Blood presentation1
- 1. BLOOD TYPES; TRANSFUSION; TISSUE AND ORGAN TRANSPLANTATION BY DR. MUHAMMAD UMAIR
- 2. BLOOD TYPES ïą Multiplicity of Antigens in the Blood Cells. ïķ At least 30 commonly occurring antigens ïķ O-A-B system and the Rh system. ïą Antigenicity & Immune Reactions of Blood The bloods of different people have different antigenic and immune properties, so that antibodies in the plasma of one blood will react with antigens on the surfaces of the red cells of another blood type causing a transfusion reaction.
- 3. O-A-B BLOOD TYPES ïĒA and B AntigensâAgglutinogens ïĒ Major O-A-B Blood Types. depend on the presence or absence of A and B agglutinogens. ïĒ Genetic Determination of the Agglutinogens. ï§ Two genes, one at a time on each of two paired chromosomes ï§ Any one of three types ïType O (functionless) ïType A or ïType B
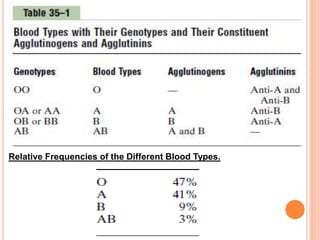
- 4. Relative Frequencies of the Different Blood Types.
- 5. AGGLUTININS (ANTIBODIES) ïĒAnti-A agglutinins ïĒ Anti-B agglutinins ï Type O blood, containing no agglutinogens, does contain both anti-A and anti-B agglutinins ï Type A blood contains type A agglutinogens and anti-B agglutinins ï Type B blood contains type B agglutinogens and anti-A agglutinins. ï Type AB blood contains both A and B agglutinogens but no agglutinins.
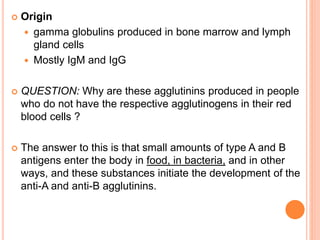
- 6. ïĒ Origin ï gamma globulins produced in bone marrow and lymph gland cells ï Mostly IgM and IgG ïĒ QUESTION: Why are these agglutinins produced in people who do not have the respective agglutinogens in their red blood cells ? ïĒ The answer to this is that small amounts of type A and B antigens enter the body in food, in bacteria, and in other ways, and these substances initiate the development of the anti-A and anti-B agglutinins.
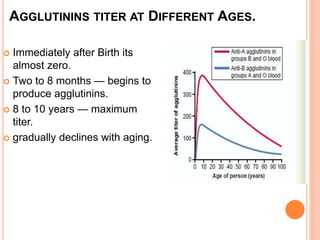
- 7. AGGLUTININS TITER AT DIFFERENT AGES. ïĒ Immediately after Birth its almost zero. ïĒ Two to 8 months â begins to produce agglutinins. ïĒ 8 to 10 years â maximum titer. ïĒ gradually declines with aging.
- 8. AGGLUTINATION PROCESS IN TRANSFUSION REACTIONS ïĒIn mismatched blood transfusion, the agglutinins of recipientâs blood are mixed with the agglutinogens of the donar RBCs. ïĒAgglutinis having binding sites attach to RBCs ïĒThis binding causes the RBCs to clump. ïĒthese clumps plug small blood vessels throughout the circulatory system
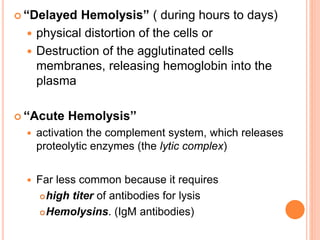
- 9. ïĒ âDelayed Hemolysisâ ( during hours to days) ï physical distortion of the cells or ï Destruction of the agglutinated cells membranes, releasing hemoglobin into the plasma ïĒ ââAcute Hemolysisââ ï activation the complement system, which releases proteolytic enzymes (the lytic complex) ï Far less common because it requires ïĒhigh titer of antibodies for lysis ïĒHemolysins. (IgM antibodies)
- 10. BLOOD TYPING ïĒ PROCEDURE ï The red blood cells are first separated from the plasma and diluted with saline. ï One portion is then mixed with anti-A agglutinin and another portion with anti-B agglutinin. ï After several minutes, the mixtures are observed under a microscope. ï An antibody antigen reaction: If the red blood cells have become clumpedââagglutinatedâ
- 11. RH BLOOD TYPES ïĒ O-A-B system VS the Rh system ïĒ massive exposure to an Rh antigen(blood transfusion) before enough agglutinins production to cause a significant transfusion reaction. ïĒ Rh Antigens ï Rh factor (six common types of Rh antigens) ï C,D, E, c, d, and e ï A person who has a C antigen does not have the c antigen and vice versa ï each person has one of each of the three pairs of antigens. ï Type D antigenâ widely prevalent and more antigenic ïĒ âRh-Positiveâ and âRh-Negativeâ People. ï +ve = having D antigen ï -ve = no D anitgen
- 12. RH IMMUNE RESPONSE ïĒ Formation of Anti-Rh Agglutinins. ï When RBCs containing Rh factor are injected into Rh-negative personâ(with no Rh factor) ï Develop slowly. ï Reach maximum conc. In about 2 to 4 months. ï With multiple exposures to the Rh factor, an Rh-negative person eventually becomes strongly âsensitizedâ to Rh factor. ïĒ Characteristics of Rh Transfusion Reactions. ï Rh +ve blood transfusion ïĒin previously unexposed Rh âve person = no immediate but delayed reaction ( after 2-4 weeks ) due to anti Rh antibodies development ïĒIn previously exposed Rh âve person = immediate and severe
- 13. ERYTHROBLASTOSIS FETALIS (âHEMOLYTIC DISEASE OF THE NEWBORNâ) ïĒ disease of the fetus and newborn child characterized by agglutination and phagocytosis of the fetusâs red blood cells. ï Mother = Rh -ve ï Father = Rh +ve ï Baby = Rh +ve ïĒ mother develops anti-Rh agglutinins from exposure to the fetusâs Rh antigen. ïĒ Which then diffuse through the placenta into the fetus and cause red blood cell agglutination. ïĒ Incidence of the Disease rises progressively with subsequent pregnancies
- 14. ïĒ Clinical Picture of Erythroblastosis. ï Anemic , jaundice, kernicterus. ï Hepatomegally and spleenomegally ï nucleated blastic red blood cells in blood picture ï Mental retardation ï Death ïĒ Treatment of the Erythroblastotic Neonate. ï Exchange Transfusion ïĒ Prevention of Erythroblastosis Fetalis. ï Rh immunoglobulinglobin, an anti-D antibody ï at 28 to 30 weeks of gestation and after delivery ï inhibit antigen-induced B lymphocyte antibody production in the expectant mother. ï anti-D antibody also attaches to D antigen sites on Rh-positive fetal RBCs hence interfere with immune response to D antigen.