Acute PVD.pptx
- 1. ? Predictive ? Non Predictive ? Protective
- 2. What Literature says: âĒ Acute PVD is typically accompanied by floaters (myodesopias or entopsias) or light flashes (photopsias) âĒ Significant variability in the literature regarding what the presence or absence of these symptoms implies âĒ studies have variably reported that photopsia symptoms are âĒ 1. Predictive either of a complicated PVD, nonpredictive, or protective âĒ The risk of RT or RRD occurring with PVD in published reports ranges widely from 15.0% to 27.1%
- 3. Current concept âĒ Acute posterior vitreous detachment (PVD) is a critical lifetime event that may be associated with the development of a retinal tear (RT) or rhegmatogenous retinal detachment (RRD), which may in turn result in permanent vision loss if not identified and treated promptly.
- 4. What is the problem with current thinking? âĒ Prior studies evaluating acute PVD have been typically performed in retinal specialty practices and likely suffer from referral bias for more significant PVD-related events
- 5. The Question? âĒ What are the risk factors for retinal tear (RT) or rhegmatogenous retinal detachment (RRD) associated with acute, symptomatic posterior vitreous detachment (PVD) in a comprehensive eye care setting
- 6. Main Issue âĒ By not referring to a retina specialist, is the comprehensive ophthalmologist correct ? âĒ Especially the chances of missing âPresence of RT or RRD at initial presentation or within 1 year thereafterâ.
- 7. Reference âĒ Complications of Acute Posterior Vitreous Detachment. VOLUME 129, ISSUE 1, P67-72, JANUARY 01, 2022. âĒ Michael I. Seider, MDCarol Conell, PhD,Ronald B. Melles, MD
- 8. Rate of RT and RRD associated with acute PVD to be lower than rates previously reported by retina subspecialty practices. Several patient features strongly predicted the presence of initial and late complications of acute PVD Complications of Acute Posterior VitreousDetachment Michael I. Seider, MD,1,2 Carol Conell, PhD,3 Ronald B. Melles, M Ophthalmology Volume 129, Number 1, January 2022
- 9. âHow likely is a patient to have a complicated PVD based on features that can be determined by a comprehensive ophthalmologistâ
- 10. Role of comprehensive ophthalmologist: âĒ Understand âĒ Risk of RT/RRD at presentation and within 1 year âĒ Evaluation of rates and risk factors âĒ Relate between refraction and risk of RT/RRD
- 12. Population distribution of 8305 patients presenting with acute symptomatic posterior vitreous detachment (PVD). Women made up 61.2% of the cohort and presented at a slightly earlier age than men (63.1 vs. 64.7 years, respectively).
- 13. Risk factors: History & Symptoms âĒ Blurred vision âĒ Age < 60 years âĒ Prior cataract surgery âĒ Prior photorefractive surgery âĒ Symptoms < 1 week duration âĒ Family history of RD âĒ Floaters âĒ Flashes
- 14. Risk factors: Signs âĒ Vitreous pigment âĒ Vitreous hemorrhage âĒ Retinal hemorrhage âĒ Lattice degeneration âĒ Vision < 20/40
- 15. âĒ Initial and delayed rates of acute posterior vitreous detachment (PVD) complicated by retinal tear (RT) or retinal detachment (RD) âĒ âHigh-risk factors for delayed events included any vitreous hemorrhage, lattice degeneration, or history of RT or RD in the fellow eye
- 16. Highly predictive of the presence of complicated PVD
- 17. The median interval until a late event was 22 days after initial presentation 93 of the late complications (70.0%) occurred within 6 weeks. Sixty of the late events (45.1%) were detected at a scheduled follow-up appointment
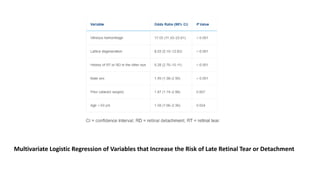
- 18. Multivariate Logistic Regression of Variables that Increase the Risk of Late Retinal Tear or Detachment
- 19. Refractive Error âĒ High myopia (-3.00D -6.0 D ) risk factor for complicated PV âĒ Independent of patient age âĒ Relatively linear relationship âĒ Between âĒ The age at presentation of PVD and refractive error âĒ Myopic patients presenting at a younger age âĒ Hyperopes at a later age, compared with emmetropes
- 20. Factors predictive of Late events âĒ More likely to occur in patients who initially presented with âĒ 1. Vitreous hemorrhage âĒ 2. Lattice degeneration âĒ 3. History of RT or RD in the fellow eye âĒ 4. Occur at a median of 22 days after presentation âĒ 5. Follow up closely sooner than interval of 6 weeks
- 21. Salient Points âĒ Incidence of RT during acute PVD in comprehensive ophthalmology is substantially lower than that reported in series from retina subspecialty clinics âĒ Specific risk factors that can assist in predicting which patients are at highest risk of complicated PVD both at triage and the time of initial examination
- 22. Predictive Factors of Late events âĒ Vitreous hemorrhage âĒ Lattice degeneration, âĒ History of RT or RRD in the fellow eye âĒ Patients with any of these key characteristics should be observed closely
- 23. Refractive error âĒ Close relationship among refractive error, patient age at PVD, and risk of complicated PVD, with myopic eyes not only presenting at a younger age but also having an independently greater risk of associated RT or RRD