bloodglucosehomeostasi taken for mbbs / nursing students
- 2. BLOOD GLUCOSE HOMEOSTASIS-OUTLINE Normal plasma glucose Factors maintaining blood glucose Post-prandial regulation Regulation during fasting Clinical aspect
- 3. BLOOD GLUCOSE HOMEOSTASIS ?Blood glucose level is tightly controlled because the brain constantly needs glucose ?Severe hypoglycemia can cause coma and death ?Chronic hyperglycemia results in ?Glycation of proteins, ?Endothelial dysfunction ?Diabetes
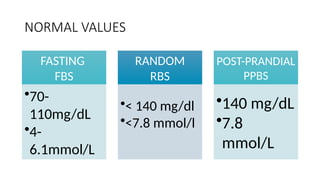
- 4. NORMAL VALUES FASTING BLOOD SUGAR[FBS] /FASTING PLASMA GLUCOSE [FPG] 70-110mg/dL 4-6.1mmol/L
- 5. REGULATION OF BLOOD GLUCOSE
- 7. FACTORS MAINTAINING BLOOD GLUCOSE Factors which cause entry of glucose into blood ? Absorption from intestines ? Glycogenolysis ? Gluconeogenesis ? Hyperglycemic hormones Factors leading to depletion of glucose in blood ? Utilization by tissues for energy ? Glycogen synthesis ? Conversion of glucose into fat ? Hypoglycemic hormone
- 8. POST-PRANDIAL REGULATION GLUCOSE ABSORPTION GLYCOGENESIS LIPOGENESIS UTILIZATION BY TISSUE FOR ENERGY GLYCOLYSIS TCA CYCLE ETC
- 9. REGULATION DURING FASTING GLUCOSE GLYCOGENOLYSIS LIPOLYSIS GLYCEROL, LACTATE, PYRUVATE, GLUCOGENIC AMINO ACIDS GLUCONEOGENESIS FFA ALTERNATE SOURCE OF ENERGY
- 10. HORMONAL REGULATION HYPERGLYCEMIC HORMONES ? Glucagon ? Cortisol ? Epinephrine ? Growth hormone HYPOGLYCEMIC HORMONES ? Insulin
- 11. HORMONAL REGULATION The pancreas detects the change in blood glucose concentration and releases the appropriate hormone High blood glucose Signal to release Hypoglycemic hormone insulin Low blood glucose Signal to release Hyperglycemic hormone glucagon
- 12. HYPERGLYCEMIC HORMONES GLUCAGON Promotes Glycogenolysis, gluconeogenesis Depresses glycogen synthesis EPINEPHRINE Promotes Glycogenolysis, gluconeogenesis Favours uptake of amino acids CORTISOL Increases gluconeogenesis Releases amino acids from the muscle GROWTH HORMONE Decreases glycolysis Mobilizes fatty acids from adipose tissue
- 14. HORMONAL REGULATION- INSULIN INSULIN GLYCOGENESIS GLYCOLYSIS GLUCONEOGENESIS GLUCOSE UPTAKE IN MUSCLE AND ADIPOSE TISSUE GLYCOGENOLYSIS LIPOLYSIS LIPOGENESIS + + + + - - -
- 15. FED STATE
- 16. HORMONAL REGULATION- INSULIN ? Glucose is diffused into cells through transporters such as GLUT4 ? GLUT4 is present in cytoplasmic vesicles ? Insulin binding to its receptor causes vesicles to diffuse into plasma membrane ? Brain and liver have non-insulin dependent glucose transporter
- 17. FASTING STATE
- 18. HORMONAL REGULATION INSULIN favours glycolysis by activating the key enzymes of glycolysis GLUCAGON inhibits key enzymes of glycolysis ?Glucokinase ?Phosphofructokinase ?Pyruvate kinase
- 19. Insulin & glucagon has opposing action
- 20. RENAL REGULATION Tubular maximum Renal threshold Glycosuria Glucosuria Occurs When the Renal Threshold for Glucose Is Exceeded Glucosuria occurs when the venous blood glucose concentration exceeds 180mg/dL [9.5©C10.0 mmol/L]
- 21. BLOOD GLUCOSE ©C CLINICAL ASPECT Estimation Common terms Value interpretaio n
- 22. BLOOD GLUCOSE ESTIMATION ? The blood is collected using an anticoagulant (potassium oxalate) and an inhibitor of glycolysis (sodium fluoride). ? Fluoride inhibits the enzyme, enolase, and so glycolysis on the whole is inhibited ? The glucose oxidase (GOD) method is the one most widely used.
- 23. NORMAL VALUES- common terms ? A FBS is taken after at least eight hours of fasting FASTING PLASMA GLUCOSE [FPG/FBS] ? Test done any time of day without regard to time since last meal. RANDOM PLASMA GLUCOSE [RBS/RPG] ? The test done about 2 hr after a good meal POST-PRANDIAL BLOOD GLUCOS [PPBS]
- 24. NORMAL VALUES FASTING FBS ?70- 110mg/dL ?4- 6.1mmol/L RANDOM RBS ?< 140 mg/dl ?<7.8 mmol/l POST-PRANDIAL PPBS ?140 mg/dL ?7.8 mmol/L
- 25. 27/12/2024 26 o v e r n i g h t f a s t n e s a m p l e i s c o l l e c s g l u c o s e i n a b o u t p e c i m e n s a r e c o l l e c t Blood tests GLUCOSE TOLERANCE TEST
- 26. 27/12/2024 27 The Diabetes Expert Committee criteria for evaluating the standard oral glucose tolerance test. Normal Glucose Tolerance Impaired Glucose Tolerance Diabetes Mellitus Fasting plasma glucose (mg/dL) < 110 <6.1mmol/L 110©C125 Ī▌126 >7mmol/L Two hours after glucose load (mg/dL) < 140 <7.8mmol/L Ī▌140©C199 Ī▌200 >11.1mmol/L Blood tests GLUCOSE TOLERANCE TEST
- 27. 27/12/2024 28
Editor's Notes
- #26: Recommendation 6 The oral glucose tolerance test (OGTT) should be retained as a diagnostic test for the following reasons fasting plasma glucose alone fails to diagnose approximately 30% of cases of previously undiagnosed diabetes an OGTT is the only means of identifying people with IGT an OGTT is frequently needed to confirm or exclude an abnormality of glucose tolerance in asymptomatic people An OGTT should be used in individuals with fasting plasma glucose 6.1©C6.9mmol/l (110©C125mg/dl) to determine glucose tolerance status. Recommendation 7 Currently HbA1c is not considered a suitable diagnostic test for diabetes or intermediate hyperglycaemia.
- #27: Federation of Clinical Chemistry (IFCC) recommendation that all glucose measuring devices report in plasma values57. Measurement differences may also arise depending on the site of collection of the blood sample. Venous and capillary samples will give the same result in the fasting state but in the non-fasting state capillary will give higher results than venous samples. The processing of the sample after collection is important to ensure accurate measurement of plasma glucose. This requires rapid separation of the plasma after collection (within minutes) but it is recognised that this seldom occurs. Collection into a container with glycolytic inhibitors (eg NaF) is only partially effective. A minimum requirement is that the sample should be placed immediately in ice-water after collection and before separating but even so separation should be within 30min58. Recommendation 5 1. Venous plasma glucose should be the standard method for measuring and reporting. However in recognition of the widespread use of capillary sampling, especially in under-resourced countries, conversion values for capillary plasma glucose are provided for post- load glucose values. Fasting values for venous and capillary plasma glucose are identical. 2. Glucose should be measured immediately after collection by near patient testing, or if a blood sample is collected, plasma should be immediately separated, or the sample should be collected into a container with glycolytic inhibitors and placed on ice-water until separated prior to analysis.
- #28: National Glycohemoglobin Standardization Program (NGSP) and standardized or traceable to the Diabetes Control and Complications Trial (DCCT)



![NORMAL VALUES
FASTING BLOOD SUGAR[FBS] /FASTING PLASMA GLUCOSE [FPG]
70-110mg/dL 4-6.1mmol/L](https://image.slidesharecdn.com/bloodglucosehomeostasitaken-241227153553-ca978794/85/bloodglucosehomeostasi-taken-for-mbbs-nursing-students-4-320.jpg)















![RENAL REGULATION
Tubular
maximum
Renal
threshold
Glycosuria
Glucosuria Occurs When the Renal Threshold for Glucose Is
Exceeded
Glucosuria occurs when the venous blood glucose concentration
exceeds 180mg/dL [9.5©C10.0 mmol/L]](https://image.slidesharecdn.com/bloodglucosehomeostasitaken-241227153553-ca978794/85/bloodglucosehomeostasi-taken-for-mbbs-nursing-students-20-320.jpg)


![NORMAL VALUES- common terms
? A FBS is taken after at least eight
hours of fasting
FASTING PLASMA
GLUCOSE [FPG/FBS]
? Test done any time of day without
regard to time since last meal.
RANDOM PLASMA
GLUCOSE [RBS/RPG]
? The test done about 2 hr after a good
meal
POST-PRANDIAL
BLOOD GLUCOS
[PPBS]](https://image.slidesharecdn.com/bloodglucosehomeostasitaken-241227153553-ca978794/85/bloodglucosehomeostasi-taken-for-mbbs-nursing-students-23-320.jpg)