Cardiac arrest cpr shock
- 1. CARDIAC ARREST/ CARDIO PULMONARY RESUCITATION/ SHOCK Dr. Boudhayan Bhattacharjee
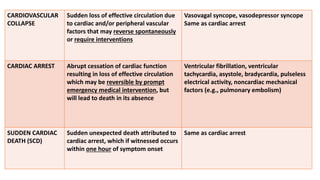
- 2. CARDIOVASCULAR COLLAPSE Sudden loss of effective circulation due to cardiac and/or peripheral vascular factors that may reverse spontaneously or require interventions Vasovagal syncope, vasodepressor syncope Same as cardiac arrest CARDIAC ARREST Abrupt cessation of cardiac function resulting in loss of effective circulation which may be reversible by prompt emergency medical intervention, but will lead to death in its absence Ventricular fibrillation, ventricular tachycardia, asystole, bradycardia, pulseless electrical activity, noncardiac mechanical factors (e.g., pulmonary embolism) SUDDEN CARDIAC DEATH (SCD) Sudden unexpected death attributed to cardiac arrest, which if witnessed occurs within one hour of symptom onset Same as cardiac arrest
- 3. DEMOGRAPHY âĒ Most Sudden cardiac arrests (SCA) occur outside hospital âĒ Fewer than 10% survive to be discharged from hospital despite after attempted resuscitation by emergency medical services (EMS) âĒ Women have a lower incidence of SCD and SCA than men âĒ Women are more likely to present with pulseless electrical activity (PEA) and to have their SCD occur at home as compared to men âĒ Black as opposed to white Americans have higher rates of SCD and are more likely to have unwitnessed arrests, to be found with PEA, and have worse rates of survival. âĒ Hispanic ethnicity appear to have lower rates of SCD, despite having a higher prevalence of cardiac risk factors âĒ Incidence of SCD may be relatively low among Asian populations as well, both within the United States and globally
- 4. PRECIPITATING FACTORS ï§ Time: Morning hours, late afternoon; winter in northern hemisphere, summer in southern hemisphere ï§ Location: Trains, airports, urban areas, living near roadways ï§ Certain activities and exposure: Earthquake, terrorist attacks; vigorous exercises
- 5. ETIOLOGY ï§ Cardiac causes: a) Coronary artery disease (40-70%)- Ischemic heart disease b) Non- ischemic heart disease- Cardiomyopathies. Arrythmias (VT, VF, PEA), Congenital heart disease, valvular heart diseases (MVPS, MR, AS), WPW, electrolyte abnormalities ï§ Non- cardiac causes: Stroke, Pulmonary embolism, aortic dissection, exsanguination, tension pneumothorax, sepsis, medication overdose, neurogenic
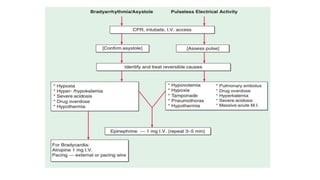
- 6. TREATABLE CAUSES OF CARDIAC ARREST ï§ Hypoxia ï§ Hypovolemia ï§ Hydrogen ion (acidosis) ï§ Hypo-/hyperkalaemia ï§ Hypothermia ï§ Toxins ï§ Tamponade (cardiac) ï§ Tension pneumothorax ï§ Thrombosis (pulmonary) ï§ Thrombosis (coronary)
- 7. SIGNS & SYMPTOMS ï§ Unconsciousness ï§ No breathing ï§ No blood pressure ï§ Pupils dilated (within 45 seconds) ï§ Seizures ï§ Death- like appearance ï§ Lips & nail beds- turns blue Diagnosis: Lack of carotid pulse
- 8. âOUT-OF-HOSPITAL CHAIN OF SURVIVALâ ï§ Initial evaluation and recognition of the SCA ï§ Rapid initiation of cardiopulmonary resuscitation (CPR) with an emphasis on chest compressions ï§ Defibrillation as quickly as possible usually with an automatic external defibrillation(AED) applied by the lay rescuer or EMT ï§ Basic and advanced EMS ï§ Advanced life support and postcardiac arrest care Initial goal of resuscitation is - achieve the return of spontaneous circulation Success is related to the time between collapse and initiation of resuscitation, decreasing markedly after 5 min, and the rhythm at the time of EMT arrival, being best for VT (25â30%), worse for VF and poor for PEA and asystole (<5%).
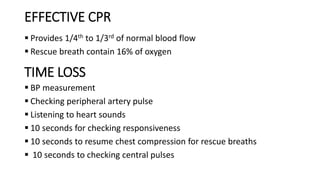
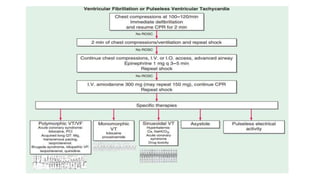
- 11. EFFECTIVE CPR ï§ Provides 1/4th to 1/3rd of normal blood flow ï§ Rescue breath contain 16% of oxygen TIME LOSS ï§ BP measurement ï§ Checking peripheral artery pulse ï§ Listening to heart sounds ï§ 10 seconds for checking responsiveness ï§ 10 seconds to resume chest compression for rescue breaths ï§ 10 seconds to checking central pulses
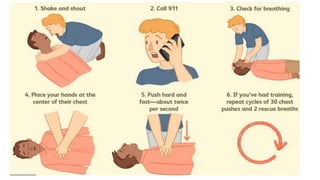
- 12. CIRCULATION- AIRWAY- BREATHING (CAB) ï§ Circulation: chest compressions (100-120/min) ï§ Airway: Head tilt, chin lift (open airways) ï§ Breathing: Rescue breaths (30:2= compressions: breath; victimâs nose pinch; over one second; with visible chest rise) ADVANCED AIRWAY- 8-10 breaths/min (not synchronised with compressions) RESCUER- one/two; interchange every two minutes
- 13. WHEN TO STOP CPR âĒ Revives and starts breathing âĒ Advanced medical help arrives âĒ Exhaustion of rescuer âĒ Death âĒ Time of onset of CPR >6 minutes: continue for 15 minutes âĒ Time of onset of CPR <6 minutes: continue for 30 minutes
- 16. AFTER RETURN OF SPONTANEOUS CIRCULATION (ROSC) âĒ SpO2 âĨ 94% âĒ Do not hyperventilate âĒ Advanced airway capnography âĒ Treat hypotension (SBP< 90 mm of Hg)- IV fluid bolus, vasopressors, consider treatable causes, do ECG âĒ Induce hypothermia âĒ Cardiac catheterisation