Burns In The Pediatric Population
- 1. Burns In The Pediatric Population Dr. E. M. Regis Jr. MD. House Officer Dept. of General Surgery
- 2. Overview ŌĆó Definition ŌĆó Incidence/ Etiology ŌĆó Risk/ Contributing Factors ŌĆó Child Abuse ŌĆó Pathophysiology ŌĆó Classification ŌĆó Criteria for admission ŌĆó Management ŌĆó Complications
- 3. Definition ŌĆó A burn is a type of injury to the flesh or skin caused by heat, electricity, chemical, friction or radiation
- 4. Incidence ŌĆó One of the leading causes of accidental injuries at home. ŌĆó 5th most common cause of accidental death in children ŌĆó Hot tap water burns cause more deaths and hospitalizations than burns from any other hot liquids.
- 5. Etiology ŌĆó Flame 57% ŌĆó Scalding 32% ŌĆó Chemical 7% ŌĆó Electricity & Radiation 4%
- 7. Contributing Factors ŌĆó Socio-economics - children from low income homes have 8x a risk of sustaining burns than those from higher income homes - severity of burns inversely proportional to decreasing SES - burn mortality is higher among children from lower SES
- 8. ŌĆó Living Conditions - children are naturally curious, impulsive and active,ŌĆ”increases risk of burns - flammable and caustic substances stored in the home - heating with indoor fires - cooking practices; NB. 2 billion people worldwide cook with open flames or unsafe traditional stoves
- 9. - lack of adult supervision - overcrowding ŌĆóMedical conditions -Epilepsy * Increase risk of fall * Traditional medicine practices; eg. The deliberate burning of feet to ŌĆ£rouse the child from convulsive stateŌĆØ.
- 10. Child Abuse ŌĆó Burns account for 10% of all cases of child abuse ŌĆó Majority of victims are < 2 years of age ŌĆó Scalding is the most common cause
- 11. Suspicion of child abuse Burns to: ŌĆō Perineum ŌĆō Ankles ŌĆō Wrists ŌĆō Palms ŌĆō Soles ŌĆóBurns with clean line of demarcation ŌĆóPresence of older injuries ŌĆóContradictory accounts of ŌĆ£accidentŌĆØ ŌĆóDelays in seeking treatment
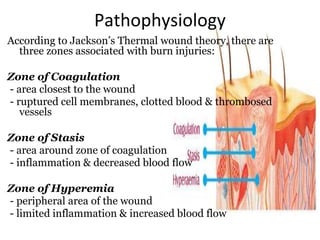
- 12. Pathophysiology According to JacksonŌĆÖs Thermal wound theory, there are three zones associated with burn injuries: Zone of Coagulation - area closest to the wound - ruptured cell membranes, clotted blood & thrombosed vessels Zone of Stasis - area around zone of coagulation - inflammation & decreased blood flow Zone of Hyperemia - peripheral area of the wound - limited inflammation & increased blood flow
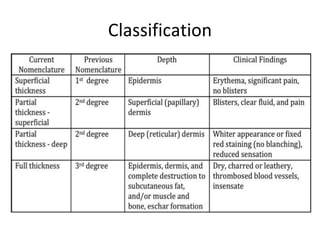
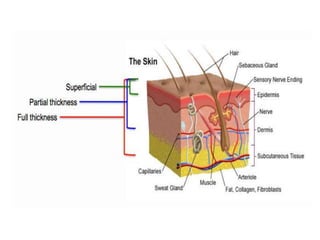
- 13. Classification
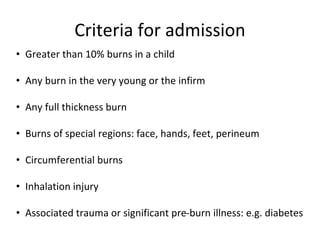
- 15. Criteria for admission ŌĆó Greater than 10% burns in a child ŌĆó Any burn in the very young or the infirm ŌĆó Any full thickness burn ŌĆó Burns of special regions: face, hands, feet, perineum ŌĆó Circumferential burns ŌĆó Inhalation injury ŌĆó Associated trauma or significant pre-burn illness: e.g. diabetes
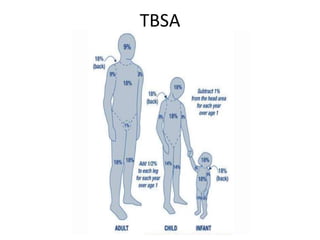
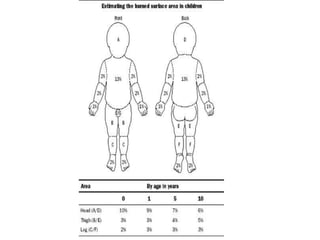
- 16. TBSA
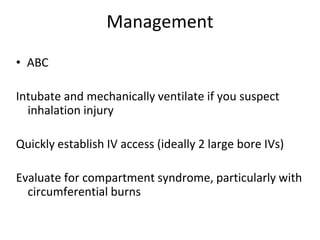
- 18. Management ŌĆó ABC Intubate and mechanically ventilate if you suspect inhalation injury Quickly establish IV access (ideally 2 large bore IVs) Evaluate for compartment syndrome, particularly with circumferential burns
- 19. Assessing inhalation injury ŌĆó Look for: ŌĆō ŌĆō Singed facial hairs ŌĆō ŌĆō Edema of nose, mouth, pharynx and larynx ŌĆō ŌĆō Carbonaceous sputum ŌĆō ŌĆō Hoarseness ŌĆō ŌĆō Stridor
- 20. Fluid Resuscitation ŌĆō ŌĆō Restoring adequate intravascular volume to prevent hypotension and shock ŌĆō ŌĆō Correcting electrolyte abnormalities ŌĆō ŌĆō Minimize renal insufficiency ŌĆó If burns >15% ŌĆō ŌĆō Massive fluid shifts will likely occur due to systemic inflammatory response syndrome (SIRS) ŌĆō ŌĆō Fluid needs will be greater than anticipated based on appearance of burn alone
- 21. ŌĆó Parkland formula: ŌĆō 3-4 ml x kg x % total burn surface area (TBSA) 1Ōüä2 in first 8 hours Remaining in next 16 hours ŌĆó Galveston ShrinerŌĆÖs formula ŌĆō 5000 mL/m2 TBSA burn + 2000 mL/m2 body surface area (BSA)
- 22. ŌĆó Fluid: Lactate Ringer ŌĆō plus 12.5 g 25% albumin per L ŌĆō plus D5W as needed for hypoglycemia Remember to monitor glucose levels ŌĆó Glycogen stores of children <5 y/o run out quickly ŌĆó Inhalation injury increases fluid requirements by 1.1 ml/kg/% TBSA ŌĆó Goal of fluid resuscitation = Adequate urine output (1-1.5ml/kg/hr)
- 23. Muir & Barclay Formula ŌĆó TBSA % x weight (kg) = volume (mls) fluid need per period. ŌĆóThe volume needs to be recalculated at each change in time period: ŌĆó Every four hours for the first 12 hours; ŌĆó Every six hours between 12 and 24 hours; ŌĆó After 36 hours.
- 24. Dressings Topical antibiotic: ŌĆō Silver nitrate ŌĆó Cheap ŌĆó Does not penetrate eschar ŌĆó Depletes electrolytes ŌĆō Silver sulfadiazine ŌĆó Some penetration of eschar ŌĆó Risk of neutropenia ŌĆō Mafenide acetate ŌĆó Penetrates eschar ŌĆó Risk of developing acidosis
- 25. Nutrition ŌĆó Burns lead to increased metabolic demands and energy requirements ŌĆō For burns >40%, resting metabolic rate increases up to 200% ŌĆō Primarily protein catabolism * Protein requirement increased to 2.0 g/kg/day ŌĆó Without adequate nutrition wound healing will not occur
- 26. ŌĆó Goal: Loss of less than 10% of preinjury weight ŌĆō Patients should be weighed daily ŌĆó Enteral feeds are superior to parenteral ŌĆō Feed child orally if possible ŌĆō Otherwise place nasogastric feeding tube
- 27. Management contŌĆÖd. ŌĆó PPIsŌĆ”. Prophylaxis against stress ulcers ŌĆó Adequate analgesics ŌĆó Prophylaxis antibiotics ŌĆó Physiotherapy/ pressure garments
- 28. Complications ŌĆó Disfigurement ŌĆó Contractures ŌĆō Lead to severe disability in many cases ŌĆó Emotional damage/sequelae ŌĆó Delay in reaching developmental milestones and educational development ŌĆó Death
- 29. Summary ŌĆó Burns account for a significant proportion of pediatric morbidity and mortality worldwide, particularly in LSES. ŌĆó Majority of burns are due to fire or scalding, often related to cooking practices. ŌĆó Initial evaluation should always include an assessment for child abuse. ŌĆó Ultimately, the key to decreasing morbidity and mortality associated with burns is prevention via... ŌĆō Educational campaigns ŌĆō Legislative changes ŌĆō Hazard reduction and environmental modification
- 30. References ’āÅStone, Keith and Humphries, Roger; Current Diagnosis and Treatment: Emergency Medicine. McGraw- Hill New York 2008 ’āÅStead, Latha G. etal ; First Aid for the Emergency medicine Clerkship; McGraw Hill 2002 ’āÅwww.emedicine.com ’āÅwww.google.com/images ’āÅGlobal Health Education Consortium
Editor's Notes
- #20: Can occur without skin burns Carbonaceous sputum ŌĆō burned saliva
- #21: Fluid is key for:
- #22: Plus maintenance fluid
- #24: this uses a colloid resuscitation with plasma and runs over 36 hours. As the fluid lost from the circulation is plasma, it seems logical to replace it with plasma. With colloid resuscitation, less volume is required and the blood pressure is better supported. However, both colloid and plasma are expensive. They may also leak out of the circulation and may result in oedema of the lungs. The 36 hours are divided into six periods of varying length, and an equal volume of plasma is administered in each period. The volume to be transfused in each period is calculated via the formula. This volume is given in each successive period of four, four, four, six, six and 12 hours. At the end of a period, if the assessment shows that the patientŌĆÖs clinical condition is stable, the transfusion is continued according to the formula. If there is any clinical evidence of under- or overtransfusion then the plasma rations for the next and following periods are altered accordingly.
- #25: Silver sulph ( broad spec prophylaxis against pseudomonas and methicillin resistant stap aureus) Silver nitrate ( not active against some gram ŌĆōve aerobes and need to be reapplied ever 2-4hrs) Mafenide cream ( painful to apply, associated with metabolic acidosis)
- #29: +/- social worker and counselling