Acinetobacter
- 2. Introduction âĒ The name, Acinetobacter, comes from the Latin word for "motionless," because they lack cilia or flagella with which to move. âĒ Have 32 species, A. baumanii and A. lwoffii have greatest clinical importance. 2
- 3. Introduction âĒ Most species are not significant sources of infection. However, one opportunistic species, Acinetobacter baumannii, is found primarily in hospitals and poses a risk to people who have supressed immunity. âĒ >2/3 of Acinetobacter infections are due to A. baumannii 3
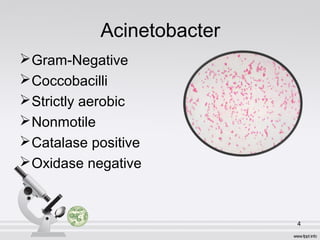
- 4. Acinetobacter ïGram-Negative ïCoccobacilli ïStrictly aerobic ïNonmotile ïCatalase positive ïOxidase negative 4
- 5. Epidemiology Environmental reservoirs âĒSoil âĒFresh water âĒVegetables âĒAnimals âĒBody lice, fleas, ticks 5
- 6. Epidemiology In the hospitalâĶ âĒ Environmental surface âĒ Ventilators, dialysis machines, air ventilation systems, water sources âĒ Hands âĒ Contaminated suction equipment âĒ Respiratory, urinary, GI tracts & wounds of patients 6
- 7. Growth Requirment Aerobic Grow at 44° C Differential Media â MacConky Agar Selective Media â CHROM Agar â Leeds Acinetobacter Agar 7
- 8. 8 MacConky Agar CHROM Agar Leeds Acinetobacter Agar
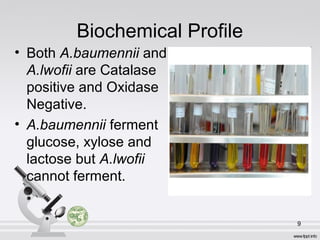
- 9. Biochemical Profile âĒ Both A.baumennii and A.lwofii are Catalase positive and Oxidase Negative. âĒ A.baumennii ferment glucose, xylose and lactose but A.lwofii cannot ferment. 9
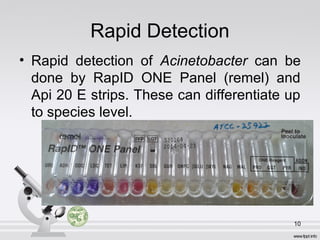
- 10. Rapid Detection âĒ Rapid detection of Acinetobacter can be done by RapID ONE Panel (remel) and Api 20 E strips. These can differentiate up to species level. 10
- 11. Molecular Detection âĒ A.baumennii and A.lwofii can be detected by PCR. âĒ recA specific primers are used to detect recA gene in A.baumennii, giving a 382 bp fragment âĒ est specific primers are used to detect est gene in A.lwofii, giving a 309 bp product. 11
- 12. Pathogenesis ïķOpportunistic pathogenâĶ ïķSurvive under dry conditions Virulence Factors âĒ Polysaccharide capsule, prevent complement activation, delay phagocytosis âĒ Fimbriae (adhere to human bronchial epithelium) âĒ Pilli (colonization of environmental surface to form biofilms) 12
- 13. Transmission âĒ Acinetobacter can be spread from person to person (infected or colonized patients), contact with contaminated surfaces of exposure to the environment. 13
- 14. Antibiotic Resistance âĒ Acinetobacter species are capable of accumulating multiple antibiotic resistance genes, leading to the development of multidrug-resistant or even panresistant strains. 14
- 15. Antibiotic Resistance Mechanisms âĒ Antibiotic-altering enzymes (beta-lactams, carbapenems, aminoglycosides) âĒ Reduced outer membrane porin expression (beta-lactams, carbapenems) âĒ Altered penicillin-binding proteins (beta- lactams, carbapenems) âĒ DNA gyrase and topoisomerase IV mutations (quinolones) 15
- 16. Treatment âĒ Multidrug-resistant A. baumannii is a common problem in many hospitals. First line treatment is with a Carbapenems antibiotic such as imipenem, but carbapenem resistance is increasingly common. Other treatment options include Polymyxin, Tigecycline and Aminoglycosides. 16
- 17. Treating the Resistant Infections âĒ Colistin and Polymyxin B have been used to treat highly resistant Acinetobacter infections. The choice of appropriate therapy is further complicated by the toxicity of colistin which is mainly renal. âĒ Acinetobacter isolates resistant to colistin and Polymyxin B have also been reported 17
- 18. Summary âĒ Opportunistic pathogen âĒ Nosocomial infection âĒ Grow best at aerobic conditions âĒ Can be transmitted by contact âĒ Possessing antibiotic resistant 18
- 20. 20 Wash your hands and shut them off.
Editor's Notes
- #3: A. Hemolyticum A. Junnii A. Johnsonii
- #5: Short, broad rod during rapid growth Coccobacillary shape in stationary phase
- #9: Colonies are 1 to 2 mm, nonpigmented, domed, and muciod, with smooth to pitted surfaces.
- #10: Oxidase negative (opposite to Neisseria spp. or Moraxella spp.) Haemolytic Indole negative. Catalase positive.
- #16: Quinoloine and nalidixic acid- inhibit DNA/RNA synthesis Rifamycine- prevent DNA synthesis Erythromycine, chloramphenicol- disruption of 50s subunit of ribosome Tetracycline, gentamycine and streptomycine- 30s subunit disruption
- #17: Polymyxin- Disruption of cell membrane Penicilline, cephalosporine and beta-lactam - inhibition of cell wall synthesis Sulfonamide and trimethoporine- inhibition of folic acid synthesis