Back/Spine examination
44 likes12,217 views
Clinical examination notes of back/spine especially based on TU course of MBBS in Nepal.I hope many students will be helped with this notes.
1 of 15





Recommended
Clinical examination of spine



Clinical examination of spinePrasanthmuddada
Ěý
Detailed history and its evaluation , examination of spine in general and local with special tests in cervical , thoracic outlet syndrome , lumbar spine and SI joint with diagrams, neurological examination both sensory and motor. Sciatica



SciaticaFahad AlHulaibi
Ěý
Sciatica is pain that radiates from the lower back down the back of the thigh and leg. It is caused by irritation or compression of the sciatic nerve, which can occur due to herniated discs, spinal stenosis, spondylolisthesis, or other causes like tumors or infections. Symptoms include pain that is worsened by certain movements and activities, numbness, and difficulty walking. Diagnosis involves physical examination including straight leg raise testing and neurological evaluation, as well as imaging like MRI or CT scan. Treatment options include medications, physiotherapy, surgery such as laminectomy or removal of bone compressing the nerve.Sciatica



Sciaticaorthoprince
Ěý
Sciatica is a common radiating pain syndrome caused by irritation of the sciatic nerve root, usually from a herniated disc at L4-L5 or L5-S1. It presents as low back pain radiating down the back of the leg and can affect the foot. Sciatica is a symptom rather than a diagnosis. Examination may reveal a positive straight leg raise test. Differential diagnoses include spondyloarthropathies. Imaging like MRI can identify disc herniations while conservative treatments include rest, analgesics, and epidural injections. Surgery is considered if conservative options fail or neurological deficits are present.Low Back Pain 



Low Back Pain Shaheed Suhrawardy Medical College
Ěý
This document discusses low back pain, its causes, symptoms, and risk factors. It summarizes that low back pain can be caused by sensory, motor, or autonomic root involvement in the spine. Symptoms may include pain, numbness, muscle weakness, or loss of bladder/bowel control. Risk factors include age, gender, family history, previous injuries or surgery, pregnancy, or congenital spine problems. Some risk factors like smoking and weight can be modified, while others like age cannot. The document was prepared by Dr. Md Nazrul Islam for Incepta Pharmaceuticals Ltd. in Bangladesh.clinical examination of spine



clinical examination of spineHardik Pawar
Ěý
This document provides an overview of the clinical examination of the spine. It discusses the anatomy of the spine and common spinal conditions. The examination involves obtaining a history, inspecting the spine, palpating for tenderness, and assessing range of motion. Special tests like the straight leg raise test help localize pain and diagnose conditions like herniated discs. A neurological exam evaluates muscle strength, sensation, and reflexes to identify abnormalities affecting the spinal cord or nerves. A thorough spinal exam provides important clues for diagnosing underlying spinal problems.Examination of cervical disorder



Examination of cervical disorderDr Kaushal Kumar Sinha
Ěý
The document discusses the examination of cervical disorders. It begins with an introduction to the anatomy of the cervical spine and then describes the various functions of the spine. The document outlines the process for examining the cervical spine, including obtaining a history, inspecting for abnormalities, palpating the spine, and performing special tests to assess range of motion and potential nerve impingement. Common cervical conditions like herniated discs and bone spurs are also summarized. The examination techniques are explained in detail with diagrams to illustrate proper procedures like compression, distraction, and rotation tests.Knee examination



Knee examinationDhananjaya Sabat
Ěý
The document summarizes the process for examining the knee, including:
- Inspecting for alignment, masses, scars while standing or supine
- Palpating for temperature, tenderness, effusion, crepitus, strength
- Testing range of motion including flexion, extension, rotation
- Performing tests like McMurray's, Lachman, and valgus/varus stress to check for injuries to structures like the meniscus, ACL, MCL, and LCLHeel spur



Heel spurRafi Alshamrani
Ěý
A heel spur is a bony growth that forms on the heel bone (calcaneus). Heel spurs are common and often do not cause pain, but can cause pain when contacting soft tissue. They may be caused by pressure on the heel and associated with plantar fasciitis or Achilles tendinopathy. Treatment options include medications like NSAIDs, corticosteroid injections, physiotherapy including stretching, ultrasound, shockwave therapy, and night splints or orthotics.Tennis elbow



Tennis elbowsshssomsen
Ěý
Tennis elbow, also known as lateral epicondylitis, is an inflammation of the tendons on the outside of the elbow caused by repetitive motions like tennis, volleyball, or computer use. It causes pain on the outside of the elbow and weakness when grasping. Resting the elbow and avoiding aggravating activities for 2-3 weeks is the first treatment, along with icing, anti-inflammatory medication, and exercises to maintain flexibility and strength once healing begins.Examination of spine



Examination of spinegroup7usmkk
Ěý
This document provides instructions for examining the spine. It describes examining a patient's gait, standing posture, and range of motion of the cervical and thoracic spine through flexion, extension, lateral flexion, and rotation. Neurological examination of the upper and lower limbs assesses tone, power, reflexes, and sensation. Special tests like the straight leg raise test and sciatic stretch test evaluate for nerve root irritation.DERMATOMES AND MYOTOMES



DERMATOMES AND MYOTOMESDr.Monica Dhanani
Ěý
Dermatomes:- the sensory distribution of each nerve root is called the dermatomes.
The area of the skin supplied by a single nerve root
sciatica final.pptx



sciatica final.pptxShubham Shukla
Ěý
Sciatica is a sharp shooting pain in the lower extremity caused by irritation of the sciatic nerve. The pain is felt from the lower back down the back of the thigh and leg. Common causes include herniated discs, spinal stenosis, and spondylolisthesis. Symptoms include radiating pain, numbness, and tingling from the back through the leg. Diagnosis involves physical exams and imaging tests like MRI. Treatment focuses on self-care methods like stretching and pain medication.De quervain’s



De quervain’sDr. Akshita Duha Juneja (PT)
Ěý
De Quervain's tenosynovitis is an inflammation of the tendon sheaths of the abductor pollicis longus and extensor pollicis brevis muscles in the wrist. It commonly affects women ages 30-50 and is caused by repetitive motions like knitting or computer use that strain the thumb and wrist. Symptoms include pain on the radial side of the wrist worsened by thumb movement. Conservative treatment involves splinting, anti-inflammatories, corticosteroid injections, and physical therapy exercises. Surgery may be considered if symptoms persist after several weeks of conservative care.Low back pain



Low back painDebajyoti Chakraborty
Ěý
1) This document provides guidance on evaluating and differentiating the causes of low back pain through patient history, physical examination, and imaging.
2) The differential diagnosis depends on characteristics of the pain such as duration, location, radiation, and aggravating/relieving factors. Common etiologies include inflammatory, mechanical, and radicular causes.
3) The physical examination focuses on the spine, hips, and tests to reproduce pain including range of motion and provocative maneuvers. Red flags are identified.
4) Imaging like MRI can identify abnormalities in the discs, vertebrae, nerves and surrounding tissues that provide diagnostic clues. Both regular sequences and enhanced images after contrast are useful.Tests for shoulder joint



Tests for shoulder jointAarti Sareen
Ěý
This document discusses various special tests used to evaluate the shoulder joint. It provides details on range of motion tests and impingement tests for the rotator cuff as well as tests for the acromioclavicular joint, bicep tendon, and shoulder instability. Impingement is classified based on the cause and grade. Specific tests described include Neer's impingement test, Hawkins-Kennedy test, empty can test, and others. Tests for the acromioclavicular joint, biceps tendon, and shoulder instability include the painful arc test, Yergason test, anterior apprehension test, and more.AVASCULAR NECROSIS



AVASCULAR NECROSISPanchakarma Sdmcahhassan
Ěý
AVASCULAR NECROSIS
Presented by Dr Aparna Chapra ,PG Scholar, Department of Panchakarma, Panchakarma Sdmcah HassanClinical case presentation spine



Clinical case presentation spinesguruprasad311286
Ěý
This document presents two clinical case presentations of patients with back pain. The first case involves a 28-year-old male with low back pain radiating to his right leg. Diagnostic tests revealed a prolapsed intervertebral disc at L4-L5 with lumbar canal stenosis. He underwent a laminectomy with discectomy and experienced post-operative relief. The second case involves a 34-year-old male with low back pain radiating to his left leg. Diagnostic tests revealed a prolapsed disc at L4-L5 more pronounced on the left side. He underwent a laminotomy with micro-discectomy at L4-L5 and also experienced post-operative relief.Frozen shoulder



Frozen shoulderReinfried Haule
Ěý
Frozen shoulder, also known as adhesive capsulitis, is an inflammation condition of the shoulder characterized by progressive pain and stiffness leading to loss of motion. It affects 2-5% of the population between ages 40-65, more commonly in women. The condition involves three stages - a freezing phase with pain and loss of motion, a frozen phase with more stiffness, and a thawing phase where motion gradually returns over 1-3 years. Diagnosis is based on the clinical presentation of pain and reduced range of motion on physical exam. Treatment involves physical therapy, injections, medications and possibly surgery if conservative treatments fail to provide relief after 4 months.Cervical spondylosis.pptx



Cervical spondylosis.pptxRajveer71
Ěý
Cervical spondylosis is a degenerative condition affecting the cervical spine that commonly occurs with aging. As the cervical discs lose hydration and height, bone spurs and other degenerative changes can occur that result in compression of nerves or the spinal cord. While aging is the primary risk factor, repetitive neck movements from activities like texting or occupations involving manual labor can also contribute. Common symptoms include neck pain and stiffness, headaches, arm or hand numbness, weakness or tingling. Diagnosis involves physical examination and imaging tests like x-rays or MRI to identify the areas of involvement and damage.Assessment of cervical spine



Assessment of cervical spinekhushali52
Ěý
This document discusses the assessment of the cervical spine. It begins with an introduction to the anatomy and biomechanics of the cervical spine. It then describes taking a patient history, including questions about pain and symptoms. The examination involves observation, palpation, range of motion testing, muscle strength testing, sensory testing, and special tests like Spurling's test. Diagnostic imaging options like x-rays, CT scans, and MRI are also discussed.Radial nerve palsy



Radial nerve palsymanoj das
Ěý
The document provides information about the radial nerve including its anatomy, course, branches and clinical presentations of radial nerve palsies. It discusses the radial nerve's origin from the brachial plexus and branches in the arm and forearm. Common causes of radial nerve palsy include fractures and entrapment in the radial tunnel. Clinical features, investigations, treatment including splinting and tendon transfers, and postoperative management are outlined. Surgical techniques for nerve repair and reconstructive procedures are also described.Sciatica 



Sciatica Kagoga Rogers
Ěý
This condition,affects the back.thus back pain and if not attended to by health personal,leads to paralysis of lower limbs.Sensory Examination



Sensory Examinationmeducationdotnet
Ěý
The document discusses the sensory system and how it processes and transmits sensory information from peripheral receptors to the sensory cortex. It describes how different sensory modalities like pain, temperature, vibration and proprioception are carried by different nerve fiber types and pathways in the body. It provides details on testing various sensory modalities and how the patterns of sensory loss can help localize lesions to different parts of the central or peripheral nervous system.The Elbow, Examination



The Elbow, ExaminationSreeraj S R
Ěý
The document discusses the anatomy and examination of the elbow joint. It describes the elbow as a compound synovial joint made up of three joints: the ulnohumeral joint, radiohumeral joint, and superior radio ulnar joint. It provides details on the ligaments, muscles, movements, and common conditions that can be examined at the elbow. Specific tests for conditions like tennis elbow and golfer's elbow are also outlined.Lumbar Spondylosis, Spondylolisthesis and Radiculopathy



Lumbar Spondylosis, Spondylolisthesis and RadiculopathyShamadeep Kaur (PT)
Ěý
definition, causes, pathophysiology, clinical features, diagnosis and treatment (medical, surgical, and physiotherapy)Plantar fasciitis



Plantar fasciitismans4ani
Ěý
Plantar fasciitis is an inflammation of the plantar fascia in the foot that causes heel pain. It is caused by overuse from activities like long-distance running or tight calf muscles limiting the foot's range of motion. Symptoms include pain, swelling, and warmth in the heel area. Conservative treatments include stretching exercises, orthotics, night splints, taping, and manual therapies to increase flexibility and support the arch. Treatment may last several months to two years and surgery is an option for severe cases that do not improve.Osteoarthritis knee



Osteoarthritis kneeNarula Gandu
Ěý
This document provides an overview of osteoarthritis of the knee, including its definition, classification, epidemiology, anatomy, pathology, risk factors, diagnosis, grading, and management. Some key points are:
- Osteoarthritis is a degenerative joint condition characterized by cartilage breakdown and new bone growth. It commonly affects the knee joint.
- Risk factors include age, obesity, previous injury, activities like squatting that increase pressure on the knee.
- Diagnosis involves clinical exams, x-rays showing bone changes and loss of joint space, and ruling out other causes through tests.
- Treatment focuses on lifestyle changes like weight loss and exercise, medications, injections, and sometimes surgery like knee replacementShoulder examination 



Shoulder examination Dhananjaya Sabat
Ěý
Shoulder examination for orthopedic students; one of the famous lectures of MAMC PG course - over last 6 years.Spine examination



Spine examinationSachin Ranvir
Ěý
This document provides information on basic vertebral structures and techniques for examining the spine and extremities. It describes the normal curves of the cervical, thoracic, and lumbar spine. It outlines the main anatomical structures of vertebrae. It then details techniques for examining range of motion, tenderness, and deformities of the spine, as well as tests for examining nerve root function in the upper and lower extremities.hip joint



hip jointAmr Mansour Hassan
Ěý
The hip joint is a ball and socket joint that connects the femur to the pelvis. It has an articular capsule and several ligaments that provide stability. Important anatomical structures near the hip joint include nerves, blood vessels, and bursae. The hip allows flexion, extension, abduction, adduction, internal and external rotation. Examination of the hip evaluates gait, range of motion, special tests like Trendelenburg sign, and imaging may be used.More Related Content
What's hot (20)
Tennis elbow



Tennis elbowsshssomsen
Ěý
Tennis elbow, also known as lateral epicondylitis, is an inflammation of the tendons on the outside of the elbow caused by repetitive motions like tennis, volleyball, or computer use. It causes pain on the outside of the elbow and weakness when grasping. Resting the elbow and avoiding aggravating activities for 2-3 weeks is the first treatment, along with icing, anti-inflammatory medication, and exercises to maintain flexibility and strength once healing begins.Examination of spine



Examination of spinegroup7usmkk
Ěý
This document provides instructions for examining the spine. It describes examining a patient's gait, standing posture, and range of motion of the cervical and thoracic spine through flexion, extension, lateral flexion, and rotation. Neurological examination of the upper and lower limbs assesses tone, power, reflexes, and sensation. Special tests like the straight leg raise test and sciatic stretch test evaluate for nerve root irritation.DERMATOMES AND MYOTOMES



DERMATOMES AND MYOTOMESDr.Monica Dhanani
Ěý
Dermatomes:- the sensory distribution of each nerve root is called the dermatomes.
The area of the skin supplied by a single nerve root
sciatica final.pptx



sciatica final.pptxShubham Shukla
Ěý
Sciatica is a sharp shooting pain in the lower extremity caused by irritation of the sciatic nerve. The pain is felt from the lower back down the back of the thigh and leg. Common causes include herniated discs, spinal stenosis, and spondylolisthesis. Symptoms include radiating pain, numbness, and tingling from the back through the leg. Diagnosis involves physical exams and imaging tests like MRI. Treatment focuses on self-care methods like stretching and pain medication.De quervain’s



De quervain’sDr. Akshita Duha Juneja (PT)
Ěý
De Quervain's tenosynovitis is an inflammation of the tendon sheaths of the abductor pollicis longus and extensor pollicis brevis muscles in the wrist. It commonly affects women ages 30-50 and is caused by repetitive motions like knitting or computer use that strain the thumb and wrist. Symptoms include pain on the radial side of the wrist worsened by thumb movement. Conservative treatment involves splinting, anti-inflammatories, corticosteroid injections, and physical therapy exercises. Surgery may be considered if symptoms persist after several weeks of conservative care.Low back pain



Low back painDebajyoti Chakraborty
Ěý
1) This document provides guidance on evaluating and differentiating the causes of low back pain through patient history, physical examination, and imaging.
2) The differential diagnosis depends on characteristics of the pain such as duration, location, radiation, and aggravating/relieving factors. Common etiologies include inflammatory, mechanical, and radicular causes.
3) The physical examination focuses on the spine, hips, and tests to reproduce pain including range of motion and provocative maneuvers. Red flags are identified.
4) Imaging like MRI can identify abnormalities in the discs, vertebrae, nerves and surrounding tissues that provide diagnostic clues. Both regular sequences and enhanced images after contrast are useful.Tests for shoulder joint



Tests for shoulder jointAarti Sareen
Ěý
This document discusses various special tests used to evaluate the shoulder joint. It provides details on range of motion tests and impingement tests for the rotator cuff as well as tests for the acromioclavicular joint, bicep tendon, and shoulder instability. Impingement is classified based on the cause and grade. Specific tests described include Neer's impingement test, Hawkins-Kennedy test, empty can test, and others. Tests for the acromioclavicular joint, biceps tendon, and shoulder instability include the painful arc test, Yergason test, anterior apprehension test, and more.AVASCULAR NECROSIS



AVASCULAR NECROSISPanchakarma Sdmcahhassan
Ěý
AVASCULAR NECROSIS
Presented by Dr Aparna Chapra ,PG Scholar, Department of Panchakarma, Panchakarma Sdmcah HassanClinical case presentation spine



Clinical case presentation spinesguruprasad311286
Ěý
This document presents two clinical case presentations of patients with back pain. The first case involves a 28-year-old male with low back pain radiating to his right leg. Diagnostic tests revealed a prolapsed intervertebral disc at L4-L5 with lumbar canal stenosis. He underwent a laminectomy with discectomy and experienced post-operative relief. The second case involves a 34-year-old male with low back pain radiating to his left leg. Diagnostic tests revealed a prolapsed disc at L4-L5 more pronounced on the left side. He underwent a laminotomy with micro-discectomy at L4-L5 and also experienced post-operative relief.Frozen shoulder



Frozen shoulderReinfried Haule
Ěý
Frozen shoulder, also known as adhesive capsulitis, is an inflammation condition of the shoulder characterized by progressive pain and stiffness leading to loss of motion. It affects 2-5% of the population between ages 40-65, more commonly in women. The condition involves three stages - a freezing phase with pain and loss of motion, a frozen phase with more stiffness, and a thawing phase where motion gradually returns over 1-3 years. Diagnosis is based on the clinical presentation of pain and reduced range of motion on physical exam. Treatment involves physical therapy, injections, medications and possibly surgery if conservative treatments fail to provide relief after 4 months.Cervical spondylosis.pptx



Cervical spondylosis.pptxRajveer71
Ěý
Cervical spondylosis is a degenerative condition affecting the cervical spine that commonly occurs with aging. As the cervical discs lose hydration and height, bone spurs and other degenerative changes can occur that result in compression of nerves or the spinal cord. While aging is the primary risk factor, repetitive neck movements from activities like texting or occupations involving manual labor can also contribute. Common symptoms include neck pain and stiffness, headaches, arm or hand numbness, weakness or tingling. Diagnosis involves physical examination and imaging tests like x-rays or MRI to identify the areas of involvement and damage.Assessment of cervical spine



Assessment of cervical spinekhushali52
Ěý
This document discusses the assessment of the cervical spine. It begins with an introduction to the anatomy and biomechanics of the cervical spine. It then describes taking a patient history, including questions about pain and symptoms. The examination involves observation, palpation, range of motion testing, muscle strength testing, sensory testing, and special tests like Spurling's test. Diagnostic imaging options like x-rays, CT scans, and MRI are also discussed.Radial nerve palsy



Radial nerve palsymanoj das
Ěý
The document provides information about the radial nerve including its anatomy, course, branches and clinical presentations of radial nerve palsies. It discusses the radial nerve's origin from the brachial plexus and branches in the arm and forearm. Common causes of radial nerve palsy include fractures and entrapment in the radial tunnel. Clinical features, investigations, treatment including splinting and tendon transfers, and postoperative management are outlined. Surgical techniques for nerve repair and reconstructive procedures are also described.Sciatica 



Sciatica Kagoga Rogers
Ěý
This condition,affects the back.thus back pain and if not attended to by health personal,leads to paralysis of lower limbs.Sensory Examination



Sensory Examinationmeducationdotnet
Ěý
The document discusses the sensory system and how it processes and transmits sensory information from peripheral receptors to the sensory cortex. It describes how different sensory modalities like pain, temperature, vibration and proprioception are carried by different nerve fiber types and pathways in the body. It provides details on testing various sensory modalities and how the patterns of sensory loss can help localize lesions to different parts of the central or peripheral nervous system.The Elbow, Examination



The Elbow, ExaminationSreeraj S R
Ěý
The document discusses the anatomy and examination of the elbow joint. It describes the elbow as a compound synovial joint made up of three joints: the ulnohumeral joint, radiohumeral joint, and superior radio ulnar joint. It provides details on the ligaments, muscles, movements, and common conditions that can be examined at the elbow. Specific tests for conditions like tennis elbow and golfer's elbow are also outlined.Lumbar Spondylosis, Spondylolisthesis and Radiculopathy



Lumbar Spondylosis, Spondylolisthesis and RadiculopathyShamadeep Kaur (PT)
Ěý
definition, causes, pathophysiology, clinical features, diagnosis and treatment (medical, surgical, and physiotherapy)Plantar fasciitis



Plantar fasciitismans4ani
Ěý
Plantar fasciitis is an inflammation of the plantar fascia in the foot that causes heel pain. It is caused by overuse from activities like long-distance running or tight calf muscles limiting the foot's range of motion. Symptoms include pain, swelling, and warmth in the heel area. Conservative treatments include stretching exercises, orthotics, night splints, taping, and manual therapies to increase flexibility and support the arch. Treatment may last several months to two years and surgery is an option for severe cases that do not improve.Osteoarthritis knee



Osteoarthritis kneeNarula Gandu
Ěý
This document provides an overview of osteoarthritis of the knee, including its definition, classification, epidemiology, anatomy, pathology, risk factors, diagnosis, grading, and management. Some key points are:
- Osteoarthritis is a degenerative joint condition characterized by cartilage breakdown and new bone growth. It commonly affects the knee joint.
- Risk factors include age, obesity, previous injury, activities like squatting that increase pressure on the knee.
- Diagnosis involves clinical exams, x-rays showing bone changes and loss of joint space, and ruling out other causes through tests.
- Treatment focuses on lifestyle changes like weight loss and exercise, medications, injections, and sometimes surgery like knee replacementShoulder examination 



Shoulder examination Dhananjaya Sabat
Ěý
Shoulder examination for orthopedic students; one of the famous lectures of MAMC PG course - over last 6 years.Similar to Back/Spine examination (20)
Spine examination



Spine examinationSachin Ranvir
Ěý
This document provides information on basic vertebral structures and techniques for examining the spine and extremities. It describes the normal curves of the cervical, thoracic, and lumbar spine. It outlines the main anatomical structures of vertebrae. It then details techniques for examining range of motion, tenderness, and deformities of the spine, as well as tests for examining nerve root function in the upper and lower extremities.hip joint



hip jointAmr Mansour Hassan
Ěý
The hip joint is a ball and socket joint that connects the femur to the pelvis. It has an articular capsule and several ligaments that provide stability. Important anatomical structures near the hip joint include nerves, blood vessels, and bursae. The hip allows flexion, extension, abduction, adduction, internal and external rotation. Examination of the hip evaluates gait, range of motion, special tests like Trendelenburg sign, and imaging may be used.Musculoskeletal examination 



Musculoskeletal examination vijayalakshminashipu
Ěý
This document provides guidance on performing a musculoskeletal examination. It outlines examining the joints, spine, and other areas in 3 stages: collecting subjective information like pain history, performing an objective physical examination, and assessing range of motion. Key parts of the exam are described, including inspection, palpation, and testing movements of joints like the shoulder, elbow, wrist, hip, knee, ankle, and spine. Specific tests are explained to evaluate ligaments, tendons, and nerves for injuries or conditions. The overall goal is to accurately diagnose musculoskeletal issues, determine severity, and develop a treatment plan.M S Examination.pptx



M S Examination.pptxvijayalakshminashipu
Ěý
This document provides guidance on performing a musculoskeletal examination. It outlines examining the joints, spine, and other areas in 3 stages: collecting subjective information like pain history, performing an objective physical examination, and assessing range of motion. Key steps are described, such as inspecting alignment, palpating for abnormalities, and testing specific movements to evaluate joints like the shoulder, elbow, wrist, hip, knee, and ankle. Special tests are also outlined to help diagnose conditions like tennis elbow or impingement. The overall goal is to accurately assess musculoskeletal symptoms, severity, and develop a treatment plan.Leg&Foot 2



Leg&Foot 2jo Han
Ěý
The document describes several muscles in the lower leg and their functions, including the triceps surae (gastrocnemius and soleus), plantaris, tibialis anterior, peroneus longus and brevis. It provides details on the origin, insertion, innervation and actions of each muscle, as well as instructions for palpating and testing each one through specific movements and positions of the leg and foot.Hip examination



Hip examinationOxford University Clinical Research Unit, Patan Academy of Health Sciences
Ěý
Clinical notes for step wise approach to hip examination in orthopaedic especially to TU/KU MBBS students of nepal.Clinical approch to rheumatological examination



Clinical approch to rheumatological examinationAshraf Okba
Ěý
This document provides guidance on performing a rheumatological examination, including inspection, palpation, and testing range of motion of various joints. The examination involves assessing gait, the upper and lower limbs, shoulders, elbows, wrists, hips, knees, ankles and feet, spine, and temporomandibular joint. For each body part, the document outlines what to inspect for, how to palpate for tenderness and swelling, and which movements to test. The goal is to identify any abnormalities, deformities, limitations in range of motion, or sites of tenderness that could indicate rheumatological conditions.Examination of hip,final



Examination of hip,finalDrSiddique H. Ranna
Ěý
This document provides guidance on examining the hip joint. It outlines the key steps which include: obtaining history regarding pain, swelling, limping etc.; inspecting gait, limb position, and bony landmarks; palpating areas for tenderness; performing range of motion tests for flexion, extension, rotation; assessing limb length with measurements; and conducting special tests for stability and pathology. Proper examination of the hip joint requires understanding patient history, performing a thorough physical exam of the joint and related structures, and using special tests to analyze function and identify potential causes of hip problems.Examination of hip joint



Examination of hip jointDrSiddique H. Ranna
Ěý
1) The document discusses the process for examining a patient's hip joint, including obtaining history, performing physical examination, and conducting specific tests.
2) The physical examination involves inspecting the hip from various angles, palpating bony landmarks and soft tissues, measuring range of motion, assessing limb length and muscle bulk, and performing stability and special tests.
3) A number of special tests are described that can help identify conditions like labral tears, femoral anteversion, and soft tissue contractures. Taking a thorough history and conducting a complete physical exam are important for accurately diagnosing hip joint pathology.Physical examination signs



Physical examination signscoolboy101pk
Ěý
The document provides descriptions of various physical examination tests for different parts of the body including the low back, cervical spine, shoulder, knee, and other areas. It describes how to perform tests like the straight leg raise test for the low back, Spurling's test and cervical distraction for the cervical spine, Neer's impingement sign and Hawkins-Kennedy test for the shoulder, Lachman test and posterior drawer test for the knee ligaments, and McMurray's test for the meniscus. The tests are used to evaluate for conditions like nerve root irritation, radiculopathy, impingement, and ligament injuries.Knee Examination.pptx



Knee Examination.pptxMohammedAli666017
Ěý
This document provides guidance on performing a thorough knee examination. It outlines steps to look, feel, move, and perform special tests on the knee to identify various injuries and conditions. The look section describes examining alignment, swelling, and other visual indicators. The feel section details palpating areas like the joint line, patella, and ligaments. Special tests are described to check the meniscus, collateral ligaments, cruciate ligaments, and other structures. It emphasizes comparing both knees and considering referrals from other joints.Knee examination



Knee examinationOxford University Clinical Research Unit, Patan Academy of Health Sciences
Ěý
Clinical examination notes based on TU/KU curriculum of MBBS in nepal. Hope this will be very much helpful in step wise approach to you people especially during exam time.examinationofhipjoint-170820154603 edited.docx



examinationofhipjoint-170820154603 edited.docxprashant372004
Ěý
This document provides guidance on examining the hip joint, including:
- Taking a thorough history regarding pain, swelling, limping, stiffness, and past medical history.
- Performing an inspection of gait, limb position, and bony landmarks.
- Conducting palpation of areas for tenderness and deep structures.
- Assessing range of motion through specific movements and tests.
- Measuring for limb length discrepancies, deformities, and muscle wasting.
- Testing stability, special maneuvers for detecting injuries, and contractures.Musculoskeletal System



Musculoskeletal SystemGovernors State University
Ěý
The document provides guidance on performing a musculoskeletal assessment, including relevant history, inspection, palpation, range of motion testing, muscle testing, and tests for common joint abnormalities. It discusses assessing the cervical spine, shoulders, elbows, wrists, hips, knees, ankles, and feet. It also covers age-specific considerations for infants, children, adolescents, pregnant females, and aging adults.5759407.ppt



5759407.pptamj20008
Ěý
1. The document describes various orthopedic tests used to evaluate common shoulder conditions like tendinitis, bursitis, instability, and rotator cuff and biceps tendon injuries.
2. Key tests include tests for supraspinatus tendinitis like the painful arc test, and tests for bicipital tendinitis like Speed's test and Lippman's test.
3. Other tests evaluate subacromial bursitis, anterior and posterior shoulder instability, rotator cuff tears using the drop arm test, and biceps tendon instability with Yergason's test and Abbott-Saunders test.5759407.ppt



5759407.pptamj20008
Ěý
This document describes various orthopedic tests for evaluating shoulder conditions like tendinitis, bursitis, instability, and rotator cuff and biceps tendon injuries. Key tests include the Neer impingement test for overuse injuries, the drop arm test for rotator cuff tears, and Yergason's test and Abbott-Saunders test for biceps tendon subluxation or rupture. Positive findings on physical exam combined with the patient's history and symptoms can help diagnose underlying shoulder issues.5759407.ppt



5759407.pptamj20008
Ěý
This document describes various orthopedic tests for evaluating shoulder conditions like tendinitis, bursitis, instability, and rotator cuff and biceps tendon injuries. Key tests include the Neer impingement test for overuse injuries, the anterior apprehension test for anterior dislocations, Speed's test for biceps tendinitis, and the drop arm test for rotator cuff tears. Positive findings on these physical exams, such as pain or weakness, help diagnose underlying shoulder issues.pft-training-Part-I-HRF-Revised PFT.pptx



pft-training-Part-I-HRF-Revised PFT.pptxMELANIEZARATE4
Ěý
This document provides information on assessing various components of physical fitness, including body composition, flexibility, strength, and cardiovascular endurance. It describes tests to measure each component and how to interpret the results. The tests included are body mass index, waist circumference, zipper test, sit-and-reach, push-ups, plank, and step test. Scoring methods and standards for each test are provided to determine if a person's fitness level is excellent, very good, good, fair, or needs improvement. The document aims to outline a revised physical fitness test that measures health-related aspects of physical fitness.Case presentation 221(2) sandamail



Case presentation 221(2) sandamailAyaz Iqbal
Ěý
This document contains a physiotherapy assessment and treatment plan for a 62-year-old female presenting with neck pain radiating to her arm. The assessment revealed reduced cervical range of motion, tenderness over the cervical spine, and positive orthopedic tests indicating nerve root compression. X-rays showed reduced disc spaces and osteophytes. The treatment plan includes shortwave diathermy, cervical traction, soft tissue techniques, range of motion exercises, and strengthening to reduce pain and muscle tightness, improve range of motion, and restore normal function. Progress will be measured by pain scale and improved cervical range of motion.Recently uploaded (20)
MLS 208 - UNIT 4 A - Tissue Processing - ETANDO AYUK - SANU 1 - Secured.pdf



MLS 208 - UNIT 4 A - Tissue Processing - ETANDO AYUK - SANU 1 - Secured.pdfEswatini Medical Christian University - EMCU / Southern Nazarene University - SANU
Ěý
The course covers the steps undertaken from tissue collection, reception, fixation,
sectioning, tissue processing and staining. It covers all the general and special
techniques in histo/cytology laboratory. This course will provide the student with the
basic knowledge of the theory and practical aspect in the diagnosis of tumour cells
and non-malignant conditions in body tissues and for cytology focusing on
gynaecological and non-gynaecological samples.PRODUCTION OF HB VACCINE AND INTERFERONS BY rDNA - Copy.pptx



PRODUCTION OF HB VACCINE AND INTERFERONS BY rDNA - Copy.pptxkarishmaduhijod1
Ěý
APPLICATION of RECOMBINANAT DNA TECHNOLOGY : IN THE PRODUCTION OF HEPATITIS B VACCINE ,INSULIN and INTERFERONHUMAN SEXUALITY AND SEXUAL RESPONCE CYCLE



HUMAN SEXUALITY AND SEXUAL RESPONCE CYCLEdaminipatel37
Ěý
It is all about topic of obg for new semester students HER2-Targeting Therapy in HER2+ MBC With and Without CNS Metastases: Selectio...



HER2-Targeting Therapy in HER2+ MBC With and Without CNS Metastases: Selectio...PVI, PeerView Institute for Medical Education
Ěý
Chair and Presenters Sara A. Hurvitz, MD, FACP, Carey K. Anders, MD, FASCO, and Vyshak Venur, MD, discuss metastatic HER2-positive breast cancer in this CME/NCPD/CPE/AAPA/IPCE activity titled “Fine-Tuning the Selection and Sequencing of HER2-Targeting Therapies in HER2-Positive MBC With and Without CNS Metastases: Expert Guidance on How to Individualize Therapy Based on Latest Evidence, Disease Features, Treatment Characteristics, and Patient Needs and Preferences.” For the full presentation, downloadable Practice Aids, and complete CME/NCPD/CPE/AAPA/IPCE information, and to apply for credit, please visit us at https://bit.ly/4f8sUs7. CME/NCPD/CPE/AAPA/IPCE credit will be available until March 2, 2026.MLS 208 - UNIT 1- Lecture Notes - ETANDO AYUK - SANU - Secured.pdf



MLS 208 - UNIT 1- Lecture Notes - ETANDO AYUK - SANU - Secured.pdfEswatini Medical Christian University - EMCU / Southern Nazarene University - SANU
Ěý
Unit 1: Introduction to Histological and Cytological techniques
ď‚· Differentiate histology and cytology
ď‚· Overview on tissue types
ď‚· Function and components of the compound light microscope
ď‚· Overview on common Histological Techniques:
o Fixation
o Grossing
o Tissue processing
o Microtomy
o Staining
o Mounting
ď‚· Application of histology and cytologyOne Health Rabies Control in Indonesia_APCAT meeting May 2022.pptx



One Health Rabies Control in Indonesia_APCAT meeting May 2022.pptxWahid Husein
Ěý
What is FAO doing to support rabies control programmes in Indonesia using One Health approachMultimodal Approaches to Clitoral Augmentation for FGM (PRP _ filler)"



Multimodal Approaches to Clitoral Augmentation for FGM (PRP _ filler)"Rehab Aboshama
Ěý
Multimodal Approaches to Clitoral Augmentation for FGM (PRP _ filler)"
Solubilization in Pharmaceutical Sciences: Concepts, Mechanisms & Enhancement...



Solubilization in Pharmaceutical Sciences: Concepts, Mechanisms & Enhancement...KHUSHAL CHAVAN
Ěý
This presentation provides an in-depth understanding of solubilization and its critical role in pharmaceutical formulations. It covers:
Definition & Mechanisms of Solubilization
Role of surfactants, micelles, and bile salts in drug solubility
Factors affecting solubilization (pH, polarity, particle size, temperature, etc.)
Methods to enhance drug solubility (Buffers, Co-solvents, Surfactants, Complexation, Solid Dispersions)
Advanced approaches (Polymorphism, Salt Formation, Co-crystallization, Prodrugs)
This resource is valuable for pharmaceutical scientists, formulation experts, regulatory professionals, and students interested in improving drug solubility and bioavailability.Biography of Dr. Vincenzo Giordano



Biography of Dr. Vincenzo GiordanoDr. Vincenzo Giordano
Ěý
Dr. Vincenzo Giordano began his medical career 2011 at Aberdeen Royal Infirmary in the Department of Cardiothoracic Surgery. Here, he performed complex adult cardiothoracic surgical procedures, significantly enhancing his proficiency in patient critical care, as evidenced by his FCCS certification.The influence of birth companion in mother care and neonatal outcome



The influence of birth companion in mother care and neonatal outcomeLokesh Kumar Sharma
Ěý
this content related to birth companionship, role of birth companion in care of mother and neonatal Eye assessment in polytrauma for undergraduates.pptx



Eye assessment in polytrauma for undergraduates.pptxKafrELShiekh University
Ěý
Eye assessment in polytrauma for undergraduates.Rabies Bali 2008-2020_WRD Webinar_WSAVA 2020_Final.pptx



Rabies Bali 2008-2020_WRD Webinar_WSAVA 2020_Final.pptxWahid Husein
Ěý
A decade of rabies control programmes in Bali with support from FAO ECTAD Indonesia with Mass Dog Vaccination, Integrated Bite Case Management, Dog Population Management, and Risk Communication as the backbone of the programmesISPE Baseline PEG Volumen 7 Risk-Based Manufacture Pharmaceutical Products 2n...



ISPE Baseline PEG Volumen 7 Risk-Based Manufacture Pharmaceutical Products 2n...alokksharma18
Ěý
guidelines for pharma productsNon-Invasive ICP Monitoring for Neurosurgeons



Non-Invasive ICP Monitoring for NeurosurgeonsDhaval Shukla
Ěý
This presentation delves into the latest advancements in non-invasive intracranial pressure (ICP) monitoring techniques, specifically tailored for neurosurgeons. It covers the importance of ICP monitoring in clinical practice, explores various non-invasive methods, and discusses their accuracy, reliability, and clinical applications. Attendees will gain insights into the benefits of non-invasive approaches over traditional invasive methods, including reduced risk of complications and improved patient outcomes. This comprehensive overview is designed to enhance the knowledge and skills of neurosurgeons in managing patients with neurological conditions.
Invasive systems are commonly used for monitoring intracranial pressure (ICP) in traumatic brain injury (TBI) and are considered the gold standard. The availability of invasive ICP monitoring is heterogeneous, and in low- and middle-income settings, these systems are not routinely employed due to high cost or limited accessibility. The aim of this presentation is to develop recommendations to guide monitoring and ICP-driven therapies in TBI using non-invasive ICP (nICP) systems.
Best Sampling Practices Webinar – USP <797> Compliance & Environmental Monito...



Best Sampling Practices Webinar – USP <797> Compliance & Environmental Monito...NuAire
Ěý
Best Sampling Practices Webinar – USP <797> Compliance & Environmental Monitoring
Are your cleanroom sampling practices USP <797> compliant? This webinar, hosted by Pharmacy Purchasing & Products (PP&P Magazine) and sponsored by NuAire, features microbiology expert Abby Roth discussing best practices for surface & air sampling, data analysis, and compliance.
đź’ˇ Key Topics Covered:
✔️ Viable air & surface sampling best practices
✔️ USP <797> requirements & compliance strategies
✔️ How to analyze & trend viable sample data
✔️ Improving environmental monitoring in cleanrooms
🎥 Watch Now: https://www.nuaire.com/resources/best-sampling-practices-cleanroom-usp-797
📢 Stay informed—follow Abby Roth on LinkedIn for more cleanroom insights!MLS 208 - UNIT 4 A - Tissue Processing - ETANDO AYUK - SANU 1 - Secured.pdf



MLS 208 - UNIT 4 A - Tissue Processing - ETANDO AYUK - SANU 1 - Secured.pdfEswatini Medical Christian University - EMCU / Southern Nazarene University - SANU
Ěý
HER2-Targeting Therapy in HER2+ MBC With and Without CNS Metastases: Selectio...



HER2-Targeting Therapy in HER2+ MBC With and Without CNS Metastases: Selectio...PVI, PeerView Institute for Medical Education
Ěý
MLS 208 - UNIT 1- Lecture Notes - ETANDO AYUK - SANU - Secured.pdf



MLS 208 - UNIT 1- Lecture Notes - ETANDO AYUK - SANU - Secured.pdfEswatini Medical Christian University - EMCU / Southern Nazarene University - SANU
Ěý
Back/Spine examination
- 1. Back/Spine Examination Prepared by: Sunil Baniya Student, NAIHS-COM, sanobharyang, ktm, Nepal 1Knee Examination/ Sunil Baniya
- 2. • Adequate exposure is essential; patients must strip to their underclothes • Examination in standing, sittting and supine examination 1. LOOK – Gait Front – Posture – Forward bending – Lateral list
- 3. – Asymmetry of chest, pelvis – Scars, sinus – Leg shortening – Side – Kyphosis – Lordosis – Scars, sinus
- 4. Back - Tufts of hair - Café au laits spots - Paraspinal muscle spasm - Scars - Muscle wasting - scoliosis
- 5. 2. FEEL a. Temperature b. Tenderness: – Elicit spine tenderness by 3 methods i) Pressure over the interspinous area ii) Twisting or pressure over the paraspinous part (facet joint) = Spinous Rock iii) Thumping over vertebral column
- 6. 3. MOVE o Forward flexion: - Touching toes - Majority touches the ground - Touching mid tibia, 7 cm above the floor o Extension: normally 30° o Lateral flexion: try to touch each side of leg (Average = 30°) o Rotation: maximum 40° (first fix pelvis then only ask for rotation)
- 7. 4. MEASUREMENT: o To measure the lumbar excursion o Take any two bony points over the lumbar region 10 cm apart while standing upright o Measure the distance between that points when patient is asked to bend forward fully o The distance must be increased by at least 5 cm (i.e; lumbar excursion = 5cm) o If less than 3 cm, substantial pathology like ankylosing spondylitis
- 8. SPECIAL TESTS: 1. SLRT (Straight Leg Raising Test)/Sciatic stretch test/ Dural tension test 2. Well Leg Raise Test or Cross SLRT test 3. Bragard test 4. Lassegue’s test 5. Bowstring’s test 6. Patric test ( Faber sign) = for sacroiliac pathology
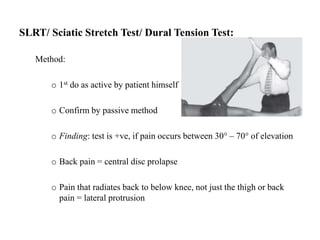
- 9. SLRT/ Sciatic Stretch Test/ Dural Tension Test: Method: o 1st do as active by patient himself o Confirm by passive method o Finding: test is +ve, if pain occurs between 30° – 70° of elevation o Back pain = central disc prolapse o Pain that radiates back to below knee, not just the thigh or back pain = lateral protrusion
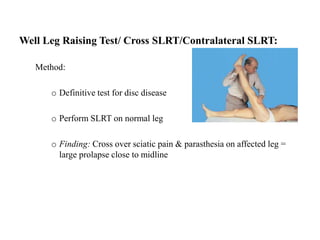
- 10. Well Leg Raising Test/ Cross SLRT/Contralateral SLRT: Method: o Definitive test for disc disease o Perform SLRT on normal leg o Finding: Cross over sciatic pain & parasthesia on affected leg = large prolapse close to midline
- 11. Bragard Test: Method: o Sciatic nerve stretch test o If SLRT +ve, leg lowered about 10° from the point of sciatic pain o Foot is dorsiflexed to reproduce the same pain
- 12. Lasegue’s Test: Method: o Patient supine o Thigh bent at 90° & knee bent at 90° o Gradually extend the knee keeping hip flexed o Thigh pain radiates down the leg = +ve
- 13. Bowstring’s Test: Method: o SLRT +ve o Slight flex the knee just to relieve pain o Then firmly press behind lateral hamstrings to tighten the common peroneal nerve o Radiating pain & parasthesia reappears o Finding: +ve Bowstring’s sign i.e; nerve root irritation
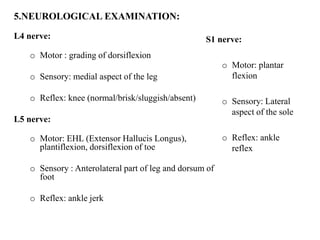
- 14. 5.NEUROLOGICAL EXAMINATION: L4 nerve: o Motor : grading of dorsiflexion o Sensory: medial aspect of the leg o Reflex: knee (normal/brisk/sluggish/absent) L5 nerve: o Motor: EHL (Extensor Hallucis Longus), plantiflexion, dorsiflexion of toe o Sensory : Anterolateral part of leg and dorsum of foot o Reflex: ankle jerk S1 nerve: o Motor: plantar flexion o Sensory: Lateral aspect of the sole o Reflex: ankle reflex
- 15. THANK YOU 15Knee Examination/ Sunil Baniya

![musculoskeletal_system_examination[1] (1) (3).pptx](https://cdn.slidesharecdn.com/ss_thumbnails/musculoskeletalsystemexamination113-241005064436-de0b77f1-thumbnail.jpg?width=560&fit=bounds)




