CENTRAL VENOUS PRESSURE MONITORINGG.pptx
- 1. CVP MONITORING PRESENTER- MAJ ANKUSH MALHOTRA MODERATOR- COL JOSEMINE DAVIS
- 2. Definition Central venous pressure is considered as a direct measurement of the blood pressure in the right atrium and it is used to determine preload and the filling pressure of heart. Normal value- 8-12 mm of Hg
- 3. Physiology behind CVP monitoring ` Two prerequisites must be met in order to correctly interpret the information provided by the CVP monitor: ŌŚÅ (a) The clinician must possess a thorough understanding of all the variables that affect right atrial pressure. ŌŚÅ (b) Measurements need to be made with extreme attention to detail. CVP is determined by the interaction of the venous return function of the circulatory system and the cardiac function.
- 4. Physiology behind CVP monitoring ŌŚÅ An increase in cardiac function with an increase in venous return will result in an increase in cardiac output and rise in CVP. ŌŚÅ An increase in cardiac function without an increase in venous return will result in an increase in cardiac output and a fall in CVP. ŌŚÅ An isolated CVP measurement has very little meaning unless the information is interpreted in the context of some estimation of cardiac function.
- 5. CVP and Venous Return ŌŚÅ Venous return is mostly determined by the gradient between the mean circulatory filling pressure (MCFP) and CVP. ŌŚÅ MCFP results from the elastic recoil pressure from distended small veins and venules and is the force that drives blood back to the right atrium. ŌŚÅ Two important corollaries emerge: ŌŚŗ right atrial pressure is key for maintaining cardiac output. ŌŚŗ The body will compensate through the mechanisms described above and others to preserve venous return.
- 6. CVP and Venous Return ŌŚÅ This explains why a patient may lose 10% to 12% of his circulating blood volume without exhibiting changes in blood pressure or CVP. ŌŚÅ The difference between MCFP and CVP is only 6 to 8 mm Hg, and hence small changes in CVP may have profound hemodynamic consequences.
- 7. CVP and Cardiac Function ŌŚÅ Changes in CVP may be the sole result of changes in inotropic state or compliance of the ventricle, independent of the total circulating volume or venous return to the heart. ŌŚÅ CVP is the result of a complex and diverse interplay among many different physiologic variables, many of which are impossible to measure in the operating room or ICU. ŌŚÅ It is therefore not surprising that studies assessing the value of CVP as a predictor of volume status or fluid responsiveness have failed to demonstrate a relationship.
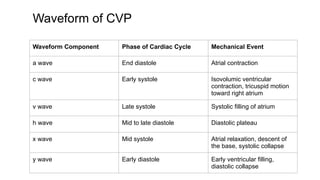
- 8. Waveform of CVP Waveform Component Phase of Cardiac Cycle Mechanical Event a wave End diastole Atrial contraction c wave Early systole Isovolumic ventricular contraction, tricuspid motion toward right atrium v wave Late systole Systolic filling of atrium h wave Mid to late diastole Diastolic plateau x wave Mid systole Atrial relaxation, descent of the base, systolic collapse y wave Early diastole Early ventricular filling, diastolic collapse
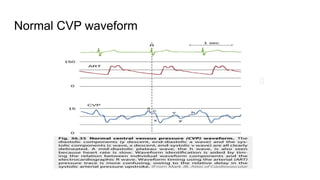
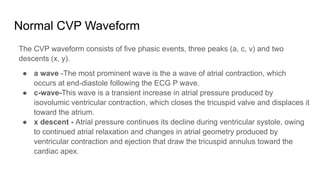
- 10. Normal CVP Waveform The CVP waveform consists of five phasic events, three peaks (a, c, v) and two descents (x, y). ŌŚÅ a wave -The most prominent wave is the a wave of atrial contraction, which occurs at end-diastole following the ECG P wave. ŌŚÅ c-wave-This wave is a transient increase in atrial pressure produced by isovolumic ventricular contraction, which closes the tricuspid valve and displaces it toward the atrium. ŌŚÅ x descent - Atrial pressure continues its decline during ventricular systole, owing to continued atrial relaxation and changes in atrial geometry produced by ventricular contraction and ejection that draw the tricuspid annulus toward the cardiac apex.
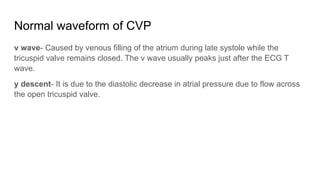
- 11. Normal waveform of CVP v wave- Caused by venous filling of the atrium during late systole while the tricuspid valve remains closed. The v wave usually peaks just after the ECG T wave. y descent- It is due to the diastolic decrease in atrial pressure due to flow across the open tricuspid valve.
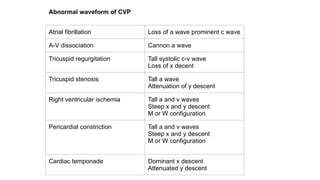
- 12. ŌŚÅ Atrial fibrillation- a wave disappears and the c wave becomes more prominent because atrial volume is greater at end-diastole and onset of systole, owing to the absence of effective atrial contraction. ŌŚÅ Atrioventricular dissociation- Atrial contraction now occurs during ventricular systole when the tricuspid valve is closed, thereby inscribing a tall ŌĆ£cannonŌĆØ a wave in the CVP waveform. Abnormal waveform of CVP
- 13. Abnormal waveform of CVP ŌŚÅ Tricuspid regurgitation- It produces abnormal systolic filling of the right atrium through the incompetent valve. A broad, tall systolic c-v-wave results, beginning in early systole and obliterating the systolic x descent in atrial pressure. ŌŚÅ Tricuspid stenosis-Produces a diastolic defect in atrial emptying and ventricular filling. The a wave is unusually prominent and they descent is attenuated, owing to the impaired diastolic egress of blood from the atrium.
- 14. Atrial fibrillation Loss of a wave prominent c wave A-V dissociation Cannon a wave Tricuspid regurgitation Tall systolic c-v wave Loss of x decent Tricuspid stenosis Tall a wave Attenuation of y descent Right ventricular ischemia Tall a and v waves Steep x and y descent M or W configuration Pericardial constriction Tall a and v waves Steep x and y descent M or W configuration Cardiac temponade Dominant x descent Attenuated y descent Abnormal waveform of CVP
- 15. Physiological Pressure Monitoring ŌŚÅ Multilumen central venous catheter (15-20 cm in length) that is inserted in the subclavian or internal jugular veins and advanced into superior vena cava. ŌŚÅ The CVP is hydrostatic pressure, so it is important that fluid filled transducer is at the same level as right atrium. ŌŚÅ Reference point - intersection of midaxillary line and fourth intercostal space.
- 16. Physiological Pressure Monitoring Components of physiological Pressure measurement ŌŚÅ Invasive catheter ŌŚÅ Pressure transducer ŌŚÅ Normal saline flush ŌŚÅ Pressure infusion bag ŌŚÅ Reusable pressure cable ŌŚÅ Bedside physiological monitor
- 17. Levelling pressure transducer system ŌŚÅ Intravascular monitoring should be at the level of heart or phlebostatic axis. ŌŚÅ Should be done with a CarpenterŌĆÖs level. ŌŚÅ Errors in pressure reading may occur if alignment with phlebostatic axis is not maintained. ŌŚÅ For every inch (2.5 cm) the heart is offset from the reference point of the transducer, a 2 mmHg of error will be introduced.
- 18. Levelling pressure transducer system
- 19. Levelling pressure transducer system
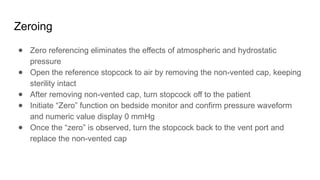
- 20. Zeroing ŌŚÅ Zero referencing eliminates the effects of atmospheric and hydrostatic pressure ŌŚÅ Open the reference stopcock to air by removing the non-vented cap, keeping sterility intact ŌŚÅ After removing non-vented cap, turn stopcock off to the patient ŌŚÅ Initiate ŌĆ£ZeroŌĆØ function on bedside monitor and confirm pressure waveform and numeric value display 0 mmHg ŌŚÅ Once the ŌĆ£zeroŌĆØ is observed, turn the stopcock back to the vent port and replace the non-vented cap
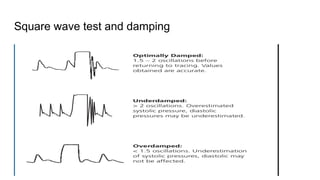
- 21. Square wave test and damping 1. Activate snap or pull tab on flush device 2. Observe square wave generated on bedside monitor 3. Count oscillations after square wave 4. Observe distance between the oscillations
- 22. Square wave test and damping
- 24. CVP values provide important information about the cardiocirculatory status of the patient and should not be abandoned. Use of CVP to guide fluid resuscitation has many limitations, but we believe it is wiser to understand and take into account these limitations rather than to discard CVP completely.
- 25. Thank you
- 26. Indication ŌŚÅ Measurement of right heart filling pressure to assess intravascular volume and right heart function. ŌŚÅ Presence of persistent hypotension despite of fluid resuscitation despite fluid resuscitation ŌŚÅ Vasopressor therapy ŌŚÅ Extensive third space losses ŌŚÅ Oliguria Or Anuria ŌŚÅ Trauma ŌŚÅ Sepsis ŌŚÅ Major surgeries ŌŚÅ Burns ŌŚÅ Heart failure
- 27. Complications of CVP Mechanical ŌŚÅ Arterial ŌŚÅ Venous ŌŚÅ Cardiac tamponade ŌŚÅ Pneumothorax ŌŚÅ Airway compression from hematoma ŌŚÅ Nerve injury ŌŚÅ Arrhythmias Thromboembolic ŌŚÅ Venous thrombosis ŌŚÅ Pulmonary embolism ŌŚÅ Arterial thrombosis and embolism Catheter or guidewire embolism Infectious ŌŚÅ Insertion site infection ŌŚÅ Catheter infection ŌŚÅ Bloodstream infection ŌŚÅ Endocarditis