Bundle care
- 3. INTRODUCTION  The care bundle is a new concept in critical care ,which is currently being promoted by the national Health service modernization agency for critical care .  Care bundle originated in north American and are described best as groups of evidence –based practice intervention .  The theory behind care bundle is that when several evidence based interventions are grouped together in a single protocol, it will improve patient outcome.
- 4. HISTORY
- 5. DEFINITION OF BUNDLE CARE A small set of evidenced – based practice protocol which is a grouping of elements for a particular symptom of a wider range of conditions in the future. A small set of evidenced – based interventions for a defined patient segment or population care setting that, when implemented together , will result in significantly better outcomes than when implemented individually.
- 6. BUNDLE DESIGN ÔÇß The bundle has three to five interventions (elements), with strong clinician agreement. ÔÇß Each bundle element is relatively independent. ÔÇß The bundle is used with a defined patient population in one location. ÔÇß The multidisciplinary care team develops the bundle. ÔÇß Bundle elements should be descriptive rather than prescriptive, to allow for local customization and appropriate clinical judgment. ÔÇß Compliance with bundles is measured using all-or-none measurement, with a goal of 95 percent or greater.
- 7. ELEMENTS OF BUNDLE CARE ÔÇßAll the elements of the bundle are necessary and removing any one of them will result in inferior result. ÔÇßAll the elements in the bundle are based on randomized controlled trial and the recommendations are beyond any controversy. ÔÇßA bundle focuses on how to deliver this evidence of care rather than what the right care should be. ÔÇßAll elements in the bundle involve an all or none phenomenon and the Bundle itself also bears the same characteristic.
- 8. That is to say each element in the bundle is either “performed” or “not performed” and entire Bundle performance also follows the same principle without leaving any scope for partial performance. Implementation of all Bundle elements should take place simultaneously at a specific time and place with a minimum delay.
- 9. TYPES OF BUNDLE 1.Ventilator bundle 2.Central line bundle ÔÉòCentral line associated blood stream infections (CLABSI) 3. Catheter associated urinary tract infections (CAUTI)
- 11. 1.VENTILATOR BUNDLE Elevation of the head of the bed (up to 30-45 degrees)  Patients on ventilator have a risk of getting pneumonia.  One of the ways to prevent patient from getting pneumonia is the elevation of head at the proper angle.  Head end elevation to 45 degree has been recommended in most ventilator care bundles when feasible.
- 12. Daily sedation vacation and assessment of readiness to extubate.  Sedation vacation is a colloquial term for an interruption of the infusion of sedatives in a mechanically ventilated patients, decreasing the depth of sedation in a critically ill patient to facilitate weaning from mechanical ventilation .  Sedation vacation was first introduced in 2000 by J.P. KRESS.  Measures like daily sedation vacation facilitates early weaning and extubation.
- 13. Stress ulcer disease prophylaxis  Stress ulcer is seen in patients who are seriously ill, including those with respiratory failure requiring mechanical ventilation, increased stress cause sympathetic nervous system activation , increased catecholamine release, vasoconstriction and secretion of cytokine.  When this condition persist they cause injury or ulceration.  Proton pump inhibitor and H2 receptor antagonist both prevent GI bleeding by raising the gastric pH.
- 14. Deep vein thrombosis prophylaxis  Whenever blood moves too slowly through veins it can cause clump of blood cells called clot, which causes deep vein thrombosis.  People in ventilator are high risk for deep vein thrombosis.  Low molecular weight heparin or unfractionated heparin products are effective in preventing deep vein thrombosis.
- 15. Oral decontamination with chlorhexidine  Chlorhexidine is a disinfectant and antiseptic that is used for skin disinfection, cleansing wounds and preventing dental plaques.  Nosocomial pneumonia is common in ICU patients oral cleansing with chlorhexidine has been shown to decrease incidence of pneumonia in patients.
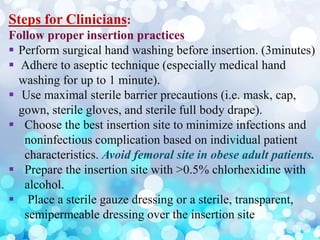
- 18. Steps for Clinicians: Follow proper insertion practices ÔÇß Perform surgical hand washing before insertion. (3minutes) ÔÇß Adhere to aseptic technique (especially medical hand washing for up to 1 minute). ÔÇß Use maximal sterile barrier precautions (i.e. mask, cap, gown, sterile gloves, and sterile full body drape). ÔÇß Choose the best insertion site to minimize infections and noninfectious complication based on individual patient characteristics. Avoid femoral site in obese adult patients. ÔÇß Prepare the insertion site with >0.5% chlorhexidine with alcohol. ÔÇß Place a sterile gauze dressing or a sterile, transparent, semipermeable dressing over the insertion site
- 19. ÔÇß For patients of age18 or more, use a chlorhexidine impregnated dressing with an FDA cleared label that specifies a clinical indication for reducing CLABSI for short term non-tunneled catheters. Handle and maintain central lines appropriately ÔÇß Comply with hand hygiene requirements. ÔÇß Bathe ICU patients over 2 months of age with a chlorhexidine preparation on a daily basis.
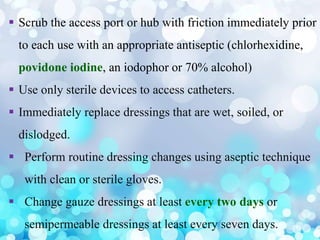
- 20. ÔÇß Scrub the access port or hub with friction immediately prior to each use with an appropriate antiseptic (chlorhexidine, povidone iodine, an iodophor or 70% alcohol) ÔÇß Use only sterile devices to access catheters. ÔÇß Immediately replace dressings that are wet, soiled, or dislodged. ÔÇß Perform routine dressing changes using aseptic technique with clean or sterile gloves. ÔÇß Change gauze dressings at least every two days or semipermeable dressings at least every seven days.
- 21. ÔÇß Change administrations sets for continuous infusions not more frequently than every 4 days, but at least every 7 days. ÔÉòIf blood or blood products or fat emulsions are administered change the tubing every 24 hours. ÔÉòIf propofol is administered, change tubing every 6-12 hours or when the vial is changed. For Healthcare Organizations: ÔÇß Educate healthcare personnel about indications for central lines, proper procedures for insertion and maintenance, and appropriate infection prevention measures.
- 22. ÔÇß Designate personnel who demonstrate competency for the insertion and maintenance of central lines. ÔÇß Periodically assess knowledge of and adherence to guidelines for all personnel involved in the insertion and maintenance of central lines. ÔÇß Provide a checklist to clinicians to ensure adherence to aseptic insertion practices. ÔÇß Reeducate personnel at regular intervals about central line insertion, handling and maintenance, and whenever related policies, procedures, supplies, or equipment changes.
- 23. ÔÇß Empower staff to stop non-emergent insertion if proper procedures are not followed. ÔÇß Ensure efficient access to supplies for central line insertion and maintenance (i.e. create a bundle with all needed supplies) ÔÇß Use hospital-specific or collaborative-based performance measures to ensure compliance with recommended practices.
- 24. CATHETER ASSOCIATED URINARY TRACT INFECTION
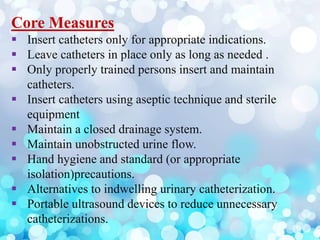
- 25. Core Measures ÔÇß Insert catheters only for appropriate indications. ÔÇß Leave catheters in place only as long as needed . ÔÇß Only properly trained persons insert and maintain catheters. ÔÇß Insert catheters using aseptic technique and sterile equipment ÔÇß Maintain a closed drainage system. ÔÇß Maintain unobstructed urine flow. ÔÇß Hand hygiene and standard (or appropriate isolation)precautions. ÔÇß Alternatives to indwelling urinary catheterization. ÔÇß Portable ultrasound devices to reduce unnecessary catheterizations.