basal cell carcinoma
- 1. Ěý
- 2. Basal cell carcinoma Bhavishya Valder
- 3. Epidemiology Most common human cancer(~80-90%) 600,000 to 800,000 cases per year in U.S. Male:Female 2-3:1 80% arise in head and neck Age âś” Likelihood increases with age âś” BCCa over 40 years old Race âś” Most often in light-skinned, rare in dark-skinned races
- 4. Etiology Ultraviolet radiation ethnicity ionizing radiation exposure chemical exposure - arsenic burns, scarring immunosuppression
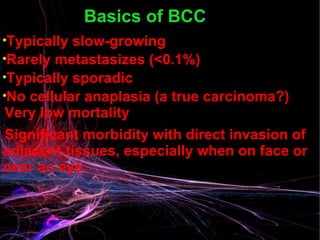
- 5. Basics of BCC Typically slow-growing Rarely metastasizes (<0.1%) Typically sporadic No cellular anaplasia (a true carcinoma?) Very low mortality Significant morbidity with direct invasion of adjacent tissues, especially when on face or near an eye
- 6. Classic presentation of basal cell
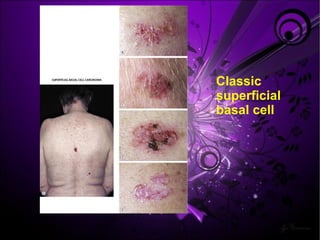
- 7. Classic superficial basal cell
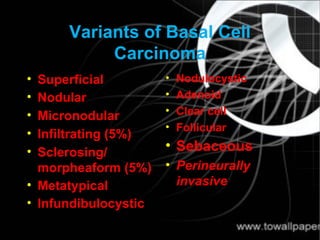
- 8. Variants of Basal Cell Carcinoma Superficial Nodular Micronodular Infiltrating (5%) Sclerosing/ morpheaform (5%) Metatypical Infundibulocystic Nodulocystic Adenoid Clear cell Follicular Sebaceous Perineurally invasive
- 9. Types of BCC Nodular Basosquamous © Schofield JK and Kneebone R (2006) Skin lesions: a practical guide to diagnosis management and minor surgery. Superficial Pigmented Morphoeic © dermNetNZ.org (http://dermnetnz.org)
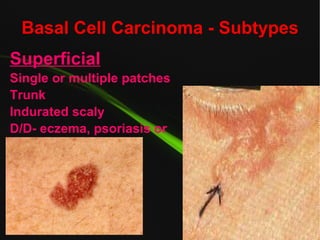
- 10. Basal Cell Carcinoma - Subtypes Superficial Single or multiple patches Trunk Indurated scaly D/D- eczema, psoriasis or tinea .
- 11. Basal Cell Carcinoma - Subtypes Nodular Ulcerative Most common Usually on the face Small, slow growing Firm Telangectasias Ulceration
- 12. Basal Cell Carcinoma - Subtypes Sclerosing (Morpheaform) Yellow white plaques Ill defined boarders Most aggressive Most likely to recur Central sclerosis & scarring
- 13. Basal Cell Carcinoma - Subtypes Pigmented Similar to nodular type Deep brown pigmentation Differential- malignant melanoma
- 14. Basal Cell Carcinoma - Subtypes FIBROEPITHELIOMA PINKUS TUMOUR Raised Moderately firm Erythematous and smooth Lower trunk (lumbosacral area)_
- 15. BCC - Syndromes BASAL CELL NEVUS (GORLIN’S) SYNDROME AD, no sex linkage, low penetrance ? Mutated tumour suppressor at Ch 9q23.1-q31 Childhood onset BCC (average age 20y) Pitting of palms and soles odontogenic keratocysts (epithelial jawline cysts) CNS calcifications (dura), MR
- 16. Other Associated Syndromes XERODERMA PIGMENTOSUM Incomplete sex-linked recessive Deficiency of endonuclease Childhood onset Extreme sun sensitivity BCC,SCC,Melanoma
- 17. Other Associated Syndromes ALBINISM Genetic abnormality of the pigment system.
- 18. Basal Cell Carcinoma - Histopathology Resemble normal basal cells Hyperchromatic nuclei, scant cytoplasm Clustered separate from stroma Peripheral palisading Desmoplastic reaction Nests or in continuity
- 19. Clinical course Nodulo-ulcerarive type begins as a flesh coloured waxy nodule with telangectasia ď€ -> enlarges -> central ulceration -> deepens -> roled out, beaded edges -> destroys structures locally as deep as bone/ cartilage -> aptly named rodent ulcer Rare metastasis, but recurrence known after inadequate treatment
- 20. DIFFERENTIAL DIAGNOSIS Cyst Infected spot Sebaceous hyperplasia Naevus Molluscum contagiosum Wart Bowens disease Tinea Eczema/psoriasis Malignant melanoma Seborrhoeic keratosis Erosions and leg ulcers
- 21. Treatment Options Electrodessication and curettage Curettage alone Surgical excision Mohs micrographically controlled surgery Cryosurgery Ionizing radiation Surgical excision plus radiation E xenteration
- 22. Factors Considered in Treatment Planning Pt preference to keep eye Pt age Surgical excision-considered definitive tx “ Careful frozen section controlled excision of periocular BCCs yields cure rates comparable to Mohs micrographic surgery at 5-year follow-up” 5 year recurrence of 2.2% in one study Therefore, avoiding exenteration was considered a good possibility
- 23. Ěý
- 24. Ěý
- 25. Ěý
- 26. Ěý
- 27. Ěý
- 28. Ěý
- 29. Ěý
- 30. Ěý
- 31. Ěý
- 32. Ěý
- 33. Ěý
Editor's Notes
- Italicized considered aggressive histotypes, n most likely to lead to perineural invasion n/or recurrence. Overall 5 year recurrence is 5%, 1.2% c adequate exc, 12% c tumor in 1 HPF of margin, n 33% if at margin
- NOTES FOR PRESENTERS: There are a range of different clinical presentations and histological variants of BCC. Superficial BCCs are important to distinguish clinically from other types of BCCs because they can frequently be managed medically, avoiding the need for excision. Nodular: Commonly on the face, cystic, pearly, telangiectasa, may be ulcerated, micronodular and microcystic types may infiltrate deeply. Superficial: Often multiple, usually on upper trunk and shoulders, erythematous well-demarcated scaly plaques, often larger than 20 mm at presentation, slow growth over months or years, may be confused with Bowen’s disease or inflammatory dermatoses, particularly responsive to medical rather than surgical treatment. Morphoeic: Also known as sclerosing or infiltrative BCC, usually found in mid-facial sites, skin-coloured, waxy, scar-like, prone to recurrence after treatment, may infiltrate cutaneous nerves (perineural spread). Pigmented: Brown, blue or greyish lesion, nodular or superficial histology, may resemble malignant melanoma. Basosquamous: Mixed BCC and squamous cell carcinoma (SCC), potentially more aggressive than other forms of BCC.
- These can be neglected and or treated as benign pathology.
- Like small patches of scleroderma.
- Pathology: Fibrous tumour intersected by thin anastomosing bands of basal cells. May be considered a precursor to BCC nodular type.
- The associated BCC lesions are primarily face and back BCC reported in 76% of patients with Gorlin’s
- Malignant degeneration in early adult life Death due to metastatic disease Treatment: early aggressive identification and excision of suspicious lesions.
- Abnormal synthesis and processing of melanin. Two large subtypes with numerous further subclassifications. Oculo Cutaneous Albinism : skin, hair, eyes. Ocular albinism: eyes. Increased risk for skin malignancies is similar to that of type I phototypes.
- Basophilic cells