Asthma
- 2. DEFINITION • ASTHMA IS A CHRONIC INFLAMMATORY DISEASE OF THE AIRWAYS THAT CAUSES AIRWAY HYPER RESPONSIVENESS, EDEMA AND MUCUS PRODUCTION. • FOR MOST OF THE PATIENTS, ASTHMA IS A DISRUPTIVE DISEASE, AFFECTING SCHOOL AND WORK ATTENDANCE, OCCUPATIONAL CHOICES, PHYSICAL ACTIVITY AND GENERAL QUALITY OF LIFE.
- 3. ETIOLOGY • ALLERGY IS THE STRONGEST PREDISPOSING FACTOR FOR ASTHMA. CHRONIC EXPOSURE TO AIRWAY IRRITANTS OR ALLERGENS ALSO INCREASES THE RISK OF ASTHMA. • COMMON ALLERGENS CAN BE: 1. SEA- SONAL ( GRASS, TREE, WEED POLLENS) 2. PERENNIAL (E.G. MOLD, DUST, ROACHES, ANIMAL DANDER) 3. AIRWAY IRRITANTS 4. FOODS ( SHELL FISH, NUTS) 5. EXERCISE 6. STRESS 7. HORMONAL FACTORS 8. MEDICATIONS, VIRAL RESPIRATORY TRACT INFECTIONS 9. GASTROESOPHAGEAL REFLEX
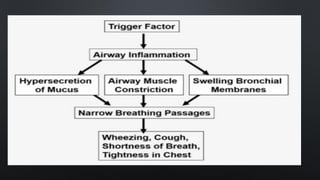
- 4. PATHOPHYSIOLOGY • THE UNDERLYING PATHOLOGY IN ASTHMA IS REVERSIBLE DIFFUSE AIRWAY INFLAMMATION THAT LEADS TO LONG- TERM AIRWAY NARROWING. • THE NARROWING WHICH IS EXACERBATED BY VARIOUS CHANGES IN THE AIRWAY, INCLUDES BRONCHOCONSTRICTION, AIRWAY EDEMA, AIRWAY HYPER RESPONSIVENESS AND AIRWAY REMODELING. • ASTHMA IS A COMPLEX DISEASE PROCESS THAT INVOLVES NUMEROUS INFLAMMATORY AND STRUCTURAL CELLS AS WELL AS MEDIATORS THAT LEAD TO THE DISORDER’S EFFECTS. • MAST CELLS, MACROPHAGES, T- LYMPHOCYTES, NEUTROPHILS, EOSINOPHILS ALL PLAY A KEY ROLE IN THE INFLAMMATION OF ASTHMA.
- 5. PATHOPHYSIOLOGY • WHEN ACTIVATED , MAST CELLS RELEASE SEVERAL CHEMICALS CALLED MEDIATORS. THESE CHEMICALS, WHICH INCLUDE HISTAMINE, BRADYKININ, PROSTANOIDS, CYTOKINES, LEUKOTRIENES AND OTHER MEDIATORS, PERPETUATE THE INFLAMMATORY RESPONSE, CAUSING INCREASED BLOOD FLOW, VASOCONSTRICTION, FLUID LEAK FROM VASCULATURE, ATTRACTION OF WHITE BLOOD CELLS TO THE AREA, MUCUS SECRETION AND BRONCHOCONSTRICTION. • DURING ACUTE EXACERBATIONS OF ASTHMA, BRONCHIAL SMOOTH MUSCLE CONTRACTION OR BRONCHOCONSTRICTION OCCURS QUICKLY TO NARROW THE AIRWAY IN RESPONSE TO AN EXPOSURE. • ACUTE BRONCHOCONSTRICTION DUE TO ALLERGENS RESULTS FROM AN IMMUNOGLOBULIN E ( IGE)- DEPENDENT RELEASE OF MEDIATORS FROM MAST CELLS; THESE MEDIATORS INCLUDE HISTAMINE, TRYPTASE, LEUKOTRIENES, AND PROSTAGLANDINS THAT DIRECTLY CONTRACT THE AIRWAY. • THERE ARE ALSO NON IGE- MEDIATED RESPONSES AND PRO -INFLAMMATORY CYTOKINES.
- 7. • ALPHA AND BETA2 ADRENERGIC RECEPTORS OF THE SYMPATHETIC NERVOUS SYSTEM LOCATED IN THE BRONCHI PLAY A ROLE. • WHEN THE ALPHA- ADRENERGIC RECEPTORS ARE STIMULATED, BRONCHO- CONSTRICTION OCCURS. • BETA2 ADRENERGIC STIMULATION RESULT IN INCREASED LEVEL OF CAMP, WHICH INHIBITS THE RELEASE OF F CHEMICAL MEDIATORS AND CAUSES BRONCHODILATION.,
- 8. CLINICAL MANIFESTATIONS • COUGH • DYSPNEA • WHEEZING • CHEST TIGHTNESS • DIAPHORESIS • TACHYCARDIA • WIDENED PULSE PRESSURE • AN ASTHMA ATTACK OFTEN OCCURS AT NIGHT OR EARLY IN THE MORNING, POSSIBLY BECAUSE OF CIRCADIAN VARIATIONS THAT INFLUENCE AIRWAY RECEPTOR THRESHOLDS.
- 9. ASSESSMENT AND DIAGNOSTIC FINDINGS • A POSITIVE FAMILY HISTORY • ENVIRONMENTAL FACTORS • SERUM LEVELS OF IGE MAY BE ELEVATED IF ALLERGY IS PRESENT. • ARTERIAL BLOOD GAS ANALYSIS • PULSE OXIMETRY • HYPERCAPNIA AND RESPIRATORY ALKALOSIS ARE PRESENT. • AS THE PATIENT’S CONDITION WORSENS AND HE OR SHE BECOMES MORE FATIGUED, THE PACO2 MAY INCREASE. • LUNG FUNCTION IS EVALUATED BY SPIROMETRY.
- 11. ASSESSMENT • SPECIFIC QUESTIONS IN THE ASSESSMENT THAT MAY HELP TO EVALUATE THE INDIVIDUAL’S ASTHMA CONTROL INCLUDE:  HAS YOUR ASTHMA AWAKENED YOU AT NIGHT OR IN THE EARLY MORNING?  HAVE YOU NEEDED YOUR QUICK – ACTING RELIEF MEDICATION MORE THAN USUAL?  HAVE YOU NEEDED UNSCHEDULED CARE FOR YOUR ASTHMA?  HAS YOUR ASTHMA IMPACTED YOUR NORMAL ACTIVITIES AT SCHOOL/ WORK/ SPORTS?
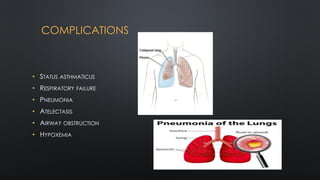
- 12. COMPLICATIONS • STATUS ASTHMATICUS • RESPIRATORY FAILURE • PNEUMONIA • ATELECTASIS • AIRWAY OBSTRUCTION • HYPOXEMIA
- 13. PREVENTION • AVOID SMOKE EXPOSURE EITHER THROUGH PASSIVE SMOKING OR ENVIRONMENTAL SMOKE, E.G., SMOKE FROM KEROSENE STOVE OR CHULLAH. • AVOID INDOOR ALLERGENS, E.G., BY AVOIDING PETS, CLEANING SOFT TOYS AND CONTROLLING HOUSE DUST MITE BY KEEPING CARPETS AND CURTAINS FREE OF DUST. • WET MOPPING OF FLOOR SHOULD BE DONE BECAUSE DRY DUSTING INCREASES EXPOSURE OF THE CHILD TO HOUSE DUST. • KEEP ROOMS WELL VENTILATED AND AVOID GROWTH OF MOLDS OR FUNGAL SPORES IN THE ROOMS BY PROMOTING GOOD VENTILATION AND CHECKING ANY SEEPAGE OR DAMPENING OF WALLS.
- 14. PREVENTION • AVOIDANCE OF OUTDOOR AIR POLLUTANTS. • AVOIDING EXPOSURE TO VERY COLD WEATHER AND STAYING INDOORS DURING VIRAL INFECTIONS. • PROMOTE PHYSICAL ACTIVITY, HEALTHY DIET AND WEIGHT REDUCTION FOR OBESE PATIENTS. • IMMUNIZATION SPECIALLY WITH PNEUMOCOCCAL AND INFLUENZA VACCINES.
- 15. DRUG THERAPY • THERE ARE THREE MAIN CATEGORIES OF MEDICATIONS FOR LONG TERM TREATMENT OF ASTHMA:
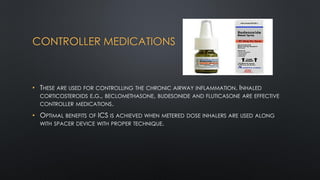
- 16. CONTROLLER MEDICATIONS • THESE ARE USED FOR CONTROLLING THE CHRONIC AIRWAY INFLAMMATION. INHALED CORTICOSTEROIDS E.G., BECLOMETHASONE, BUDESONIDE AND FLUTICASONE ARE EFFECTIVE CONTROLLER MEDICATIONS. • OPTIMAL BENEFITS OF ICS IS ACHIEVED WHEN METERED DOSE INHALERS ARE USED ALONG WITH SPACER DEVICE WITH PROPER TECHNIQUE.
- 17. RELIEVER MEDICATIONS • THESE ARE USED FOR AS- NEEDED RELIEF OF BREAKTHROUGH SYMPTOMS AND FOR SHORT TERM PREVENTION OF EXERCISE – INDUCED BRONCHOCONSTRICTION. • INHALED SHORT- ACTING BETA- AGONISTS ARE THE PREFERRED RELIEVER DRUGS OWING TO RAPID ONSET OF ACTION AND SAFETY PROFILE AS COMPARED TO ORAL ROUTE.
- 18. OTHER DRUGS • THESE MAY BE CONSIDERED AS AN ALTERNATIVE OR AS AN ADD ON DRUGS, E.G., LTRA ( LEUKOTRIENE RECEPTOR ANTAGONISTS, SUCH AS MONTELUKAST) OR THEOPHYLLINE. • LONG TERM PHARMACOLOGICAL TREATMENT IS BASED ON THE SYMPTOMS AND CLASSIFICATION OF ASTHMA .
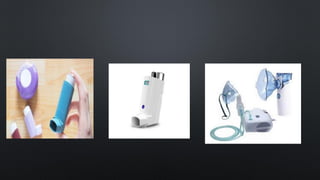
- 19. INHALATION DEVICES USED FOR ASTHMA • DRUGS USED BY THE INHALATION ROUTE ARE MORE EFFECTIVE AND HAVE RAPID ONSET OF ACTION, AND FEWER SIDE EFFECTS. • ALSO, SMALLER DRUG DOSES AS COMPARED TO ORAL ARE NEEDED TO ACHIEVE THE SAME PHARMACOLOGICAL EFFECT. • COMMONLY AVAILABLE INHALATION DEVICES INCLUDE METERED DOSE INHALERS, DRY POWDER INHALER (ROTA HALER), AND NEBULIZER.
- 21. STEPS FOR USING PMDIS WITH SPACER • REMOVE CAP, SHAKE INHALER AND INSERT INTO SPACER DEVICE. • PLACE MOUTHPIECE OF SPACER IN MOUTH. FOR YOUNGER KIDS, ATTACH THE BABY MASK AT THE MOUTH END OF THE SPACER AND COVER BABY’S MOUTH AND NOSE WITH BABY MASK. • START BREATHING IN AND OUT GENTLY. • ONCE THE BREATHING PATTERN IS ESTABLISHED, PRESS CANISTER AND TAKE 5-10 TIDAL BREATHS.
- 22. • REMOVE THE DEVICE FROM THE MOUTH AND WAIT FOR 30 SECONDS BEFORE REPEATING STEP 1-4. DON’T USE MULTIPLE ACTUATIONS AT A TIME. • RINSE MOUTH WITH WATER AFTER USING ICS TO PREVENT OROPHARYNGEAL DRUG DEPOSITION AND PREVENT ACCOMPANYING SIDE EFFECTS LIKE OROPHARYNGEAL CANDIDIASIS. • A NEW SPACER HAS STATIC CHARGES ON ITS PLASTIC SURFACE WHICH DEPOSITS THE DRUG ACTUATED IN THE CHAMBER. • TO PREVENT THIS, A NEW SPACER SHOULD BE PRE- WASHED WITH DETERGENT AND AIR- DRIED TO BE READY FOR USE. • DO NOT RINSE WITH WATER AFTER WASHING WITH DETERGENT. • WASH SPACER DEVICE ONCE WEEKLY WITH DETERGENT AND DO NOT RINSE WITH WATER AFTER WASHING WITH DETERGENT.
- 23. NEBULIZERS • NEBULIZER IS A DEVICE BY WHICH THE DRUG IS DELIVERED TO THE AIRWAYS IN FORM OF VERY SMALL DROPLETS. a. IF USING COMPRESSOR, PLUG THE COMPRESSOR INTO PROPERLY GROUNDED ELECTRIC SHOCK. b. THE REQUIRED AMOUNT OF DRUG IS DILUTED WITH NORMAL SALINE TO MAKE 3-5ML OF SOLUTION. DO NOT USE DISTILLED WATER FOR THIS PURPOSE AS HYPOTONIC SOLUTIONS MAY CAUSE REFLEX BRONCHOSPASM. c. THE RESPIRABLE RANGE OF AEROSOL PARTICLES ARE PRODUCED AT A FLOW OF 6-12L/MIN IN OXYGEN OR AIR DRIVEN DEVICES. d. IF USING MOUTHPIECE, SEAL THE LIPS AROUND IT AND ENCOURAGE CHILD TO BREATH THROUGH MOUTH . IF USING A MASK, PLACE IT OVER MASK AND NOSE TO MINIMIZE DRUG LOSS.
- 24. NEBULIZERS • TAPPING THE SIDE OF NEBULIZER CHAMBER DURING OPERATION INDUCES THE DROPLETS ON THE SIDES TO FALL BACK INTO THE RESERVOIRS; THIS MINIMIZES DRUG LOSS. • HOLD THE NEBULIZER CHAMBER UPRIGHT WHILE IN USE.
- 25. COUNSELING OF PARENTS • EXPLAINING THE WIDE- SPECTRUM OF THE DISEASE AND BUILDING CONFIDENCE IN PARENTS THAT THE ACTIVITY LIMITATION AND DISEASE CAN BE BROUGHT TO MINIMAL WITH TREATMENT PLAN. • IDENTIFICATION AND AVOIDANCE OF POTENTIAL TRIGGERS. • AVOIDANCE OF ALL KINDS OF SMOKE, E.G., TOBACCO AND BIOMASS SMOKE. • MAINTAINING ASTHMA DIARY AND BRING IT IN FOLLOW- UP VISITS. • PROPER EXPLANATION AND DEMONSTRATION OF USE OF MDI AND SPACER DEVICES. • IF POSSIBLE, MEASURE PEFR. • IDENTIFICATION AND HOME MANAGEMENT OF ASTHMA EXACERBATION. • WHEN TO SEEK HELP FROM HEALTHY FACILITY.
- 26. HOME TREATMENT OF ACUTE EXACERBATION • A WRITTEN ACTION PLAN SHOULD BE GIVEN TO PARENTS. i. GIVE 2 PUFFS OF INHALED SABA GIVEN ONE PUFF AT A TIME VIA A SPACER DEVICE. IT MAY BE REPEATED TWO MORE TIMES AT 20 MINUTES INTERVAL. ii. SEEK MEDICAL ATTENTION, IF > 6 PUFFS OF SABA ARE REQUIRED WITHIN THE FIRST TWO HOURS, OR THE CHILD HAS NOT RECOVERED AFTER 24 HOURS.