Acute pancreatitis
- 1. Acute pancreatitis PRESENTED BY: IRFAN UL HAQ MBBS FINAL YEAR. GMC SRINAGAR.
- 2. Definition ïĩ Acute pancreatic inflammation associated with little or no fibrosis. ïĩ It ranges from a mild self-limiting inflammation of the pancreas to critical disease characterized by infected pancreatic necrosis, multiple organ failure and a high risk of mortality.
- 3. Pancreas with biliary tree
- 4. Epidemiology ïĩ Worldwide annual incidence of acute pancreatitis may range from 5 to 50 per 100,000 with highest incidence in Finland and US. ïĩ The disease may occur at any age , with peak in young men and older women. ïĩ Smoking is an independent risk factor for acute pancreatitis.
- 5. Aetiology ïĩ There are two major causes of acute pancreatitis which are ïĩ Gallstones and ïĩ Alcohol abuse. ïĩ Gallstone pancreatitis is seen in 50-70% of cases whereas due to alcohol abuse it is 25%. ïĩ The other possible causes of acute pancreatitis are: ïĩ Biliary tract disease ïĩ Hyperlipidemia ïĩ Hereditary ïĩ Hypercalcemia
- 6. Aetilogy (contdâĶ) ïĩ Trauma: ïĩ External ïĩ Surgical ïĩ Endoscopic retrograde cholangiopancreatography. ïĩ Ischemia: ïĩ Hypoperfusion ïĩ Atheroembolic ïĩ Vasculitis ïĩ Pancreatic duct obstruction: ïĩ Neoplasms ïĩ Pancreas divisum ïĩ Ampullary and duodenal lesions ïĩ Infections. ïĩ Venom. ïĩ Drugs. ïĩ Idiopathic.
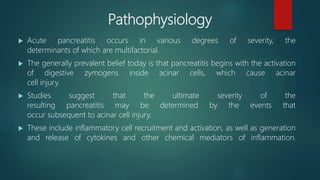
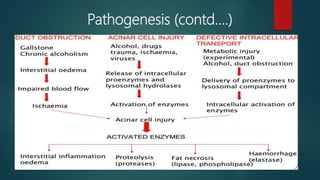
- 7. Pathophysiology ïĩ Acute pancreatitis occurs in various degrees of severity, the determinants of which are multifactorial. ïĩ The generally prevalent belief today is that pancreatitis begins with the activation of digestive zymogens inside acinar cells, which cause acinar cell injury. ïĩ Studies suggest that the ultimate severity of the resulting pancreatitis may be determined by the events that occur subsequent to acinar cell injury. ïĩ These include inflammatory cell recruitment and activation, as well as generation and release of cytokines and other chemical mediators of inflammation.
- 9. Clinical features ïĩ The most common symptoms and signs include: ïĩ Severe epigastric pain radiating to the back, relieved by leaning forward. ïĩ Nausea, vomiting, diarrhea and loss of appetite. ïĩ Fever/chills. ïĩ Hemodynamic instability, including shock. ïĩ In severe case may present with tenderness, guarding, rebound .
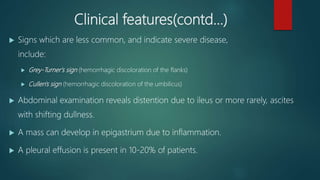
- 10. Clinical features(contdâĶ) ïĩ Signs which are less common, and indicate severe disease, include: ïĩ Grey-Turner's sign (hemorrhagic discoloration of the flanks) ïĩ Cullen's sign (hemorrhagic discoloration of the umbilicus) ïĩ Abdominal examination reveals distention due to ileus or more rarely, ascites with shifting dullness. ïĩ A mass can develop in epigastrium due to inflammation. ïĩ A pleural effusion is present in 10-20% of patients.
- 11. Cullenâs sign
- 13. Investigations ïĩ Full blood count: neutrophil leukocytosis. ïĩ Electrolyte abnormalities include hypokaemia, hypocalcemia. ïĩ Elevated LDH in biliary disease. ïĩ Glycosuria ( 10% of cases). ïĩ Blood sugar: hyperglycaemia in severe cases. ïĩ Ultrasound look for stones in biliary tract diseases. ïĩ Abdominal CT scan may reveal phlegmon (inflammatory mass), pseudocyst or abscess(complications of acute pancreatitis).
- 14. Investigations(contdâĶ) Amylase and lipase : ïĩ Elevated serum amylase and lipase levels, in combination with severe abdominal pain, often trigger the initial diagnosis of acute pancreatitis. ïĩ Serum lipase rises 4 to 8 hours from the onset of symptoms and normalizes within 7 to 14 days after treatment. ïĩ Marked elevation of serum amylase level during first 24 hours ïĩ Reasons for false positive elevated serum amylase include salivary gland disease (elevated salivary amylase) and macroamylasemia. ïĩ If the lipase level is about 2.5 to 3 times that of Amylase, it is an indication of pancreatitis due to Alcohol or gallstone ïĩ The degree of amylase/lipase elevation does not correlate with severity of acute pancreatitis.
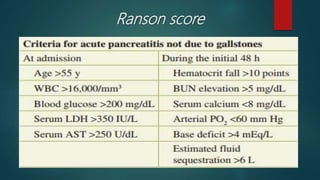
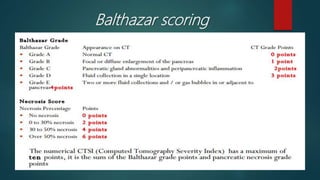
- 15. Assesment of severity of AP. ïĩ Different scoring systems have been applied to asses the severity and prognosis of acute pancreatitis viz: ïĩ Ranson Score. ïĩ APACHE II Score. ïĩ Balthazar Score.
- 16. Ranson score
- 18. APACHE II Score(Acute Physiology And Chronic Health Evaluation) Score 0 to 2 : 2% mortality. Score 3 to 4 : 15% mortality. Score 5 to 6 : 40% mortality. Score 7 to 8 : 100% mortality. 1) Hemorrhagic peritoneal fluid. 2) Obesity. 3) Indicators of organ failure. 4) Hypotension (SBP <90 mmHG) or tachycardia > 130 beat/min. 5) PO2 <60 mmHg. 6) Oliguria (<50 mL/h) or increasing BUN and creatinine. 7) Serum calcium < 1.90 mmol/L (<8.0 mg/dL). 8) Serum albumin <33 g/L (<3.2.g/dL).
- 20. Complications ïĩ Immediate: ïĩ Shock. ïĩ DIVC. ïĩ ARDS. ïĩ Late: ïĩ Pancreatic pseudocyst. ïĩ Pancreatic abscess. ïĩ Pancreatic necrosis. ïĩ Pancreatic jaundice. ïĩ Persistant duodenal ileus. ïĩ G I bleed. ïĩ Pancreatic ascites.
- 21. Management ïĩ IV fluid replacement (normal saline). ïĩ Bowel rest (NG tube, NPO) in severe case. ïĩ Administration of meperidine/pethidine as pain killer. ïĩ Antiemetic if necessary. ïĩ Monitor & correct electrolytes. ïĩ Prevent infection by antibiotic prophylaxis. ïĩ Determine & treat specific etiology(avoid alcohol). ïĩ Indication to surgery if pancreatitis not respond to treatment.