Burn
- 2. ÔÇßBurn is defined as a wound caused by an exogenous agent leading to coagulated necrosis of the tissue.
- 3. ÔÇßTHERMAL BURNS ÔÇßCHEMICAL BURNS ÔÇßELECTRICAL BURNS ÔÇßCOLD BURNS ÔÇßRADIATIONS
- 4. THERM AL BURNS Scald burn  Most frequent in home injuries like hot water , liquids and food are most common cause. Temperature above than 136˚F causes burn. Temperature less than 111˚F tolerated for long periods
- 5. CHEMIC AL BURN  Common in industries and factories but can occur at homes also. Caused by concentrated acids or alkalis. Acids are more common than alkali.
- 6. ELECTRIC AL BURNWorse than other types of burn with entry and exit wounds. May stop the heart and depress the respiratory system. May cause thrombosis and cataracts.
- 7. RADIATI ON BURNSCause due to radiations Radioactive explosions. X-Rays. Nuclear bomb explosions.
- 8. P’PHYSIOLO GY OF BURNS FLUID SHIFT Period of inflammatory response. Vessels adjacent to burn injury dilates – inc. hydrostatic pressure and inc. capillary permeability. Continuous leak of plasma from intravascular space to interstitial space. Associated imbalances of fluids, electrolytes and acid-base occur. Hemoconcentration Lasts 24-36 hours.
- 9. P’PHYSIOLO GY OF BURNS FLUID REMOBILIZATION Capillary leak ceases and fluid shifts back into the circulation. Restores renal perfusion and fluid balance. Increase urine formation and diuresis. Continued electrolyte imbalances. Hyponatremia Hypokalemia hemodilution
- 10. BODY’S RESPON SE TO BURN. Emergent phase (STAGE 1) Pain response Catecholamine response Tachycardia ,tachypnea , mild hypertension , mild anxiety
- 11. BODY’S RESPON SE TO BURN. FLUID SHIFT PHASE (STAGE 2) Length 18-24 hours. Begins after emergent phase Reaches peak level in 6-8 hours. Damaged cells initiate inflammatory response. Increased blood flow to cells Shift of fluid from intravascularto extravascular space
- 12. BODY’S RESPON SE TO BURN. HYPERMETABOLIC PHASE ( STAGE 3) Last for days to weeks Large increase in body’s need for nutrients as it repairs itself RESOLUTION PHASE (STAGE 4) Scar formation General rehabilitation and progression to normal function.
- 13. CLASSIFICA TION OF BURNSÔÇßFIRST DEGREE ÔÇßSUPERFICIAL SECOND DEGREE ÔÇßDEEP SECOND DEGREE ÔÇßTHIRD DEGREE ÔÇßFOURTH DEGREE
- 14. 1ST DEGREE BURN ÔÇßReddened skin ÔÇßPain at burn site ÔÇßInvolves only epidermis ÔÇßBlanch to touch ÔÇßHave an intact epidermal barrier ÔÇßDo not result in scaring ÔÇßEG: sunburn , minor accident ÔÇßTreatment with topical soothing agents or NSAIDS
- 15. 2ND DEGREE BURNS ÔÇßIntense skin ÔÇßWhite to red skin ÔÇßBlisters ÔÇßInvolves dermis and papillary layers of dermis ÔÇßSpares hair follicles , sweat glands etc. ÔÇßErythematous and blanch to touch. ÔÇßVery painful/sensitive. ÔÇßNo or minimal scarring ÔÇßSpontaneously re-epithelize from retained epidermal structures in 7-14 days.
- 16. SECOND DEGREE BURN ÔÇßInjury to deeper layers of dermis-reticular dermis ÔÇßAppear pale and mottled ÔÇßDo not blanch to touch ÔÇßCapillary return sluggish or absent. ÔÇßTake 13 to 45 days to heal ÔÇßRequires excision or skin grafting.
- 17. 3RD DEGREE BURN ÔÇßDry, leathery skin (white , dark , brown or charred) ÔÇßLoss of sensation (little pain) ÔÇßAll dermal layers/tissues may be involved. ÔÇßAlways require surgery.
- 18. 4TH DEGREE BURN ÔÇßInvolves structure beneath the skin- muscle , bone
- 19. ASSESEM ENT OF BURNS RULE OF NINES Best used for large surface areas Expedient tool to measure extent of burn • RULE OF PALMS Best used for burns <10 % BSA
- 20. MANAGEM ENTÔÇßPRE HOSPITAL CARE ÔÇßEnsure rescuer safety ÔÇßStop the burning process : stop , drop and fall. ÔÇßCheck for other injuries ÔÇßA standard ABC (AIRWAY , BREATHING , CIRCULATION) check followed by a rapid secondary survey.
- 21. MANAGEM ENT ÔÇßCool the burnt wound ÔÇßGive oxygen ÔÇßElevate ÔÇßGive analgesic
- 22. HOSPIT AL CARE A : Airway control B : Breathing and ventilation C : Circulation D : Disability – neurological status E : exposure with environmental control F : fluid resuscitation
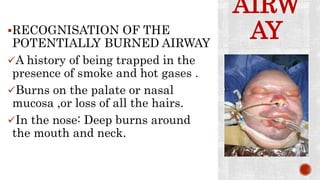
- 23. AIRW AYRECOGNISATION OF THE POTENTIALLY BURNED AIRWAY A history of being trapped in the presence of smoke and hot gases . Burns on the palate or nasal mucosa ,or loss of all the hairs. In the nose: Deep burns around the mouth and neck.
- 24. AIRW AYBurned airway Early elective intubation is safest. Delay can make intubation very difficult because of swelling. Be ready to perform an emergency cricothyroidotomy if intubation is delayed.
- 25. BREATHI NGInhalation injury Thermal burn injury to the lower airway. Metabolic pathway:carboxy hemoglobin Mechanical block to breathing: escharotomy
- 26. CIRCULATI ONMaintain iv line with wide bore cannula peripherally. One central line. Escharotomy of limbs if circulatory compromise in circumferential burns.
- 27. FLUIDS FOR RESUSCITAT ION In children with burns over 10% TBSA and adults with burns over 15%TBSA , consider the needs for iv fluid resuscitation. If oral fluids are to be used , salt must be added. Fluids needed can be calculated from a standard formula. The key is to monitor unit output.
- 28. FLUIDS FOR RESUSCITAT ION PARKLAND FORMULA % TBSA ×Weight (KG)×4 = Volume (ml) Half this volume is given in first eight hours. Second half is given in the subsequent 16 hours. Crystalloid : ringer lactate Hypertonic saline Human albumin solution Colloid resuscitation
- 29. NUTRITI ONÔÇßBurnt patient need extra feeding ÔÇßA nasogastric tube should be used in all patients with burn over 15% of TBSA ÔÇßRemoving the burn and achieving healing stops the catabolic drive.
- 30. NUTRITI ONSUTHERAND FORMULA Children : 60 kcal/kg +35 %kcal TBSA Adults : 20 kcal/kg +70 %kcal TBSA •PROTEIN 20% of energy 1.5 to 2 g/kg protein/day
- 31. MONITORING AND CONTROL OF INFECTION ÔÇßBurn patients are immunocompromised. ÔÇßThey are susceptible to infections through many routes. ÔÇßSterile precautions should be taken. ÔÇßSwabs should be used regularly. ÔÇßA rise in WBC count ,thrombocytosis, and increase catabolism are warnings of infections.
- 32. TOPICAL TREATMEN T OF DEEP BURNS ÔÇß1% silver sulphadiazine cream. ÔÇß0.5% silver nitrate solution. ÔÇßMafenide acetate cream. ÔÇßSerum nitrate, silver sulphadiazine and cerium nitrate.
- 33. PRINCIPLES OF DRESSINGS FOR BURNS Full – thickness and deep dermal burns need antibacterial dressings to delay colonization prior to surgery. Superficial burns will heal and require simple dressings. An optimal healing environment can make a difference to outcome in borderline depth burns.