ASSESSMENT OF AKI IN ER.pptx
- 1. Patient Assessment with AKI in ER BASMAH AL MUSALAM RN,BSN,TOT CERTIFIED ,ICU CLINICAL INSTRUCTOR
- 2. Clinical Objectives By the end of this lecture the audience will be able to: Taking history from the patient for kidney function Discuss the assessment of fluids and electrolytes Differentiate pitting edema scale Assess patient for orthostatic hypotension Explain the needed lab test to assess kidney function Discuss the 5 step approach to AKI in the ED
- 3. Course Contents Introduction History Taking Fluid and Electrolyte Assessment Pitting Edema Scale Orthostatic Hypotension Assessment Laboratory Studies 5 step approach to AKI in the ED
- 4. Introduction ŌĆó Acute kidney injury (AKI), formerly known as acute renal failure (ARF) ŌĆó It is a sudden and often reversible reduction in kidney function, as measured by glomerular filtration rate (GFR) ŌĆó According to Kidney Disease ŌĆō Improving Global Outcomes (KDIGO), AKI is the presence of any of the following: ’ā╝ Increase in serum creatinine by 0.3 mg/dL or more (26.5 micromoles/L or more) within 48 hours. ’ā╝ Increase in serum creatinine to 1.5 times or more baseline, within the prior 7 days ’ā╝ Urine volume less than 0.5 mL/kg/h for at least 6 hours
- 5. https://cutt.us/ljyoG ŌĆó ED-AKI 20.421 19.849 17% 71% 11% Pre renal post renal ATN ER ATTENDANCE NON-ED-AKI
- 6. History of the patient Patient Profile Personal habits Use of herbs, vitamins, and dietary supplements Illicit drug use Financial problems resulting from illness Sexual function
- 7. History of the patient Family History Current Medication Use Hypertension Diabetes mellitus Polycystic kidney disease Chronically swollen extremities Nonsteroidal anti-inflammatory medications Antibiotics Antihypertensive Diuretics Use of iodine-based radiographic contrast media
- 8. Past Kidney Studies ’āś Urinalysis with proteinuria ’āś Creatinine clearance ’āś Kidney-ureter-bladder (KUB) radiograph ’āś Intravenous pyelogram ’āś Kidney ultrasound ’āś Renal arteriography ’āś Kidney biopsy
- 9. Fluid and Electrolyte Assessment
- 10. Fluid Status
- 11. Fluid Status
- 12. Electrolyte and Waste Product Status Chvostek & Trousseau signs sodium, potassium, calcium levels
- 13. Electrolyte and Waste Product Status Therapies that can alter electrolyte status ( diuretics, antihypertensives, calcium channel blockers) Gastrointestinal changes (nausea and vomiting Muscle strength (potassium, BUN) Behavioral and mental changes (sodium, BUN levels)
- 16. JVP Assessment
- 17. Laboratory Studies Assessment Test BUN is increased when kidney function deteriorates. Blood urea nitrogen (BUN) is used to trend kidney function in critical illness as creatine is not re sorbed by the kidney tubules and rises when kidney function deteriorates. Serum creatinine is a newer serum biomarker for early identification of acute kidney injury Cystatin C Electrolyte derangements are frequent in kidney failure including: sodium, potassium, phosphate, calcium, chloride, and bicarbonate.. Electrolyte increased in kidney failure in association with electrolyte and acidŌĆōbase changes. Anion gap provide valuable information about kidney function, but results are not reliable if the patient has recently been administered diuretics Urinalysis
- 18. 5 step approach to AKI in the ED
- 19. Step 1 Rule out the immediate life-threats ŌĆó Vital signs - Temp, Bp, saturation ŌĆ”.etc ŌĆó Hyperkalemia ŌĆō ECG, electrolytes sample ŌĆó Severe acidosis ŌĆō Blood Gas
- 20. Step 2 Assess for adequate perfusion ŌĆō are they in shock? ŌĆó Use your history, physical examination and POCUS to assess for perfusion and treat shock (hemorrhagic, vasodilatory, cardiogenic shock etc.) accordingly.
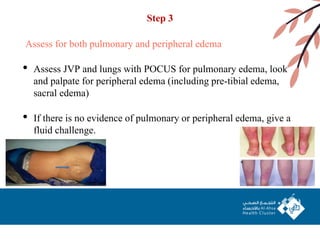
- 21. Step 3 Assess for both pulmonary and peripheral edema ŌĆó Assess JVP and lungs with POCUS for pulmonary edema, look and palpate for peripheral edema (including pre-tibial edema, sacral edema) ŌĆó If there is no evidence of pulmonary or peripheral edema, give a fluid challenge.
- 22. Step 3 A. AKI with adequate perfusion, with pulmonary edema (with or without peripheral edema) ŌĆó furosemide 1 mg/kg IV (or 1.5 mg/kg IV if on furosemide already) ŌĆó Think about pulmonary renal syndromes other than CHF B. AKI with adequate perfusion, with peripheral edema but not pulmonary edema ŌĆó furosemide 1 mg/kg IV (or 1.5 mg/kg IV if on furosemide already)ŌĆŗ ŌĆó If no improvement in renal function think about hypovolemia (ŌĆ£pre renalŌĆØ) despite peripheral edema Low serum albumin ŌĆō treat underlying cause, and consider hepatorenal syndrome which may require IV albumin Venous insufficiency and/or lymphedema ŌĆō give crystalloid Drug induced edema ŌĆō give crystalloid, reassess offending drug Severe myxedema ŌĆō give L-thyroxine and monitor
- 23. Step 4 The golden rules of AKI workup Measure a post-void residual (PVR) with bladder scan or urethral catheter Get a urine dip to look for blood and protein suggestive of nephritic syndrome Monitor urine output ideally with a urethral catheter Avoid nephrotoxins (NSAIDs, ACEi, ARBs, gentamicin etc)
- 24. Step 5 Consider imaging for a small subset of post-renal AKI Radiology department imaging should be reserved for those patients who: Do not improve with fluid challenge (making pre-renal less likely), Have a normal urine dip (making intra-renal less likely), Have a post-void residual <100mL (making BPH less likely) Have obvious bilateral hydronephrosis on POCUS These patients warrant further imaging as they might have a rare post- renal bilateral ureteric obstruction cause of AKI such as obstructive metastatic cancer, lymphoma or a kidney stone with a solitary kidney.
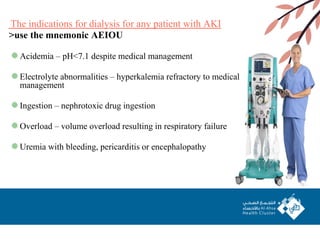
- 25. The indications for dialysis for any patient with AKI >use the mnemonic AEIOU Acidemia ŌĆō pH<7.1 despite medical management Electrolyte abnormalities ŌĆō hyperkalemia refractory to medical management Ingestion ŌĆō nephrotoxic drug ingestion Overload ŌĆō volume overload resulting in respiratory failure Uremia with bleeding, pericarditis or encephalopathy
- 26. References: AKI - Simple ED Approach | Emergency Medicine Cases Overview of the management of acute kidney injury (AKI) in adults ŌĆō UpToDate https://www.stgeorges.nhs.uk/service/renal-medicine/acute-kidney-injury-aki-clinic/ https://www.theinternatwork.com/nephrology-week/2020/4/1/day-1-acute-kidney-injury https://journals.lww.com/cjasn/fulltext/2008/07000/evaluation_and_initial_management_of_acute_kidn ey.11.aspx ds/Patricia_Gonce_Morton_Dorrie_K_Fontaine_Critical_Care_Nursing version 3
- 27. Thank You
Editor's Notes
- #5: Normal creatinine level for men=0.74 to 1.35 mg/dl (65.4 to 119.3micromoles/L ( Normal creatinine level for women =0.59 to 1.04 mg/dl (52.2 to 91.9 micromoles/L ( Urine out put 0.5-1.5ml/kg/hr
- #18: Normal anion gap 4-12meq/l NA+K-(CL+HCO3) NA-(CL+HCO3)
- #22: Pocus = point of care ultrasongraphy
- #24: ACEI =angiotensin converting enzyme inhibitor ARBS =angiotensin receptor blocker
- #25: Benign prostatic hyperplasia (BPH)┬Ā
- #26: Benign prostatic hyperplasia (BPH)┬Ā