Biologic consideration
- 1. Biologic Consideration By SHAMIN JOSHI 1
- 2. Biologic Considerations • Margin Placement and Biologic Width • Tissue Retraction • Provisional Restorations • Marginal Fit • Crown Contour • Subgingival Debris • Hypersensitivity to Dental Materials 2
- 3. Margin Placement and Biologic Width • most important aspects of understanding periodontal-restorative relationship is the location of the restorative margin to the adjacent gingival tissue. • Restorative clinicians must understand the role of biologic width in preserving healthy gingival tissues and controlling the gingival form around restorations • There are three options for margin placement: 1 ) Supragingival, 2 ) Equigingival (even with the tissue), and 3 ) Subgingival 3
- 4. Advantages of extending restoration gingivally 1) to create adequate resistance and retentive form in the preparation 2) to make significant contour alterations because of caries or other tooth deficiencies 3) to mask the tooth/restoration interface by locating it subgingivally.4
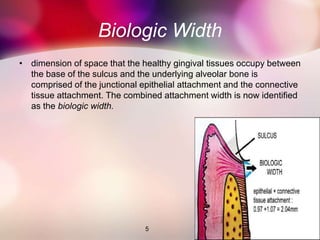
- 5. Biologic Width • dimension of space that the healthy gingival tissues occupy between the base of the sulcus and the underlying alveolar bone is comprised of the junctional epithelial attachment and the connective tissue attachment. The combined attachment width is now identified as the biologic width. 5
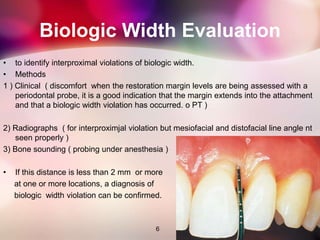
- 6. Biologic Width Evaluation • to identify interproximal violations of biologic width. • Methods 1 ) Clinical ( discomfort when the restoration margin levels are being assessed with a periodontal probe, it is a good indication that the margin extends into the attachment and that a biologic width violation has occurred. o PT ) 2) Radiographs ( for interproximjal violation but mesiofacial and distofacial line angle nt seen properly ) 3) Bone sounding ( probing under anesthesia ) • If this distance is less than 2 mm or more at one or more locations, a diagnosis of biologic width violation can be confirmed. 6
- 7. . • In 1994, Vacek et al also investigated the biologic width phenomenon they also reported a range of biologic widths as narrow as 0.75 mm in some individuals, whereas others had biologic widths as tall as 4.3 mm . • The biologic width can be identified for the individual patient by probing to the bone level and subtracting the sulcus depth from the resulting measurement. 7
- 8. Correcting Biologic Width Violations • Biologic width violations can be corrected either by ;- 1) Surgically removing bone away from proximity to the restoration margin 2) orthodontically extruding the tooth and thus moving the margin away from the bone. 8
- 9. Surgery • Surgery is the more rapid of the two treatment options (also crown lengthening ) • In these situations the bone should be moved away from the margin by the measured distance of the ideal biologic width , with an additional 0.5 mm as a safety zone. • Disadvantage 1) gingival recession after removal of bone 2) papillary recession ( interproximal removal ) 3) creation of an unesthetic triangle of space below the interproximal contacts. 9
- 10. Extrusion • . 1) low force - tooth will erupt slowly, bringing alveolar bone and gingival tissue with it until the bone level has been carried coronal to the ideal level by the amount that needs to be removed surgically to correct the attachment violation. The tooth is stabilized and then surgerically corrected . 2) Rapid orthodontic extrusion - tooth is erupted to the desired amount over several weeks. (supracrestal fiberotomy is performed circumferentially around the tooth weekly ,stabilized for at least 12 weeks to confirm the position of the tissue and bone ) 10
- 11. Margin Placement Guidelines • The first step in using sulcus depth as a guide in margin placement is to manage gingival health. Once the tissue is healthy, the following three rules can be used to place intracrevicular margins • Rule 1: If the sulcus probes 1.5 mm or less, place the restoration margin 0.5 mm below the gingival tissue crest. This is especially important on the facial aspect and will prevent a biologic width violation in a patient who is at high risk in that regard. 11
- 12. • Rule 2: If the sulcus probes more than 1.5 mm, place the margin half the depth of the sulcus below the tissue crest. This places the margin far enough below tissue, so that it will still be covered if the patient is at higher risk of recession. • Rule 3: If a sulcus greater than 2 mm is found, especially on the facial aspect of the tooth, evaluate to see if a gingivectomy could be performed to lengthen the teeth and create a 1.5-mm sulcus. Then the patient can be treated using Rule 1. 12
- 13. Clinical Procedures in Margin Placement • The placement of supragingival or equigingival margins is simple because it requires no tissue manipulation. • With regard to overall tooth preparation, the amount reduced is dictated by the choice of restorative materials. • Before extending subgingivally , the preparation should be completed to the free gingival margin facially and interproximally . • This allows the margin of the tooth preparation to be used as a reference for subgingival extension once the tissue is retracted . 13
- 14. Tissue Retraction • Once the supragingival portion of the preparation is completed, it is necessary to extend below in appropriate depth in the sulcus, • tissue must be protected from abrasion, which will cause hemorrhage and can adversely affect the stability of the tissue level around the tooth. • Access to the margin is also required for the final impression, with a clean, fluid-controlled environment. • Tissue management is achieved with gingival retraction cords Thin, fragile gingival tissues and shallow sulcus situations usually dictate that smaller diameter cords be chosen to achieve the desired tissue displacement. 14
- 15. For a Rule 1 margin (sulcus depth 1.5 mm or less), • the cord should be placed so that the top of the cord is located in the sulcus at the level in which the final margin is to be established (0.5mm) • With this initial cord in place, the preparation is extended to the top of the cord • To create space and allow access for a final impression,needs second retraction cord that it displaces the first cord apically and sits between the margin and the tissue . • For the final impression, only the top cord is removed, leaving the margins visible and accessible to be recorded with the impression material The initial cord remains in place in the sulcus until the provisional restoration is complete 15
- 16. For Rule 2 situations in which the sulcus is deeper • two larger diameter cords are used to deflect the tissue before extending the margin apically . • The top of the second cord is placed to identify the final margin location at the correct distance below the previously prepared margin, which was at the gingival tissue crest level . • The margin is lowered to the top of the second cord then a third cord is placed in preparation for the impression . • In the patient with a deep sulcus in which the margin may be 1.5 to 2.0 mm below the tissue crest, electrosurgery is often required to remove any overlying tissue in the retraction process ) 16
- 17. Provisional Restorations • Three critical areas must be effectively managed to produce a favorable biologic response to provisional restorations. 1) marginal fit, 2) crown contour 3) surface finish • Its helps to maintain the health and position of the gingival tissues during the interval until the final restorations are delivered. • Provisional restorations that are poorly adapted at the margins, that are overcontoured or undercontoured, and that have rough or porous surfaces can cause inflammation, overgrowth, or recession of gingival tissues. • As a result it compromises final restoration . 17
- 18. Marginal Fit • Marginal fit has clearly been implicated in producing an inflammatory response in the periodontium. • It has been shown that the level of gingival inflammation can increase corresponding with the level of marginal opening. • Margins that are significantly open are capable of harboring large numbers of bacteria and may be responsible for the inflammatory response • However, the quality of marginal finish and the margin location relative to the attachment are much more critical to the periodontium . 18
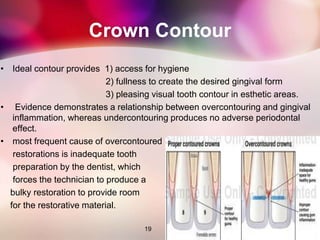
- 19. Crown Contour • Ideal contour provides 1) access for hygiene 2) fullness to create the desired gingival form 3) pleasing visual tooth contour in esthetic areas. • Evidence demonstrates a relationship between overcontouring and gingival inflammation, whereas undercontouring produces no adverse periodontal effect. • most frequent cause of overcontoured restorations is inadequate tooth preparation by the dentist, which forces the technician to produce a bulky restoration to provide room for the restorative material. 19
- 20. Subgingival Debris • Leaving debris below the tissue during restorative procedures can create an adverse periodontal response. The cause can be retraction cord, impression material, provisional material, or either temporary or permanent cement. • The diagnosis of debris as the cause of gingival inflammation can be confirmed by examining the sulcus surrounding the restoration with an explorer, removing any foreign bodies, and then monitoring the tissue response. 20
- 21. Hypersensitivity to Dental Materials • Inflammatory gingival responses have been reported related to the use of non precious alloys in dental restorations (nickel, ) • Hypersensitivity responses to precious alloys are extremely rare, and these alloys provide an easy solution to the problems encountered with the nonprecious alloys. • More importantly, tissues respond more to the differences in surface roughness of the material rather than to the composition of the material.The rougher the surface of the restoration subgingivally, the greater are the plaque accumulation and gingival inflammation. • porcelain, highly polished gold, and highly polished resin all show similar plaque accumulation. 21
- 22. 22 Thank you !
Editor's Notes
- #4: Esp in esthetic zones margin placemant iz imp
- #5: . With the advent of more translucent restorative materials, adhesive dentistry, and resin cements, the ability to place supragingival margins in esthetic areas is now a reality . Therefore, whenever possible, these restorations should be chosen not only for their esthetic advantages but also for their favorable periodontalimpact
- #7: mesiofacial and distofacial line angles , radiographs are not diagnostic because of tooth superimposition.