Cerebellarexaminationdemyer2 180912212324-converted
- 2. CLINICAL SIGNS OF CEREBELLAR DYSFUNCTION *4 cardinal cerebellar signs consist of 1 Ataxia (=dystaxia) 2Tremor (intention tremor and postural)or static type of action tremor or end-point, or kinetic tremor 3hypotonia 4- Asthenia. *The unsteady oscillations of the head and trunk are also called titubation, occur a few times per second, and while it may be seen in cerebellar dysfunction is not pathognomonic or localizing. * The uncoordinated, slurred speech is called dysarthria, like any neurogenic disturbance of voice articulation
- 3. # The effect of cerebellar lesions on speech 1 Dysarthria (slowness, slurring of words) 2scanning speech: the PtĪ»s voice varies from a low volume to a high volume as if scanning from peak to peak. Thus accentuating the wrong syllables or words. # The effects of cerebellar lesions on eye movement 1- Nystagmus(gaze evoked) 2Dysmetria of saccades: have the Pt look straight ahead and place your index fingers in the temporal fields. Ask the Pt to look first at one finger and then the other and then direct the Pt to look rapidly from one to the other several times and it will be noted that the eyes over or undershoot the target. 3 Jerky rather than smooth pursuit 4Slowness in initiating eye movements 5- Skew deviation
- 4. # Clinical tests for dystaxia of station (stance) and gait *Inspect the Pt for swaying when standing, and for ataxia of gait. * lateropulsion is the tendency to move from side to side. *To compensate for unsteadiness of stance and gait, the cerebellar Pt assumes a broad-based stance and a broad-based gait, just as a toddler does before gaining coordination, or an elderly os asks the Pt to stand with the feet together. *Ask the Pt to step along a straight line, placing the heel of one foot directly in front of the toe of the other, the so-called tandem walking, a sensitive test for gait ataxia.
- 5. Clinical tests for arm dystaxia 1- Postural tremor and tremor of the arms during the finger- to-nose test a. Ask the Pt to extend the arms straight out in front: -Inspect the arms for wavering indicating incoordination for frank, rhythmic postural tremor. -Having the Pt hold the fingers a little apart in front of the nose, with the arms elevated horizontally, in Ī░the batswingĪ▒ position, also demonstrates postural instability of the arms or postural tremor b. Do finger nose test: look for intention tremor , dysmetria And dysenergia. - A tremor of the outstretched hands is called a postural tremor. -A tremor that increases as the finger approaches the nose or is reaching a target is called a (Positional Intention type of kinetic tremor (called terminal or end-point tremor by some investigators) tremor.
- 6. - Dysmetria: undershoots or overshoots the target during finger nose test. 2- The rapid alternating-movements tests for dystaxia and dysmetria (dysdiadochokinesia) * The Pt holds out the hands and pronates and supinates them as rapidly as possible. Test the hands separately and together.
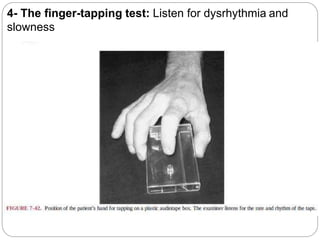
- 7. 4- The finger-tapping test: Listen for dysrhythmia and slowness
- 8. Overshooting and checking tests of the arms 1- Rebound sign: * Pt stand with eyes closed and arms outstretched. *Tell the Pt, Ī░I am going to tap your arms. Hold them still. Do not let me budge them. *The Ex delivers to the back of the PtĪ»s wrist a quick push, strong enough to displace the arm. *The normal subjectĪ»s arm returns quickly to its initial position. # The cerebellar PtĪ»s arm oscillates back and forth , It overshoots several times 2- The arm-pulling test : * The Ex pulls hard against the PtĪ»s flexed arm. When the Ex suddenly releases the PtĪ»s arm, the cerebellar Pt fails to check the armĪ»s flight
- 10. Clinical tests for leg dystaxia: 1. heel-to-shin test : * Have the Pt supine (or sitting). *Instruct the Pt to place one heel precisely on the opposite knee,Then direct the Pt to run the heel in a straight line precisely down the shin * observe for a positional tremor 2. heel-tapping test: *ask the Pt to place one heel over the other shin and to tap the shin with the heel as rapidly as possible on one spot. *The cerebellar Pt misses the spot (dysmetria) and taps dysrhythmically (dysdiadochokinesia).
- 11. 3- Gait examination: a.If the patient is able to walk, a good test of lower limb coordination consists of asking him to walk along a straight line. b.Tandem walk: Ask the patient to walk along straight line on the floor placing the heel of one foot immediately adjacent to the toe of the one behind. 4. Combus test: Ask the patient to walk to a known point and then to return back to the original place. In patient with cerebellar lesion he will continuously deviate to the side of the lesion until he finally makes a combus.
- 12. Clinical tests for hypotonia *Muscle tone is defined as the muscular resistance the Ex feels when moving the PtĪ»s resting extremity(Passive movement) *Hypotonic Pt assumes floppy postures ,rag-doll or dumped-in-a-heap postures. *When walking, the hypotonic Pt presents a floppy, sagging, loose-jointed appearance. *The arms fail to swing properly, the knees may bend backward slightly (genu recurvatum), and the head and trunk bobĪ¬a rag-doll gait, as seen in drunkenness.
- 13. # Pendular or hypotonic muscle stretch reflexes (MSRs) * In cerebellar Pts: After the quadriceps MSR is elicited, the leg normally stops swinging after one or two excursions but The cerebellar PtĪ»s leg swings to-and-fro several times, like a pendulum. # Effect of cerebellar lesions on strength and endurance *The cerebellar Pt may experience mild asthenia, that is, weakness, fatigability, and a reluctance to move. *Destruction of the pathway that connects the cerebellar cortex with the cerebral motor cortex might explain the asthenia.