Case Study - Medical Error.pptx
- 1. ŌĆ£Biopsy results of two patients mixed upŌĆØ
- 2. Objectives 1. Describe the case study 2. Describe the theoretical model 2. Analysis of the case for root causes 4. Study how to prevent its recurrence suggesting recommendations
- 3. Case Study Mr: O : Consultant Urologist Dr: P : SHO Pathology Dr: R : Consultant Pathologist Mr A & Mr B : Patients undergoing Trans-Rectal US guided needle biopsy of prostate.
- 4. Case Study ct.. ’éŚ Two prostatic biopsy samples : taken (from Mr A & Mr B); ’éŚ Each sample: labelled with relevant patientŌĆÖs details; ’éŚ Labelled samples: sent to path lab with relevant request forms; ’éŚ In the lab: slides were prepared; and sent to SHO with their relevant request forms; ’éŚ Each slide : examined first by SHO & findings noted down; ’éŚ Both slides : taken to const. pathologist; to be reviewed together; ’éŚ Diagnosis made; 1. Prostate Cancer 2. Benign Prostatic Hyperplasia (BPH)
- 5. Case Study ct.. ’éŚ Consultants findings: written on back of each patientŌĆÖs request form by SHO; ’éŚ Findings from each request form: taken to a tape; each tape was attached to corresponding request form; sent to secretary to computerize; computer reports were double checked and matched with request forms; ’éŚ Reports sent to cont. Urologist; ’éŚ Mr: A: No cancer (BPH); No treatment ’éŚ Mr: B: Adenocarcinoma; Radiotherapy
- 6. Identification of the medical error: ’éŚ One year later: Mr: A : High S. PSA; ’éŚ Repeat needle biopsy : adenocarcinoma diagnosed
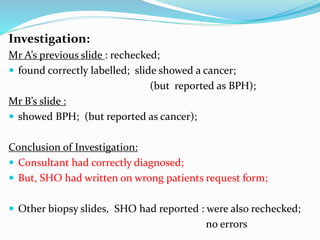
- 7. Investigation: Mr AŌĆÖs previous slide : rechecked; ’éŚ found correctly labelled; slide showed a cancer; (but reported as BPH); Mr BŌĆÖs slide : ’éŚ showed BPH; (but reported as cancer); Conclusion of Investigation: ’éŚ Consultant had correctly diagnosed; ’éŚ But, SHO had written on wrong patients request form; ’éŚ Other biopsy slides, SHO had reported : were also rechecked; no errors
- 8. Disclosure: ’éŚ Mr: O (urologist) met each patient and apologized; ’éŚ explained what happened. Consequences: Two patients harmed by single slip up; ’éŚ One yearŌĆÖs delay in treating Mr A could significantly affect the prognosis; ’éŚ Mr B was subjected to an unnecessary course of radiotherapy. All other checks : invalidated by a single mistake resulting in great consequences.
- 9. A- Biopsy B-Biopsy A- Biopsy B-Biopsy one sample: benign one sample adeno carcinoma A- PSA gradually increasing A-no treatment follow up PSA B- Underwent radiotherapy A- Benign report B-adenocarcinoma of prostate A- Adeno carcinoma Ex by Dr P Ex by dr P & R Enter into com One year later Dr O Repea t Bx
- 10. Swiss cheese model of Accident causation In this model , errors made by individuals result in disastrous consequences due to flawed system- ŌĆ£the holes in the cheeseŌĆØ
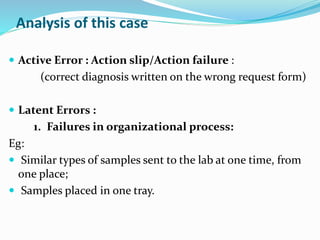
- 11. Analysis of this case ’éŚ Active Error : Action slip/Action failure : (correct diagnosis written on the wrong request form) ’éŚ Latent Errors : 1. Failures in organizational process: Eg: ’éŚ Similar types of samples sent to the lab at one time, from one place; ’éŚ Samples placed in one tray.
- 12. Analysis Ct.. 2. Back ground factors: (Work load, Communication, Supervision etc) Eg: ’éŚ Identity of slides & request forms - not double checked by two personnel; ’éŚ No accountability of consultant for the accuracy of diagnosis; ’éŚ No computer reports checked against patient identification details and diagnosis on the request form
- 13. Recommendations Organizational process should be improved: ’éŚ Process mapping and documented clear guidelines to each level of the staff. ’éŚ Similar types of samples should be separated in the lab; ’éŚ They should be placed in separate trays; Back ground factors should be improved: ’éŚ ║▌║▌▀Ż matched with the identity on the request form by the consultant; ’éŚ Request forms signed by consultant for the accuracy of diagnosis ’éŚ Computer reports to be checked against both patient identification details and diagnosis on the request form.
- 14. Sample checked and received by lab counter ║▌║▌▀Ż and request form : separate tray SHO Ex Bx Rechecked & signed by consultant Generate the report Consultant Ex Bx colour coding Positive reports informed over the phone lf mismatch : discussion Recheck: identity and findings
- 15. Recommendations ct.. ’éŚ Implement an Adverse Event Reporting System, system of root cause analysis with a constructive feed back system. ’éŚ Motivate staff to foster a Patient Safety Culture. ’éŚ Establish a culture where patient safety issues are discussed openly, staff and patients treated fairly; promoting learning & communicating experience to mitigate future incidents.
- 16. Summary ’éŚ Case Study of a Medical Error with mixed up lab reports. ’éŚ Two patients were harmed by single failure. ’éŚ Both Active Errors (Action failure) and Latent Errors (Failures in organizational process & Back ground factors) were identified as causative factors. ’éŚ Strengthening of Patient Safety Culture was recommended.
- 17. Thank You