Catract ppt
- 1. CATARACT
- 2. ANATOMY OF THE LENS STRUCTURE OF THE LENS: ? LENS CAPSULE ? ANTERIOR LENS EPITHELIUM ? LENS FIBER
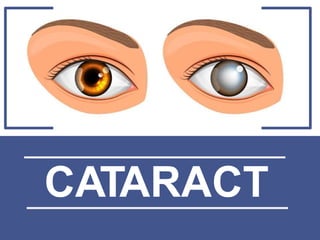
- 3. CATARACT WHAT IS CATARACT? Cataract is a clouding of the lens or any opacity within the lens which leads to a decrease in vision
- 4. DEFINITION ? A cataract is a clouding of the normally clear lens of eye ? A cataract is a dense, cloudy area that forms in the lens of the eye. ? A cataract begins when proteins in the eye form clumps that prevent the lens from sending clear images to the retina. ? The retina works by converting the light that comes through the lens into signals. It sends the signals to the optic nerve, which carries them to the brain.
- 5. CATARACT
- 6. RISK FACTORS ? Increasing age (protein break in lens) ? Diabetes ? Excessive exposure to sunlight ? Smoking ? Obesity ? High blood pressure ? Previous eye injury or inflammation ? Previous eye surgery ? Prolonged use of corticosteroid medications ? Drinking excessive amounts of alcohol ? an overproduction of oxidants, which are oxygen molecules that have been chemically altered due to normal daily life ? ultraviolet radiation ? Trauma ? Nutritional deficiency ©C vitamin- A, B1, C
- 7. INCIDENCE Incidence of Lens opacities in the Ī░normalĪ▒ population with aging. (Cinotti & Patti,1968) AGE GROUP (YEARS) LENS OPACITY (%) 50 ©C 59 65 60 ©C 69 83 70 ©C 79 91 > 80 100
- 8. CAUSES CONGENITAL AGE METABOLIC ? Familial ? Intrauterine infections ? Maternal drug ingestions ? Elderly ? Diabetes ? Hypocalcaemia ? WilsonĪ»s Disease ? Galactosemia
- 9. CAUSES DRUG - INDUCED TRAUMATIC AND INFLAMMATORY DISEASE ASSOCIATED ? Corticosteroids ? Miotics ? Amiodarone ? Phenothiazines ? Post intra-ocular surgery ? Uveitis ? DownĪ»s Syndrome ? Dystrophia Myotonica ? LoweĪ»s Syndrome ? Atopic dermatitis
- 10. CLASSIFICATION MORPHOLOGICAL CLASSIFICATION 1. Subcapsular cataract - Anterior subcapsular cataract - Posterior subcapsular cataract 2. Nuclear cataract - Involves the nucleus of lens. Yellow to brown coloration 3. Cortical cataract - Wedge shaped or radial spike-like opacities. 4. Polar cataract - Central posterior part of the lens
- 12. CLASSIFICATION
- 13. CLASSIFICATION HYPERMATURE Cataract is shrunken and wrinkled anterior capsule due to leakage of water out of the lens MORGAGNIAN Cataract is a hypermature cataract in which liquefaction of the cortex has allowed the nucleus to sink inferiorly BASED ON DEGREE OF MATURITY MATURE IMMATURE Cataract is one in which the lens is completely opaque. Cataract is one in which the lens is partially opaque.
- 14. MATURE CATARACT
- 15. MATURE VS IMMATURE HOW TO DIFFERENTIATE MATURE AND IMMATURE CATARACT? IMMATURE CATARACT MATURE CATARACT ? Visual acuity is reduced to counting fingers ? Visual acuity is reduced to hand movement or perception of light ? Lens is partially opaque ? Lens in totally opaque ? Fundus may be visible ? No fundus details
- 17. MORGAGNIAN CATARACT ? Complete cortex is liquefied and appears milky white in colour. ? Nucleus settles at the bottom ? Calcium deposits may also be seen on the lens capsule.
- 18. CLINICAL PRESENTATION ? Painless Clouded, blurred or dim vision ? Increasing difficulty with vision at night ? Sensitivity to light and glare ? Need for brighter light for reading and other activities ? Seeing "halos" around lights ? Frequent changes in eyeglass or contact lens prescription ? Fading or yellowing of colors ? Double vision in a single eye ? color shift (the aging lens become progressively more absorbent at the blue end of the spectrum) ? Brunescens (color values shift to yellow-brown)
- 19. VISUAL ACUITY Blurred vision due to scattering of light on the retina
- 20. VISUAL ACUITY
- 21. VISUAL ACUITY
- 22. LENS OPACITY Normal eye ©C Good red reflex Cataractous eye ©C Poor red reflex
- 23. DIAGNOSIS ? History collection of patient ? Physical examination ? Snellen Visual acuity test ? Opthalmoscopy- visualization of eye ? Retinoscopy- Retinal exam
- 24. MANAGEMENT
- 25. TREATMENT The aim of treatment is: 1. Improve vision 2. Increase mobility and independence 3. Relief from the fear of going blind
- 26. INDICATIONS 1. Work or lifestyle is affected by vision problems caused by the cataract. 2. Glare caused by bright lights is a problem. 3. Cannot pass a vision test 4. Have double vision. 5. Notice a big difference in vision when you compare one eye to the other. 6. Have another vision-threatening eye disease, such as diabetic retinopathy or macular degeneration.
- 27. TREATMENT The treatment of cataracts is : 1. Glasses 2. Better lighting 3. Surgery a. Phacoemulsification b. ECCE ( Extracapsular Cataract Extraction) c. ICCE (not performed now) Sometimes a cataract should be removed even if it doesn't cause major problems with vision, if it is preventing the treatment of another eye problem, such as age-related macular degeneration, diabetic retinopathy or retinal detachment
- 28. SURGERY: ECCE ? Extracapsular cataract extraction ? An 5 mm to 6 mm incision is made in the eye where the clear front covering of the eye (cornea) meets the white of the eye (sclera). ? Another small incision is made into the front portion of the lens capsule. The lens is removed, along with any remaining lens material. ? An IOL may then be placed inside the lens capsule. And the incision is closed. *it is usually done if the cataract is too large to be destroyed by ultrasound
- 29. SURGERY: ECCE
- 30. SURGERY: ICCE ? Intracapsular cataract extraction ? Involves extraction of the entire lens, including the posterior capsule and zonules ? Weak and degenerated zonules are a pre-requisite for this method ? This is the surgery of choice if there is markedly subluxated or dislocated lens ? This technique of surgery has largely been replaced by ECCE
- 31. COMPLICATIONS 1. Infection in the eye (endophthalmitis). 1. Swelling and fluid in the center of the nerve layer (cystoid macular edema). 1. Swelling of the clear covering of the eye (corneal edema). 1. Bleeding in the front of the eye (hyphema). 1. Detachment of the nerve layer at the back of the eye (retinal detachment).
- 32. ICCE VS ECCE ECCE ICCE Small incision 5-6mm Large incision 10-12mm Posterior lens conserved Removal entire lens No stiches required, self healing Required stiches, long rehabilitation time IOL implant Aphakic eye Post operative complication minimal Added risk for retinal detachment, corneal edema and vitreous loss
- 33. PHARMACOEMULSIFICATION ? Two small incisions are made in the eye where the clear front covering (cornea) meets the white of the eye (sclera). ? A circular opening is created on the lens surface (capsule) ? A small surgical instrument (phaco probe) is inserted into the eye. ? Sound waves (ultrasound) are used to break the cataract into small pieces. Sometimes a laser is used too. The cataract and lens pieces are removed from the eye using suction. ? An intraocular lens implant (IOL) may then be placed inside the lens capsule. ? Usually, the incisions seal themselves without stitches.
- 35. INTRAOCULAR LENS ? Insertion of IOLs during cataract surgery is the usual approach to lens replacement. After cataract extraction, or phacoemulsification, the surgeon implants an IOL. ? IOL implantation is contraindicated in patients with recurrent uveitis, proliferative diabetic retinopathy, glaucoma.
- 36. THANK YOU