Ca penis
- 1. Carcinoma penis Joydeep Ghosh SR, medical oncology
- 2. Risk factors.. Risk factor Relevance •Phimosis OR 11-16 •chronic penile inflammation (balanoposthitis related to phimosis) •balanitis xerotica obliterans (lichen sclerosus) Increased risk •sporalene and UV-A phototherapy for various dermatologic conditions such as psoriasis Incidence increases 9 folds with > 250 treatments •Smoking 5 fold increase •HPV infection, esp types 16 and 18 Present in 22 – 68% cases •Rural area, low SE status, unmarried •Multiple sexual partners, early age if intercourse 3-5 fold increased risk
- 6. • N: 193 • Included the following: – Histological grade – Depth of infiltration – PNI • Score: – 0: no mets, 7: 80% mets • May be used as a guide to inguinal node dissection
- 7. Recommendations for staging Primary tumor Physical examination, recording morphology, extent and invasion of penile structures. MRI with artificial erection in selected cases with intended organ preserving surgery. Inguinal nodes: Physical examination of both groins, recording number, laterality and characteristics of inguinal nodes • If nodes are not palpable, invasive lymph node staging in high-risk patients. • If nodes are palpable, a pelvic CT may be indicated, PET/CT is an option. Distant mets In N+ patients, abdomino-pelvic CT scan and chest X-ray are required for systemic staging. PET/CT scan is an option. Bone scan if clinically indicated
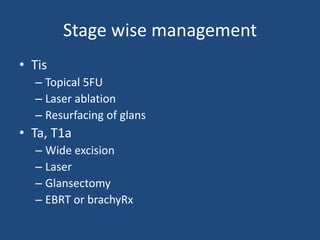
- 8. Stage wise management • Tis – Topical 5FU – Laser ablation – Resurfacing of glans • Ta, T1a – Wide excision – Laser – Glansectomy – EBRT or brachyRx
- 9. • T2 with corpora cavernosa invasion – Partial amputation – RT for lesions <4cm • T3 with urethral involvement – Partial or total penectomy with perineal urethrostomy • T4 lesion: – NACT followed by surgery in responders – Pall EBRT
- 10. Management of regional nodes • Defn of regional nodes:
- 11. • cN0 nodes: – Surveillance: only for very early lesions, pTa, pTis – Invasive nodal lesions: • Modified ILND • SLNB : Tc99 colloid or patent blue, sensi: 88-90% – If LN are found to be positive: ipsilateral ILND is indicated
- 12. Palpable inguinal nodes: cN1, cN2 • Antibiotics and reassessment: NOT RECOMMENDED • no additional investigation is required if palpable clinically • However, CT/ MRI/ PET may be used to rule out pelvis LN • Options: – Ipsilateral ILND – Pelvis LND • If two or more positive lymph nodes or • Ornellas AA,. J Surg Oncol 2008 May • one node with extracapsular extension (pN3) • Lughezzani G,. J Urol 2013 Nov
- 13. Fixed nodes… • Metastatic workup is necessary • Surgery is not generally recommended • Multimodal treatment is recommended – NACT followed by surgery in responders – Long term survival of 30% • Pizzocaro G, Piva L. Adjuvant and neoadjuvant vincristine, bleomycin, and methotrexate for inguinal metastases from squamous cell carcinoma of the penis. Acta Oncol 1988;27(6b):823-4
- 14. Nodal recurrence • If after surveillance: same principles apply as before • If after LND – Mets w/u – NACT or ACT after re surgery if feasible
- 15. Role of RT • Not much published data • Does not improve survival either in neoadjuvant or adjuvant settings • Prospective trial comparing RT vs surgery: surgery better – Kulkarni JN, Kamat MR. et al Eur Urol 1994 • Adjuvant chemo is better than adjuvant RT: retrospective data – Lucky MA, Rogers B, Parr NJ. Referrals into a dedicated British penile cancer centre and sources of possible delay. Sex Transm Infect 2009
- 16. Role of chemotherapy • Adjuvant: – Italian group: 1979-1990 – 25 pts treated with weekly VMB (VCR, bleomycin, mtx): for 12 couses – Compared to retrospective cohort of 35pts – Median f/u 42 months – Long term DFS: 84% vs 39%
- 17. • N: 19 pts • Median f/u: 15.3 months • Median DFS was 16.2 months • Median OS was not reached
- 18. • No data available on adjuvant in pN1 disease
- 19. NACT for fixed or relapsed nodes • Small retrospective studies of 5-20 patients have reported bleomycin-vincristine- methotrexate (BVM) and bleomycin- methotrexate-cisplatin (BMP) • Hakenberg OW, Nippgen JB, Froehner M, et al. Cisplatin, methotrexate and bleomycin for treating advanced penile carcinoma. BJU Int 2006 • Leijte JA, Kerst JM, Bais E, et al. Neoadjuvant chemotherapy in advanced penile carcinoma. Eur Urol 2007
- 20. • N : 28 • irinotecan (60 mg/m2) on days 1, 8 and 15 and cisplatin (80mg/m2) administered every 28 days • T3/4, N1-3, M1 were included • Failed to demonstrate a response rate of more than 30%
- 21. • N: 30 • N2/3 disease, non metastatic • ORR: 50% • Median f/u 34 months • 30% remained alive and disease free • TTP and OS was significantly associated with – Response – Absence of bilateral residual tumor – Absence of PNE
- 22. • N : 29 • Locally advanced or metastatic • Doce: 75mg/m2 d1, CDDP: 60mg/m2 d1, 5FU: 750mg/m2 day1-5 • Primary outcome: objective response • OR: 38.5% • Grade 3/4 toxicity: 65.5%
- 23. Advanced metastatic and relapsed disease • Palliative chemotherapy • Initial studies showed response to cisplatin • Recent studies have shown even better response on addition of taxanes • Virtually no data on second lien therapy • Upcoming data on EGFR blockade – Cetuximab, panitumumab
- 24. Studies in the metastatic settings
- 25. • N: 25 • Single agent paclitaxel 175mg/m2 q 3 wks • PR: 20% • Median PFS: 11wks • Median survival 32 weeks
- 26. • Retrospective anaysis • N: 26 • Taxane with platinum • Median PSF: 96days (approx: 13wks) • Median OS: 246 days (approx: 35wks)
- 27. • Case reports • 2 cases • Prolonged survival
- 28. Place of targeted therapies • Retrospective • 13 pts • Median PFS: 3.2mo • Median OS: 9.8mo
- 30. Thank you