AT TERM â—¦ Membrane rupture at term without spontaneous uterine contractions complicates approximately 8 percent of pregnancies. â—¦ labor induction with intravenous oxytocin was preferred management â—¦ In those with an unfavorable cervix, no or few contraction, and no significant fetal heart rate decelerations, prostaglandin E1 (misoprostol) is chosen to promote cervical ripening and contractions. â—¦ The benefit of prophylactic antibiotics in women with ruptured membranes before labor at term is unclear (Passos, 2012). â—¦ However, in those with membranes ruptured longer than 18 hours, antibiotics are instituted for group B streptococcal infection prophylaxis
- 12. PRECIPITOUS LABOR AND DELIVERY â—¦ Precipitous labor terminates in expulsion of the fetus in <3 hours. â—¦ Complications â—¦ uterine rupture or extensive lacerations of the cervix, vagina, vulva, or perineum â—¦ Amniotic fluid embolism â—¦ Uterine atony
- 13. â—¦ As treatment, analgesia is unlikely to modify these forceful contractions significantly. â—¦ The use of tocolytic agents such as magnesium sulfate or terbutaline is unproven in these circumstances. â—¦ A single, intramuscular 250-ug terbutaline dose may be reasonable in an attempt to resolve a nonreassuring fetal heart rate pattern. This is balanced against the risk of associated uterine atony if delivery is imminent. â—¦ Certainly, oxytocin administration should be stopped.
- 14. FETOPELVIC DISPROPORTION â—¦ Pelvic Capacity â—¦ Fetopelvic disproportion arises from diminished pelvic capacity or from abnormal fetal size, structure, presentation, or position. Commonly, both are present. â—¦ The pelvic inlet, midpelvis, or pelvic outlet may be contracted solely or in combination. Any contraction of the pelvic diameters that diminishes pelvic capacity can create dystocia.
- 15. Face Presentation â—¦ With this presentation, the neck is hyperextended so that the occiput is in contact with the fetal back, and the chin (mentum) is presenting. â—¦ The rate is approximately 0.1 percent of births
- 16. â—¦ During labor, fetal heart rate monitoring is best done with external devices to help avoid face or eye injury. â—¦ Because face presentations among term-size fetuses are more common with some degree of pelvic inlet contraction, cesarean delivery rates are substantially higher than with occiput presentation. â—¦ If indicated, low or outlet forceps delivery of a mentum anterior face presentation can be completed (Chap. 29, p. 542). Vacuum extraction has been associated with eye trauma and is not recommended
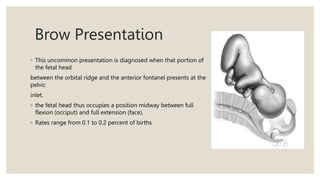
- 17. Brow Presentation â—¦ This uncommon presentation is diagnosed when that portion of the fetal head between the orbital ridge and the anterior fontanel presents at the pelvic inlet. â—¦ the fetal head thus occupies a position midway between full flexion (occiput) and full extension (face). â—¦ Rates range from 0.1 to 0.2 percent of births
- 18. â—¦ The presentation may be recognized by abdominal palpation when both the occiput and chin can be palpated easily, but vaginal examination is usually necessary. â—¦ The frontal sutures, large anterior fontanel, orbital ridges, eyes, and root of the nose are felt during vaginal examination, but neither the mouth nor the chin is palpable. â—¦ Except when the fetal head is small or the pelvis is unusually large, engagement of the fetal head and subsequent delivery cannot take place as long as the brow presentation persists.
- 19. Transverse Lie ◦ the fetus’ long axis lies approximately perpendicular to that of the ◦ mother. In a transverse lie, the shoulder is usually positioned over the pelvic ◦ inlet. The head occupies one iliac fossa, and the breech the other. This ◦ creates a shoulder presentation in which the side of the mother on which the ◦ acromion rests determines the designation of the position as right or left ◦ acromial. In addition, the back may be directed anteriorly or posteriorly and ◦ also superiorly or inferiorly. Thus, it is customary to further distinguish right ◦ or left varieties as dorsoanterior and dorsoposterior
- 20. Umbilical Cord Prolapse â—¦ umbilical cord prolapse may be more common with pelvis contraction. â—¦ Most risks stem from an unengaged presenting part and include hydramnios, breech presentation, transverse lie, premature or small fetus with weight <2500 g, preterm rupture of membranes, and multifetal gestation
- 21. â—¦ Umbilical cord prolapse is usually diagnosed clinically. â—¦ The cord loop is palpated in a position lower in the vaginal canal than the head or beside it. â—¦ For most cases, prompt manual elevation of the fetal head relieves cord â—¦ compression. â—¦ Concurrently, expeditious transfer to an operating room and preparations for cesarean delivery are completed. â—¦ Rarely, vaginal or operative vaginal birth is reasonable if it can be completed much more rapidly than emergent cesarean birth
- 22. Compound Presentation â—¦ an extremity prolapses alongside the presenting part, and both â—¦ present simultaneously in the pelvis
- 23. â—¦ In most cases, the prolapsed part should be left alone. It typically does â—¦ not impede labor and often retracts out of the way with descent of the â—¦ presenting part. If it fails to retract and if it appears to prevent descent of the â—¦ head, the prolapsed part can be pushed gently upward and the head â—¦ simultaneously downward by fundal pressure. In cases with a co-presenting â—¦ hand, the fetus may reflexively retract the hand if pinched by the provider. â—¦ In general, rates of perinatal mortality and morbidity are increased, but â—¦ these mainly stem from effects of associated preterm birth, prolapsed â—¦ umbilical cord, and traumatic obstetrical procedures. Tebes and coworkers â—¦ (1999) described a rare case of pressure-induced forearm ischemia and later â—¦ surgical amputatio
- 24. COMPLICATIONS WITH DYSTOCIA ◦ Dystocia, especially if labor is prolonged, is associated with a higher incidence of several common obstetrical and neonatal complications ◦ Maternal infection, either intrapartum chorioamnionitis or postpartum endomyometritis, ◦ Postpartum hemorrhage from atony ◦ Uterine tears – second stage caesarean section ◦ Uterine rupture –prolonged labour ◦ the upper segment of the uterus contracts, retracts, and expels the fetus. ◦ In response, the softened lower uterine segment and cervix dilate and thereby form a greatly expanded, thinned-out tube through which the fetus can pass. ◦ The boundary between these segments is the physiological retraction ring the pathological retraction ring of Bandl
- 25. â—¦ Fistula formation â—¦ Lower-extremity nerve injury â—¦ Caput succedaneum and molding develop commonly and may be impressive â—¦ Mechanical trauma â—¦ such as nerve injury, fractures, and cephalohematoma also are more frequent