Advanced cardiac life support at emergency department
- 1. ADVANCED CARDIAC LIFE SUPPORT SUBMITTED BY SATHESHWARI N II YR MSC N
- 2. INTRODUCTION ŌĆó Advanced cardiac life support(ACLS) or advanced cardiovascular life support refers to a set of clinical interventions for urget treatment of cardiac arrest and other life- threadening medical emergencies,as well as the knowledge and skills to deploy those interventions. ŌĆó American heart association ( AHA) protocols are considered to be gold standard ACLS protocols, and it gets reviewed every 5 years. ŌĆó ACLS is build heavily upon the foundation of BLS ( Basic life support ).
- 3. DEFINITION ŌĆó Advanced cardiac life support, advanced cardiovascular life support refers to a set of clinical guidelines for the urgent and emergent treatment of life- threating cardiovascular conditions that will cause or have caused cardiac medicatios, and techniques.
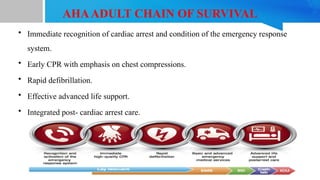
- 4. AHAADULT CHAIN OF SURVIVAL ŌĆó Immediate recognition of cardiac arrest and condition of the emergency response system. ŌĆó Early CPR with emphasis on chest compressions. ŌĆó Rapid defibrillation. ŌĆó Effective advanced life support. ŌĆó Integrated post- cardiac arrest care.
- 5. COMPONENTS OF HIGH QUALITY CPR IN BLS SCENE SAFETY ŌĆó Make sure the environment is safe for recuers and victim. RECOGNITION OF CARDIAC ARREST ŌĆó Check for responsiveness ŌĆó No breathing or only gasping ( no normal breathing ) ŌĆó No definitive pulse left with in 10 secs ( cartoid or femoral pulse ) ŌĆó Breathing and pulse check can be performed with in 10 secs
- 6. ACTIVATION OF EMERGENCY RESPONSE SYSTEM ŌĆó If done with no mobile phone, leave the victim to activate the emergency response system and get the AED befre beginning CPR. ŌĆó Otherwise, send someone and begin CPR immediately, use the AED as soon as it is available. 1. Chest compression 30 : 2 2. Compression rate 100 - 120 / min 3. Compression depth -- at least 5 cm or 2 inches 4. Hand placement - 2 hands on the half of the sternum 5. Chest recoil- allow full chest recoil 6. Minimize interuptions - < 30 secs ( Early defibrillation and early CPR for treatable arrhythmias remains the corner stone of ACLS)
- 8. IN HOSPITAL CARDIAC ARREST (IHCA)
- 9. OUT HOSPITAL CARDIAC ARREST (OHCA)
- 11. CPR QUALITY ŌĆó Push hard ( at least 2 inches (5 cm) and fast (100- 120/min) and allow complete chest recoil. ŌĆó Minimize interuptions in compressions. ŌĆó Avoid excessive ventilation. ŌĆó Change compresser every 2 minutes, or sooner if fatiqued. ŌĆó If no advanced airway, 30:2 compression : ventilation ratio. ŌĆó Quantitative waveform capnography. If PETCO2 is low oe decreasing reassess CPR quality
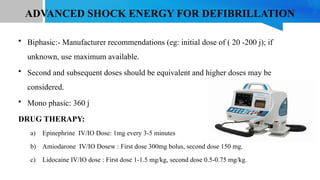
- 12. ADVANCED SHOCK ENERGY FOR DEFIBRILLATION ŌĆó Biphasic:- Manufacturer recommendations (eg: initial dose of ( 20 -200 j); if unknown, use maximum available. ŌĆó Second and subsequent doses should be equivalent and higher doses may be considered. ŌĆó Mono phasic: 360 j DRUG THERAPY: a) Epinephrine IV/IO Dose: 1mg every 3-5 minutes b) Amiodarone IV/IO Dosew : First dose 300mg bolus, second dose 150 mg. c) Lidocaine IV/IO dose : First dose 1-1.5 mg/kg, second dose 0.5-0.75 mg/kg.
- 13. ADVANCED AIRWAY ŌĆó Endotrachial intubation or supraglottic advanced airway ŌĆó Waveform capnography or capnometry to confirm and monitor ET tube/ Placement. ŌĆó Once advanced airway in place, give 1 breath every 6 seconds ( 10 breaths/ min) with continous chest compressions.
- 14. RETURN OF SPONTANEOUS CIRCULATION (ROSC) ŌĆó Pulse and blood pressure ŌĆó Abrupt sustained increase in PETCO2 ( typically Ōēź 40 mm Hg) ŌĆó Spontaneous arterial pressure wave with intra arterial pressure
- 15. REVERSIBLE CAUSES 5 H ŌĆō Hypovolemia ŌĆō Hypoxia ŌĆō Hydrogen ion ( acidosis) ŌĆō Hypo, Hyperkaelemia ŌĆō Hypothermia 5 T ŌĆō Tension pneumothorax ŌĆō Tanponade, cardiac ŌĆō Toxins ŌĆō Thrombosis, pulmonary ŌĆō Thrombosis, coronary
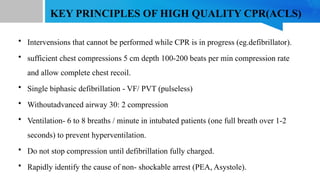
- 16. KEY PRINCIPLES OF HIGH QUALITY CPR(ACLS) ŌĆó Intervensions that cannot be performed while CPR is in progress (eg.defibrillator). ŌĆó sufficient chest compressions 5 cm depth 100-200 beats per min compression rate and allow complete chest recoil. ŌĆó Single biphasic defibrillation - VF/ PVT (pulseless) ŌĆó Withoutadvanced airway 30: 2 compression ŌĆó Ventilation- 6 to 8 breaths / minute in intubated patients (one full breath over 1-2 seconds) to prevent hyperventilation. ŌĆó Do not stop compression until defibrillation fully charged. ŌĆó Rapidly identify the cause of non- shockable arrest (PEA, Asystole).
- 17. CONTD... ŌĆó Irreversible causes 5 tŌĆÖs, 5 hŌĆÖs are to be corrected rapidly. ŌĆó Definitive airway management may be delayed if there is adequate recue breahing without an advanced airway in place. ŌĆó A blindly inserted supraglottic airway (eg. laryngeal mask airway, combitube laryngeal tube, can be placed without interupting chest compressions. ŌĆó Provide adequate ventilation in modt casese and reduce the risk of aspiration as compared to bag- m,ask ventilation. ŌĆó Attempets at intubation should last no longer than 10 seconds.
- 18. MANAGEMENT OF ARRHYTHMIAS ŌĆó VENTRICULAR FIBRILLATION/ PULSELESS VENTRICULAR TACHYCARDIA 1. Early defibrillation is the most critical action in the resuscitaion effort, followed by the performance of excellent CPR. 2. Manage potentially treatable underlying causes as appropriate. 3. Decreased time in defibrillation improves the likelihood of successful conversion to a perfusing rhythm and patient survival. Biphasic- 100-120 J- ventricular fibrillation Monophasic 360 J - pulseless ventricular tachycardia
- 19. 1. Epinephrine 1mg IV every 3 - 5 min (while CPR) 2. Vasopressin (40 units/ IV) first and second close of epinephrine. 3. Amiodarone ( 300mg IV with a repeat dose of 150 mg IV as indicated) 4. lodocaine ( 1- 1.5mg/kg/ IV then 0.5 - 0.75 mg/kg every 5 to 10 minutes. 5. Magnesiumsulphate 2g IV followed by a manintaience infusion
- 20. ASYSTOLE/ PEA ŌĆó Complete absence of demonstrable electrical and mechanical cardiac activity is asystole. ŌĆó PEA - pulseless electrical activity is defined as any one of a heterogenous group of organised electrocardiographic rhythms without sufficient mechanical conraction of the heart to produce a palpable pulse or measurable blood pressure. ŌĆó Treat irreversible caueses. ŌĆó Atropine is no longer recommended.
- 21. BRADYCARDIA ŌĆó Assess appropriateness for clinical condition. ŌĆó HR typically < 50 min in brady arrhythmia ŌĆó Identify and treat underlying cause. 1. Maintain patent airway, assist breathing as necessary 2. Oxygen (if hypoxaemia) 3. Cardiac monitor ti idebtify rhythm, Monitor blood pressure and oximetry 4. IV access 5. 12 lead ECG if available, donŌĆÖt delay therapy 6. consider possible hypoxia and toxicologic causes 7. Persistent bradyarrhythmia causing ( hypotension, acutely altered mental status)
- 22. No signs of shock No Ischemic chest discomfort Acute heart failure Atropine if atropine ineffective Transcutaneous pacing and /orŌĆÖ Dopamine infusion or epinephrine infusion Consider Expert consultation Transvenous pacing M o n i t o r & o b s e r v e
- 23. DRUG DOSES Atropine IV infusion ’āś First dose: 1 mg bolus ’āś Repeat every 3-5 minutes ’āś Maximum 3 mg Dopamine IV dose ’āś Uusual infusion rate is 5- 20 mcg/ kg per minute. titrate to patient response slowly. Epinephrine ’āś 2- 10 mcg per minute infusion ’āś Titrate to patient response ’āś Causes- MI, drugs toxicity ( CCB, BB, digoxin), hypoxia, electrolyte abnormality.
- 24. TACHYCARDIA ŌĆó Assess appropriateness for clinical condition ŌĆó HR typically Ōēź 150 / min if tachy arrhythmias. DRUG DOSES Adenosin IV doses ŌĆō 1st dose 6mg rapid IV push- follow with NS flush ŌĆō 2 nd dose 12 mg if required Antiarrhythmic infusions for stsble wide QR tachycardia Procainamide IV dose ŌĆō 20-50 mg/min until arrhythmia suppressed. Amiodarone ŌĆō 1st dose 150 mg over 10 minutes, repeat as needed. Sotalol IV dose ŌĆō 100 mg ( 1.5mg/kg) over 5 minutes.
- 25. POST CARDIAC ARREST CARE
- 26. TERMINATION OF RESUSCITATION Factors influencing the decision to stop resuscitative efforts include:- 1. Duration of resusitative effort > 30 min without sustained perfusing rhythm. 2. Initial electrocardiographic rhythm of asystole. 3. Prolonged interval between estimated time of arrest and initiation of resuscitation. 4. Patient age and severity of comorbid disease. 5. Absence of brain steam reflexes 6. Normothermic. 7. EFCO2 < 10 mmhg even after > 20 minutes of resuscitation.