ANTEPARTUM HAEMORRHAGE.pptx
- 2. ŌĆó Third-trimester bleeding, ranging from spotting to massive hemorrhage, occurs in 2% to 6% of all pregnancies. ŌĆó The differential diagnosis includes: ŌĆó Bloody show from labor ŌĆó Abruptio placentae (AP) ŌĆó Placenta previa (PP) ŌĆó Vasa previa (VP) ŌĆó Cervicitis, postcoital bleeding, trauma, uterine rupture, and carcinoma.
- 3. PLACENTA
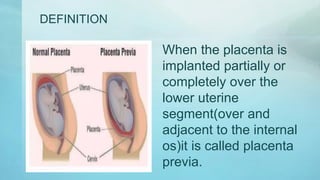
- 5. DEFINITION When the placenta is implanted partially or completely over the lower uterine segment(over and adjacent to the internal os)it is called placenta previa.
- 6. INCIDENCE O.5 ŌĆō 1% among hospital deliveries ŌĆó80% cases found in multiparous women ŌĆó Increase incidence beyond 35yrs ŌĆóIncrease incidence with high birth order and multiple pregnancy 1 in 300- 400 pregnancy .
- 7. MECHANISM OF BLEEDING ŌĆóProgressive stretching of the lower uterine segment normally occurs during the 3rd trimester and labour, but the inelastic placenta cannot stretch with it. This leads to inevitable separation of a part of the placenta with unavoidable bleeding. ŌĆóThe closer to term, the greater is the amount of bleeding.
- 8. ETIOLOGY THEORIES POSTULATED ŌĆóDropping down theory ŌĆóPersistence of chorionic activity ŌĆóDefective decidua ŌĆóBig surface area of the placenta
- 9. HIGH RISK FACTORS ŌĆóMultiparity ŌĆóIncreased maternal age ŌĆóPrevious cesarean section or any other scar in the uterus ( fibroids myomectectomy ) ŌĆóPlacental size and abnormality ( twin) ŌĆóSmoking( due to defective decidual vascularisation) ŌĆóPrior curettage
- 10. BROWNE`S CLASSIFICATION 1. TYPE I ŌĆō Low ŌĆō lying Major part of the placenta is attached to the upper segment ŌĆóOnly the lower margin encroaches to the lower segment But not up to the os 2. TYPE II ŌĆō Marginal ŌĆóPlacenta reaches the margin of the internal os But does not cover it 3. TYPE III ŌĆō Incomplete or partial central ŌĆó Placenta covers the internal os partially 4. TYPE IV ŌĆō Central or total ŌĆó Placenta covers the internal os even after it is fully dilated Type 1 and type 2 are minor degree. Type 3 and 4 are major degree.
- 13. CLINICAL FEATURES & SYMPTOMS ŌĆóVAGINAL BLEEDING ŌĆō ŌĆóThe classical presentation is painless antepartum haemorrhage. Causeless Recurrent SIGNS ŌĆóGeneral condition and anemia are proportionate to the visible blood loss ŌĆóABDOMINAL EXAMINATION ŌĆóThe size of the uterus proportionate to the period of gestation ŌĆóThe uterus feels relaxed, soft and elastic without any localised area of tenderness ŌĆóPersistence of malpresentation ( breech) ŌĆóHead is floating ŌĆóFetal heart sound heard usually ŌĆóStallworthyŌĆÖs sign ŌĆóVAGINAL EXAMINATION SHOULD NOT BE DONE IN SUSPECTED
- 14. CONFIRMATION OF DIAGNOSIS ŌĆó LOCALISATION OF PLACENTA ŌĆó SONOGRAPHY ŌĆó TAS ŌĆó TVS ŌĆó Color Doppler flow study ŌĆó MAGNETIC RESONANCE IMAGING CLINICAL ŌĆó By internal examination(double set up examination) ŌĆó Direct visualization during caesarean section ŌĆó Examination of the placenta following vaginal delivery
- 15. MANAGEMENT ŌĆó There are two types of management for placenta previa based on certain criteria ŌĆó They are : ŌĆó Expectant management ŌĆó Active management ŌĆó The most important guiding principle is when the mothers life is at risk donŌĆÖt think about saving the baby
- 16. MANAGEMENT ’āś IMMEDIATE ATTENTION ŌĆó Blood samples are taken ŌĆó A large bore IV cannula is sited ŌĆó Infusion of NS ŌĆó Gentle abdominal palpation ŌĆó Inspection of vulva ŌĆóEXPECTANT MANAGEMENT - Macaffee and Johnson regime ŌĆó Bed rest ŌĆó Periodic inspection ŌĆó Supplementary hematinics ŌĆó A gentle speculum examination ŌĆó Rh immunoglobulin ŌĆó Termination done at 37 weeks ŌĆó Steroid therapy - Inj betamethasone is given to hasten the lung maturity of the fetus
- 17. CONT. ’āśEXPECTANT MANAGEMENT - Macaffee and Johnson regime ŌĆó Bed rest ŌĆó Periodic inspection ŌĆó Supplementary hematinics ŌĆó A gentle speculum examination ŌĆó Rh immunoglobulin ŌĆó Termination done at 37 weeks ŌĆó Steroid therapy ŌĆō Inj. betamethasone is given to hasten the lung maturity of the fetus
- 18. ACTIVE MANAGEMENT INDICATIONS ŌĆó Bleeding occurs at or after 37 weeks of pregnancy ŌĆó Patient is in labour ŌĆó Patient is exsaguinated state on admission ŌĆó Bleeding is continuing and of moderate degree ŌĆó Baby is dead or known to be congenitally malformed ’üČ DEFINITIVE MANAGEMENT ŌĆó CESAREAN DELIVERY ŌĆó Placental edge is within 2cm from the internal os ŌĆó VAGINAL DELIVERY ŌĆó Placental edge is clearly 2-3cm away from the internal os
- 19. COMPLICATION MATERNAL DURING PREGNANCY ŌĆó APH ŌĆó Malpresentation ŌĆó Premature labor
- 20. Complications during labour MATERNAL Early rupture of the membrane ŌĆó Cord prolapse ŌĆó Slow dilation ŌĆó Intrapartum haemorrhage ŌĆó Increased incidence of operative interference PPH FETAL ŌĆó Asphyxia ŌĆó Birth injury ŌĆó Low birth weight (m/c) ŌĆó IUD ŌĆó Congenital malformations
- 22. DEFINITION DEFINITION Abruptio placenta is defined as haemorrhage occurring in pregnancy due to the separation of a normally situated placenta. It is also called accidental haemorrhage or premature separation of placenta.
- 23. ŌĆóINCIDENCE ŌĆó It is 1 : 200 ŌĆó It is less than previa ŌĆó Accounts for 5 % maternal mortality and 20% perinatal mortality
- 24. Types of abruption 1. Revealed ŌĆó In this type the blood seeps between the decidua and the membranes to present at the vagina 2. Concealed ŌĆó In this the blood gets collected behind the placenta and forms the retro placental clot ŌĆó Sometimes it may be due to collection between the decidua and membranes but it canŌĆÖt present at vagina because the presenting part is firmly pressed over the cervix 3. Mixed 4. ŌĆó In this type it is partly revealed and partly retroplacenta