Cervical Lymphadenopathy
Download as PPTX, PDF38 likes11,695 views
Differential Diagnosis of Cervical Lymph node enlargement OTORHINOLARNGOLOGY EAR, NOSE and THROAT TOPIC
1 of 16
Downloaded 118 times






Recommended
Cervical lymphadenopathy



Cervical lymphadenopathymac os
╠²
Cervical lymphadenopathy refers to abnormal enlargement of lymph nodes in the neck. The document discusses the anatomy and classification of cervical lymph nodes. Characteristics of enlarged lymph nodes that suggest malignancy include size greater than 2 cm, hard or firm consistency, fixation to surrounding tissues, and location in supraclavicular or parotid regions. Evaluation of lymphadenopathy depends on characteristics of the nodes, patient age and symptoms, with concerning signs warranting further workup.Salivary gland tumor



Salivary gland tumorMahesh Raj
╠²
The document summarizes salivary gland tumours. It discusses the various types of benign and malignant salivary gland tumours, their locations, characteristics, risk factors, clinical features, investigations and treatments. The major tumours discussed include pleomorphic adenoma, adenolymphoma, mucoepidermoid carcinoma and adenoid cystic carcinoma. It provides details on the incidence, presentation and management of tumours in the parotid, submandibular and minor salivary glands.Ludwigs angina



Ludwigs anginaPraveena Veena
╠²
Ludwig's angina is a serious neck infection that can compromise the airway. It involves the sublingual and submandibular spaces and spreads through connective tissue planes. The infection is usually polymicrobial, involving bacteria like Streptococcus and Staphylococcus. It commonly originates from an odontogenic infection. Symptoms include neck swelling, difficulty swallowing and breathing. Immediate priorities in treatment are airway protection through intubation or tracheostomy and IV antibiotics.Salivary glands disorders ii



Salivary glands disorders iiIAU Dent
╠²
The document discusses various salivary gland disorders including infections, inflammatory conditions, cysts, tumors and other pathologies. It provides details on:
- Acute and chronic bacterial sialadenitis, most commonly caused by retrograde infection from the mouth. Acute infections more often affect the parotid gland.
- Viral infections like mumps can cause acute non-suppurative sialadenitis. Mumps is spread through droplets and involves the parotid glands.
- Sj├Čgren's syndrome is an autoimmune condition characterized by lymphocytic destruction of exocrine glands causing dry mouth and eyes. Diagnosis involves labial biopsy.
- Common benign salParotid tumors



Parotid tumorsSharath !!!!!!!!
╠²
The parotid gland is located below and in front of the ear. It has two lobes and is drained by Stenson's duct which opens into the mouth. The gland has a capsule and structures like arteries pass through it. It is supplied by parasympathetic and sympathetic nerves. Common tumors include pleomorphic adenoma and Warthin's tumor. Mucoepidermoid carcinoma and adenoid cystic carcinoma are malignant tumors that can occur. Surgical excision is the main treatment for tumors but radiotherapy may also be used for malignant ones. Complications after parotidectomy include facial nerve injury and salivary fistula.Midline swellings of the neck



Midline swellings of the neckpeace10136
╠²
This document discusses various causes of midline neck swellings, including congenital, infectious, inflammatory, and neoplastic etiologies. It provides details on specific conditions such as thyroglossal duct cyst, laryngocele, Ludwig's angina, sublingual dermoid cyst, reactive lymphadenopathy, thyroid disorders, and laryngeal malignancy. Treatment options vary depending on the underlying cause but may include antibiotics, incision and drainage, surgery, radiotherapy, or a combination of therapies.Salivary gland disorders



Salivary gland disordersSaleh Bakry
╠²
The document discusses salivary gland disorders. It begins with definitions and classifications of salivary glands. It then discusses the anatomy, functions, and disorders of the parotid, submandibular, and sublingual salivary glands. Diagnostic aids are outlined including clinical history, physical examination, imaging such as CT, MRI, ultrasound and sialography. Cystic conditions of the minor salivary glands such as mucoceles are also summarized. Disorders are classified and inflammatory, obstructive, neoplastic and other conditions are described.Examination of Swelling



Examination of SwellingSANDEEP KASHYAP
╠²
This document provides an overview of examining swellings in the head and neck region. It begins with definitions of key terms like swelling, cyst, and lump. It then classifies swellings based on location and etiology. The document outlines the important components of physically examining a swelling, including inspection, palpation, percussion, and auscultation. It describes the process of taking a patient history. Key investigations that can be performed for swellings are also summarized, including x-rays, ultrasound, biopsy and more. Differential diagnoses and management strategies are also briefly mentioned.Ameloblastoma



Ameloblastomasakshat Lamichhane
╠²
Benign, locally aggressive tumor of odontogenic epithelium, Previously called adamantinoma, Second most common odontogenic tumor after odontoma, Mandible is most common site, Usually asymptomatic and can be found incidentally on routine dental examinationsCarcinoma tongue



Carcinoma tongueViswa Kumar
╠²
This document discusses the anatomy, etiology, clinical presentation, staging, and treatment options for carcinoma of the tongue. It notes that carcinoma of the tongue most commonly presents as a non-healing ulcer and can cause symptoms like otalgia, odynophagia, and bleeding. Treatment depends on staging and may involve surgery, radiation therapy, chemotherapy, or a combination. Prognosis decreases with more advanced stage at diagnosis.Diseases of-salivary-glands 



Diseases of-salivary-glands Weam Faroun
╠²
This document discusses diseases of the salivary glands, including sialadenitis (inflammation of the salivary glands), which can be caused by bacterial or viral infections. It also discusses Sjogren's syndrome, an autoimmune disease that causes dry mouth and dry eyes due to lymphocytic infiltration and destruction of the lacrimal and salivary glands. Obstructive diseases like salivary calculi (stones) are also covered. The document provides details on symptoms, diagnosis, and treatment of various salivary gland diseases.Odontogenic tumors ppt



Odontogenic tumors pptmadhusudhan reddy
╠²
This document discusses different types of odontogenic tumors. It classifies them into three categories: tumors of odontogenic epithelium, mixed odontogenic tumors, and tumors of odontogenic ectomesenchyme. Key tumors discussed include ameloblastoma, adenomatoid odontogenic tumor (AOT), and calcifying epithelial odontogenic tumor (CEOT). Ameloblastoma is the most common odontogenic tumor and can be solid/multicystic, unicystic, or peripheral. AOT typically occurs in younger females in the anterior maxilla. CEOT accounts for less than 1% of odontogenic tumors and resembles cells of the enamel organ or dental lamina.Oral cavity lesions



Oral cavity lesionsNotre Dame De Chartres Hospital
╠²
This document discusses various lesions that can occur in the oral cavity. It begins by defining mouth ulcers and listing common causes such as physical abrasion, infection, and cancer. It then covers specific conditions like recurrent aphthous stomatitis, lichen planus, pemphigus vulgaris, and necrotizing sialometaplasia. It provides details on symptoms, appearance, epidemiology, treatment and pathogenesis for each condition. In general, the document provides a comprehensive overview of acute and chronic ulcerative lesions that can present in the oral cavity.Weber ferguson incison (poster)



Weber ferguson incison (poster)Sk Aziz Ikbal
╠²
The Weber-Fergusson incision is indicated for access to tumors involving the maxilla extending superiorly to the infraorbital nerve and into or involving the orbit. It provides wide access to all areas of the maxilla. The incision line is drawn through the vermillion border along the filtrum of the lip, extending around the base of the nose along the facial nasal groove. It then extends infraorbitally below the cilium to the lateral canthus. Tarsorrhaphy sutures are placed in the eyelid. The incision is made through the skin and subcutaneous tissue along the nose, and the full thickness upper lip is transsected with ligation of the labial arteryTumor of oral cavity



Tumor of oral cavityshekhar star
╠²
The document discusses tumors and neoplasms of the oral cavity. It defines a tumor as a swelling of tissue, while neoplasia is an abnormal mass of tissue that exceeds normal growth. For simplicity, tumors and neoplasms are used interchangeably. Tumors of the oral cavity are classified based on their tissue of origin into epithelial, connective, muscle, nerve or metastatic tumors. Benign epithelial tumors include squamous papilloma and keratoacanthoma. Squamous papilloma presents as a painless, cauliflower-like growth caused by HPV infection, while keratoacanthoma is a potentially malignant growth associated with sun exposure. Both lesions can be surgically excised with low recurrence ratesOral malignancy



Oral malignancySaleh Bakry
╠²
This document discusses the clinical diagnosis and evaluation of oral malignancy. It covers:
- Performing a thorough clinical examination of the oral cavity and lymph nodes to check for abnormalities.
- Taking a detailed patient history regarding the lesion.
- Using radiographic imaging like x-rays and MRI to examine intraoral lesions and bone involvement.
- Conducting lab tests and biopsy of suspicious areas to confirm a diagnosis of oral cancer.
- Classifying oral cancers based on location, pathology, and extent of spread to aid in staging and treatment planning.Tumors of salivary gland



Tumors of salivary glandazfarneyaz
╠²
This document provides information on various types of salivary gland tumors. It begins with an overview of the major and minor salivary gland tumors that are most commonly seen in adults and children. Examples include Warthin tumor, acinic cell carcinoma, and polymorphous low-grade adenocarcinoma. The document then describes the histological features of many benign and malignant epithelial and nonepithelial salivary gland tumors at both the macroscopic and microscopic levels. Key diagnostic characteristics of tumors like pleomorphic adenoma, myoepithelioma, oncocytoma, and adenoid cystic carcinoma are highlighted.Parotidectomy



ParotidectomyPrashanth Lakshman
╠²
This document provides information about parotidectomy, which is the surgical removal of the parotid gland. It discusses the different types of parotidectomy including superficial and total parotidectomy. Superficial parotidectomy involves removing the superficial lobe of the parotid gland while preserving the facial nerve. The procedure is described in detail, including identifying landmarks to locate the facial nerve and carefully dissecting the gland superficial to the nerve. Complications involving the facial nerve are also addressed.Salivary glands diseases



Salivary glands diseasesIAU Dent
╠²
This document provides information on salivary gland diseases presented over multiple sessions. It begins with the objectives and overview of topics to be covered, including applied anatomy of the salivary glands, autonomic innervation and effects on function, inflammatory and obstructive disorders, neoplasms, and investigations. It then describes in detail the anatomy, physiology and investigations of the major salivary glands. Salivary gland diseases are classified as functional, obstructive, non-neoplastic and neoplastic. Specific conditions like sialadenitis, sialolithiasis, mucocele and ranula are explained. Imaging modalities like ultrasound, sialography, CT, MRI and sialendoscopyAetiology and management of trismus



Aetiology and management of trismusHope Inegbenosun
╠²
This document outlines the etiology and management of trismus. It defines trismus as restricted mouth opening and describes normal ranges of opening. Common causes of trismus include infections, trauma, surgery, tumors, radiation, TMJ disorders, and drugs. Management involves thorough history and examination, investigations to diagnose the underlying cause, and various treatment approaches depending on the etiology such as heat therapy, medical management, physiotherapy, surgery, and appliances.Sialolithiasis



SialolithiasisRuchi Rathi
╠²
Sialolithiasis refers to the formation of calcific stones within the salivary glands or ducts. The submandibular gland is most commonly affected. Clinical features include intermittent pain and swelling near the affected gland during or after meals. Investigations like radiography can detect radiopaque stones, while sialography or CT scans provide further detail. Treatment depends on stone location but may involve gland massage, duct incision or excision, or endoscopic stone removal procedures.Parotid gland swelling



Parotid gland swellingsakshat Lamichhane
╠²
Introduction
Approach to Parotid gland enlargement
Parotid gland swelling classification
Sj├ČgrenŌĆÖs Syndrome
WarthinŌĆÖs Tumor
Pleomorphic adenoma
Mucoepidermoid carcinoma
Sialadenitis
Sialolithiasis
Conclusion
Ameloblastoma



AmeloblastomaManjari Reshikesh
╠²
1) Ameloblastoma is a benign, locally invasive odontogenic tumor of enamel organ-type tissue that is the second most common odontogenic tumor.
2) It typically presents as a painless swelling in the mandible and is classified based on histological and clinical features into subtypes including follicular, plexiform, unicystic, and peripheral ameloblastoma.
3) Treatment involves surgical resection such as segmental resection for large tumors due to the high recurrence risk with more conservative treatments like curettage or enucleation.lichen planus and lichenoid reaction 4 .ppt



lichen planus and lichenoid reaction 4 .pptmadhusudhan reddy
╠²
Oral Lichen Planus is a common chronic inflammatory disease that affects the oral mucosa. It is characterized by T-cell mediated apoptosis of epithelial cells that leads to inflammation. The cause is unknown but believed to be autoimmune in nature. It presents as white reticulated lesions that can be reticular, papular, plaque-like, atrophic, erosive, bullous or ulcerative. Histopathology shows saw-tooth rete pegs and Civatte bodies. Direct immunofluorescence demonstrates a fibrin band in the basement membrane. The erosive form has a risk of malignant transformation. Treatment involves topical corticosteroids and immunosuppressants to reduce symptoms of pain and inflammation.Ludwig's angina



Ludwig's anginaAnwaaar
╠²
Ludwig's angina is a severe bacterial infection that involves the submandibular, sublingual, and submental spaces of the neck. It causes swelling in these areas bilaterally and can potentially lead to airway obstruction. The infection is usually caused by both aerobic and anaerobic bacteria spreading from an odontogenic source such as a dental abscess. Treatment involves aggressive antibiotic therapy, incision and drainage of the swollen areas, and airway management to prevent respiratory distress. Without proper treatment, Ludwig's angina can cause complications such as sepsis, mediastinitis, or even death from asphyxiation within 12 to 24 hours.Osteomyelitis of jaw



Osteomyelitis of jawSapeedeh Afzal
╠²
This document discusses osteomyelitis, including its pathogenesis and management. It defines osteomyelitis as an infection of the bone marrow and describes how local and systemic predisposing factors can lead to decreased bone vitality and impaired host defense. The main types of osteomyelitis covered are suppurative, focal sclerosing, diffuse sclerosing, and proliferative perositis. For each type, the document discusses pathogenesis, clinical features, histology, radiology, and management. Key points include how acute suppurative osteomyelitis can progress to chronic form if inadequately treated, and how eliminating infection sources is important but bone changes may persist radiographically for some types.Peripheral giant cell granuloma (giant cell epulis



Peripheral giant cell granuloma (giant cell epulisKhin Soe
╠²
The document discusses two types of giant cell lesions of the jaw: peripheral giant cell granuloma (PGG) and central giant cell granuloma (CGG). PGG is a reactive lesion caused by local irritation or trauma that occurs on the gingiva. CGG is a benign process that occurs within the jaw bones and can be non-aggressive or aggressive depending on symptoms and growth rate. Both lesions contain multinucleated giant cells and are treated with surgical excision, with CGG having a slightly higher recurrence rate. Key distinguishing features and histological characteristics are provided.Pleomorphic adenoma



Pleomorphic adenomaAishwarya Gopal
╠²
Pleomorphic adenoma is the most common benign tumor of the parotid gland. It consists of both epithelial cells and spindle-shaped mesenchymal cells within an abundant mucoid matrix. On pathology, it displays well-differentiated epithelial cells and spindle/stellate cells in a pleomorphic stroma with mucoid material. The tumor presents as a slow-growing, painless swelling of the parotid gland and is diagnosed by FNAC. The treatment is complete surgical excision via superficial parotidectomy while preserving the facial nerve. Recurrence is possible if there are pseudopods left behind or inadequate margins. Malignant transformation may occur in long-standing tumors.Cervical mases DDx and Radio-imaging by B.H.A.A Malik



Cervical mases DDx and Radio-imaging by B.H.A.A Malikbushra a malik
╠²
1. Cystic hygromas are fluid-filled sacs that result from a blockage in the lymphatic system and present as single or multiple cysts in the neck region. They can be congenital or develop later in life.
2. Cervical masses can have many potential causes, including infections, tumors, cysts, or abscesses arising from structures in the neck like lymph nodes, salivary glands, bones, or blood vessels. Imaging plays an important role in characterizing neck masses and determining their origin.
3. CT and ultrasound are useful in evaluating neck masses. Features like size, borders, internal architecture, and effects on surrounding tissues help differentiate benign from malignant causeslymphangitis.ppt



lymphangitis.pptLakshmi Murthy
╠²
This document discusses lymphangitis and lymphadenitis. Lymphangitis is defined as inflammation of the lymphatic channels that occurs as a result of infection at a site distal to the channel. Common causes include streptococcal bacteria. Symptoms include red streaks on the skin extending from the infection site toward lymph nodes. Treatment involves antibiotics. Lymphadenitis is inflammation of lymph nodes, which can be caused by various bacteria, viruses, fungi or other pathogens. Evaluation may involve imaging and biopsy to determine the cause and guide treatment.More Related Content
What's hot (20)
Ameloblastoma



Ameloblastomasakshat Lamichhane
╠²
Benign, locally aggressive tumor of odontogenic epithelium, Previously called adamantinoma, Second most common odontogenic tumor after odontoma, Mandible is most common site, Usually asymptomatic and can be found incidentally on routine dental examinationsCarcinoma tongue



Carcinoma tongueViswa Kumar
╠²
This document discusses the anatomy, etiology, clinical presentation, staging, and treatment options for carcinoma of the tongue. It notes that carcinoma of the tongue most commonly presents as a non-healing ulcer and can cause symptoms like otalgia, odynophagia, and bleeding. Treatment depends on staging and may involve surgery, radiation therapy, chemotherapy, or a combination. Prognosis decreases with more advanced stage at diagnosis.Diseases of-salivary-glands 



Diseases of-salivary-glands Weam Faroun
╠²
This document discusses diseases of the salivary glands, including sialadenitis (inflammation of the salivary glands), which can be caused by bacterial or viral infections. It also discusses Sjogren's syndrome, an autoimmune disease that causes dry mouth and dry eyes due to lymphocytic infiltration and destruction of the lacrimal and salivary glands. Obstructive diseases like salivary calculi (stones) are also covered. The document provides details on symptoms, diagnosis, and treatment of various salivary gland diseases.Odontogenic tumors ppt



Odontogenic tumors pptmadhusudhan reddy
╠²
This document discusses different types of odontogenic tumors. It classifies them into three categories: tumors of odontogenic epithelium, mixed odontogenic tumors, and tumors of odontogenic ectomesenchyme. Key tumors discussed include ameloblastoma, adenomatoid odontogenic tumor (AOT), and calcifying epithelial odontogenic tumor (CEOT). Ameloblastoma is the most common odontogenic tumor and can be solid/multicystic, unicystic, or peripheral. AOT typically occurs in younger females in the anterior maxilla. CEOT accounts for less than 1% of odontogenic tumors and resembles cells of the enamel organ or dental lamina.Oral cavity lesions



Oral cavity lesionsNotre Dame De Chartres Hospital
╠²
This document discusses various lesions that can occur in the oral cavity. It begins by defining mouth ulcers and listing common causes such as physical abrasion, infection, and cancer. It then covers specific conditions like recurrent aphthous stomatitis, lichen planus, pemphigus vulgaris, and necrotizing sialometaplasia. It provides details on symptoms, appearance, epidemiology, treatment and pathogenesis for each condition. In general, the document provides a comprehensive overview of acute and chronic ulcerative lesions that can present in the oral cavity.Weber ferguson incison (poster)



Weber ferguson incison (poster)Sk Aziz Ikbal
╠²
The Weber-Fergusson incision is indicated for access to tumors involving the maxilla extending superiorly to the infraorbital nerve and into or involving the orbit. It provides wide access to all areas of the maxilla. The incision line is drawn through the vermillion border along the filtrum of the lip, extending around the base of the nose along the facial nasal groove. It then extends infraorbitally below the cilium to the lateral canthus. Tarsorrhaphy sutures are placed in the eyelid. The incision is made through the skin and subcutaneous tissue along the nose, and the full thickness upper lip is transsected with ligation of the labial arteryTumor of oral cavity



Tumor of oral cavityshekhar star
╠²
The document discusses tumors and neoplasms of the oral cavity. It defines a tumor as a swelling of tissue, while neoplasia is an abnormal mass of tissue that exceeds normal growth. For simplicity, tumors and neoplasms are used interchangeably. Tumors of the oral cavity are classified based on their tissue of origin into epithelial, connective, muscle, nerve or metastatic tumors. Benign epithelial tumors include squamous papilloma and keratoacanthoma. Squamous papilloma presents as a painless, cauliflower-like growth caused by HPV infection, while keratoacanthoma is a potentially malignant growth associated with sun exposure. Both lesions can be surgically excised with low recurrence ratesOral malignancy



Oral malignancySaleh Bakry
╠²
This document discusses the clinical diagnosis and evaluation of oral malignancy. It covers:
- Performing a thorough clinical examination of the oral cavity and lymph nodes to check for abnormalities.
- Taking a detailed patient history regarding the lesion.
- Using radiographic imaging like x-rays and MRI to examine intraoral lesions and bone involvement.
- Conducting lab tests and biopsy of suspicious areas to confirm a diagnosis of oral cancer.
- Classifying oral cancers based on location, pathology, and extent of spread to aid in staging and treatment planning.Tumors of salivary gland



Tumors of salivary glandazfarneyaz
╠²
This document provides information on various types of salivary gland tumors. It begins with an overview of the major and minor salivary gland tumors that are most commonly seen in adults and children. Examples include Warthin tumor, acinic cell carcinoma, and polymorphous low-grade adenocarcinoma. The document then describes the histological features of many benign and malignant epithelial and nonepithelial salivary gland tumors at both the macroscopic and microscopic levels. Key diagnostic characteristics of tumors like pleomorphic adenoma, myoepithelioma, oncocytoma, and adenoid cystic carcinoma are highlighted.Parotidectomy



ParotidectomyPrashanth Lakshman
╠²
This document provides information about parotidectomy, which is the surgical removal of the parotid gland. It discusses the different types of parotidectomy including superficial and total parotidectomy. Superficial parotidectomy involves removing the superficial lobe of the parotid gland while preserving the facial nerve. The procedure is described in detail, including identifying landmarks to locate the facial nerve and carefully dissecting the gland superficial to the nerve. Complications involving the facial nerve are also addressed.Salivary glands diseases



Salivary glands diseasesIAU Dent
╠²
This document provides information on salivary gland diseases presented over multiple sessions. It begins with the objectives and overview of topics to be covered, including applied anatomy of the salivary glands, autonomic innervation and effects on function, inflammatory and obstructive disorders, neoplasms, and investigations. It then describes in detail the anatomy, physiology and investigations of the major salivary glands. Salivary gland diseases are classified as functional, obstructive, non-neoplastic and neoplastic. Specific conditions like sialadenitis, sialolithiasis, mucocele and ranula are explained. Imaging modalities like ultrasound, sialography, CT, MRI and sialendoscopyAetiology and management of trismus



Aetiology and management of trismusHope Inegbenosun
╠²
This document outlines the etiology and management of trismus. It defines trismus as restricted mouth opening and describes normal ranges of opening. Common causes of trismus include infections, trauma, surgery, tumors, radiation, TMJ disorders, and drugs. Management involves thorough history and examination, investigations to diagnose the underlying cause, and various treatment approaches depending on the etiology such as heat therapy, medical management, physiotherapy, surgery, and appliances.Sialolithiasis



SialolithiasisRuchi Rathi
╠²
Sialolithiasis refers to the formation of calcific stones within the salivary glands or ducts. The submandibular gland is most commonly affected. Clinical features include intermittent pain and swelling near the affected gland during or after meals. Investigations like radiography can detect radiopaque stones, while sialography or CT scans provide further detail. Treatment depends on stone location but may involve gland massage, duct incision or excision, or endoscopic stone removal procedures.Parotid gland swelling



Parotid gland swellingsakshat Lamichhane
╠²
Introduction
Approach to Parotid gland enlargement
Parotid gland swelling classification
Sj├ČgrenŌĆÖs Syndrome
WarthinŌĆÖs Tumor
Pleomorphic adenoma
Mucoepidermoid carcinoma
Sialadenitis
Sialolithiasis
Conclusion
Ameloblastoma



AmeloblastomaManjari Reshikesh
╠²
1) Ameloblastoma is a benign, locally invasive odontogenic tumor of enamel organ-type tissue that is the second most common odontogenic tumor.
2) It typically presents as a painless swelling in the mandible and is classified based on histological and clinical features into subtypes including follicular, plexiform, unicystic, and peripheral ameloblastoma.
3) Treatment involves surgical resection such as segmental resection for large tumors due to the high recurrence risk with more conservative treatments like curettage or enucleation.lichen planus and lichenoid reaction 4 .ppt



lichen planus and lichenoid reaction 4 .pptmadhusudhan reddy
╠²
Oral Lichen Planus is a common chronic inflammatory disease that affects the oral mucosa. It is characterized by T-cell mediated apoptosis of epithelial cells that leads to inflammation. The cause is unknown but believed to be autoimmune in nature. It presents as white reticulated lesions that can be reticular, papular, plaque-like, atrophic, erosive, bullous or ulcerative. Histopathology shows saw-tooth rete pegs and Civatte bodies. Direct immunofluorescence demonstrates a fibrin band in the basement membrane. The erosive form has a risk of malignant transformation. Treatment involves topical corticosteroids and immunosuppressants to reduce symptoms of pain and inflammation.Ludwig's angina



Ludwig's anginaAnwaaar
╠²
Ludwig's angina is a severe bacterial infection that involves the submandibular, sublingual, and submental spaces of the neck. It causes swelling in these areas bilaterally and can potentially lead to airway obstruction. The infection is usually caused by both aerobic and anaerobic bacteria spreading from an odontogenic source such as a dental abscess. Treatment involves aggressive antibiotic therapy, incision and drainage of the swollen areas, and airway management to prevent respiratory distress. Without proper treatment, Ludwig's angina can cause complications such as sepsis, mediastinitis, or even death from asphyxiation within 12 to 24 hours.Osteomyelitis of jaw



Osteomyelitis of jawSapeedeh Afzal
╠²
This document discusses osteomyelitis, including its pathogenesis and management. It defines osteomyelitis as an infection of the bone marrow and describes how local and systemic predisposing factors can lead to decreased bone vitality and impaired host defense. The main types of osteomyelitis covered are suppurative, focal sclerosing, diffuse sclerosing, and proliferative perositis. For each type, the document discusses pathogenesis, clinical features, histology, radiology, and management. Key points include how acute suppurative osteomyelitis can progress to chronic form if inadequately treated, and how eliminating infection sources is important but bone changes may persist radiographically for some types.Peripheral giant cell granuloma (giant cell epulis



Peripheral giant cell granuloma (giant cell epulisKhin Soe
╠²
The document discusses two types of giant cell lesions of the jaw: peripheral giant cell granuloma (PGG) and central giant cell granuloma (CGG). PGG is a reactive lesion caused by local irritation or trauma that occurs on the gingiva. CGG is a benign process that occurs within the jaw bones and can be non-aggressive or aggressive depending on symptoms and growth rate. Both lesions contain multinucleated giant cells and are treated with surgical excision, with CGG having a slightly higher recurrence rate. Key distinguishing features and histological characteristics are provided.Pleomorphic adenoma



Pleomorphic adenomaAishwarya Gopal
╠²
Pleomorphic adenoma is the most common benign tumor of the parotid gland. It consists of both epithelial cells and spindle-shaped mesenchymal cells within an abundant mucoid matrix. On pathology, it displays well-differentiated epithelial cells and spindle/stellate cells in a pleomorphic stroma with mucoid material. The tumor presents as a slow-growing, painless swelling of the parotid gland and is diagnosed by FNAC. The treatment is complete surgical excision via superficial parotidectomy while preserving the facial nerve. Recurrence is possible if there are pseudopods left behind or inadequate margins. Malignant transformation may occur in long-standing tumors.Similar to Cervical Lymphadenopathy (20)
Cervical mases DDx and Radio-imaging by B.H.A.A Malik



Cervical mases DDx and Radio-imaging by B.H.A.A Malikbushra a malik
╠²
1. Cystic hygromas are fluid-filled sacs that result from a blockage in the lymphatic system and present as single or multiple cysts in the neck region. They can be congenital or develop later in life.
2. Cervical masses can have many potential causes, including infections, tumors, cysts, or abscesses arising from structures in the neck like lymph nodes, salivary glands, bones, or blood vessels. Imaging plays an important role in characterizing neck masses and determining their origin.
3. CT and ultrasound are useful in evaluating neck masses. Features like size, borders, internal architecture, and effects on surrounding tissues help differentiate benign from malignant causeslymphangitis.ppt



lymphangitis.pptLakshmi Murthy
╠²
This document discusses lymphangitis and lymphadenitis. Lymphangitis is defined as inflammation of the lymphatic channels that occurs as a result of infection at a site distal to the channel. Common causes include streptococcal bacteria. Symptoms include red streaks on the skin extending from the infection site toward lymph nodes. Treatment involves antibiotics. Lymphadenitis is inflammation of lymph nodes, which can be caused by various bacteria, viruses, fungi or other pathogens. Evaluation may involve imaging and biopsy to determine the cause and guide treatment.Common neck swellings 



Common neck swellings OmarAlaidaroos3
╠²
This document discusses common neck swellings, including their anatomy, clinical presentations, investigations, and management. The main points are:
1. Neck lumps in children are rarely malignant, while adults with lateral neck lumps should be investigated to exclude cancer.
2. The neck is divided into anterior and posterior triangles bounded by muscles and bones. Lymph nodes are grouped into levels.
3. Common neck swellings include infected lymph nodes, cysts, tumors, and abscesses. Investigations include physical exam, imaging like CT/MRI, and biopsy. Management depends on diagnosis and may include antibiotics, surgery, or other treatments.Congenital anomalies of larynx



Congenital anomalies of larynxSanjay Maharjan
╠²
This document discusses various congenital anomalies of the larynx that can occur due to errors in embryogenesis. It begins with an overview of laryngeal development from the 4th to 6th week of gestation. It then describes several supraglottic anomalies such as laryngomalacia, laryngeal or saccular cysts, and lymphangiomas. Glottic anomalies discussed include laryngeal webs, atresia, and vocal cord paralysis. Subglottic anomalies like congenital subglottic stenosis and subglottic hemangiomas are also covered. The document concludes with descriptions of genetic and central nervous system anomalies that can involve the larynx, such as Cri du Chat syndrome andPapillary lesions



Papillary lesionsIAU Dent
╠²
The document discusses various verrucal-papillary lesions of the oral cavity including reactive lesions such as papillary hyperplasia, condyloma latum, squamous papilloma, condyloma acuminatum, and focal epithelial hyperplasia. It also discusses neoplasms like keratoacanthoma and verrucous carcinoma. Rare lesions of unknown etiology discussed include pyostomatitis vegetans and verruciform xanthoma. Each lesion is described in terms of etiology, clinical features, histopathology, differential diagnosis, and treatment.meningococci-190124192447ueueueuejj.pptx



meningococci-190124192447ueueueuejj.pptxsandysingh8112002
╠²
Neisseria meningitidis is a gram-negative bacterium that can cause meningitis and meningococcemia. It is transmitted through respiratory droplets and colonizes the nasopharynx. The highest rates occur in sub-Saharan Africa, known as the meningitis belt. Diagnosis involves examining CSF, blood, or nasopharyngeal samples by microscopy, culture, or PCR. Treatment involves immediate hospitalization and intravenous antibiotics such as ceftriaxone. Vaccines are available to help prevent disease.Clinical approach fever +lymphadenopathy



Clinical approach fever +lymphadenopathyWalaa Manaa
╠²
This document provides an overview of lymphadenopathy in children, including its anatomy, pathophysiology, causes, and management approaches. It distinguishes between generalized and regional lymphadenopathy. Common causes of generalized lymphadenopathy include viral infections like mononucleosis, while regional lymphadenopathy is often due to infections in the local drainage area. Evaluation involves considering infectious, inflammatory, and malignant etiologies based on presentation. Management depends on the identified cause but typically involves supportive care or antibiotics for infections.Child with lymphadenopathy



Child with lymphadenopathyNurzawani Shamsudin
╠²
This document discusses the approach to a child presenting with lymphadenopathy. It begins with an introduction to lymph node anatomy and pathophysiology. It then discusses the differential diagnosis and key features of generalized versus regional lymphadenopathy. Specific infectious, inflammatory and malignant conditions that can cause lymphadenopathy are outlined. The summary concludes with guidance on taking a thorough history to identify potential causes and guide appropriate investigations.Surgical site infection



Surgical site infectionMasrur Akbar Khan
╠²
This document discusses various surgical site infections including:
1. Boils, carbuncles, and hidradenitis suppurativa which are infections of hair follicles and sweat glands caused by bacteria like Staphylococcus aureus. Treatment involves antibiotics and drainage.
2. Impetigo, a contagious skin infection in children caused by Staphylococcus or Streptococcus that forms blisters and crusts. It is treated with oral antibiotics and topical antiseptics.
3. Septicemia and pyemia, serious bloodstream infections that can lead to organ dysfunction or failure. Gram-positive infections commonly originate from the skin while gram-negative infections often start inSalivary gland pathology



Salivary gland pathologySaleh Alorainy
╠²
This document discusses salivary gland pathology. It begins with the anatomy and histology of the major salivary glands. It then covers the physiology of salivary secretion and neural regulation. Specific conditions are discussed like parotitis, submandibular gland stones, and salivary gland tumors. Parotitis includes mumps infection which causes inflammation of the parotid glands. Submandibular gland stones form in the salivary ducts. Benign tumors are most common, with pleomorphic adenoma being the most frequent. Malignant tumors can also occur, such as mucoepidermoid carcinoma and adenoid cystic carcinoma.Rectal diseases



Rectal diseasesakshaykumar choragi
╠²
This document discusses various rectal diseases including prolapse, proctitis, polyps, benign lesions, and carcinoma. Rectal prolapse is classified as mucosal or full-thickness and can be caused by straining, weak pelvic floor muscles, or trauma from childbirth. Treatment depends on the type but may include injections, banding, or surgery. Proctitis is inflammation that can be caused by infection, radiation, or inflammatory bowel disease. Polyps are growths that can be removed endoscopically if small or via surgery if large. Benign lesions include endometriosis, hemangiomas, and neuroendocrine tumors. Rectal carcinoma is often treated with surgery such as anterior resection or6. diseases of the external ear



6. diseases of the external earkrishnakoirala4
╠²
Diseases of the external ear can be congenital, traumatic, inflammatory, or neoplastic in nature. Common inflammatory conditions include otitis externa, perichondritis, and keratosis obturans. Otitis externa may be localized like furunculosis or diffuse. Malignant otitis externa is a severe infection that can spread to the skull base. Preauricular sinus and hematoma of the pinna are examples of traumatic external ear diseases. Treatment involves cleaning, topical or oral antibiotics, incision and drainage of abscesses, and sometimes surgery. Recurrence is possible with some conditions.Diseases of the external ear



Diseases of the external earDr Krishna Koirala
╠²
1.Congenital
Minor : Accessory auricular tags , Bat ear Pre - auricular sinus
Major : Anotia ,Microtia
3. Traumatic
Hematoma , lacerations
Inflammatory : Perichondritis
4. Neoplastic : Squamous cell carcinoma
Basal cell carcinoma
5. Others : Sebaceous cyst ,lipoma , keloids, Pseudocyst pinna
benign neck disease [Autosaved].pptx orlhns![benign neck disease [Autosaved].pptx orlhns](https://cdn.slidesharecdn.com/ss_thumbnails/benignneckdiseaseautosaved-241117151930-f0f5c123-thumbnail.jpg?width=560&fit=bounds)
![benign neck disease [Autosaved].pptx orlhns](https://cdn.slidesharecdn.com/ss_thumbnails/benignneckdiseaseautosaved-241117151930-f0f5c123-thumbnail.jpg?width=560&fit=bounds)
![benign neck disease [Autosaved].pptx orlhns](https://cdn.slidesharecdn.com/ss_thumbnails/benignneckdiseaseautosaved-241117151930-f0f5c123-thumbnail.jpg?width=560&fit=bounds)
![benign neck disease [Autosaved].pptx orlhns](https://cdn.slidesharecdn.com/ss_thumbnails/benignneckdiseaseautosaved-241117151930-f0f5c123-thumbnail.jpg?width=560&fit=bounds)
benign neck disease [Autosaved].pptx orlhnsadhikariparitosh09
╠²
basic approach to benign neck diseases congenital , inflammatory and least common disease Otitis externa



Otitis externaAhmed Almumtin
╠²
Otitis externa refers to infections of the external ear canal. It can be acute or chronic. Acute otitis externa is commonly known as swimmer's ear and is caused by bacterial or fungal infections due to water exposure. Chronic otitis externa is defined as lasting over 4 weeks and is often due to bacterial, fungal, or dermatological causes. Necrotizing external otitis is a potentially lethal infection seen in immunocompromised patients like diabetics. Treatment involves topical or oral antibiotics, cleaning of the ear canal, and surgery in severe cases. Proper diagnosis depends on history, exam, and sometimes imaging or labs.Hypopharyngeal carcinoma



Hypopharyngeal carcinomaTabeer Arif
╠²
This document provides an overview of hypopharyngeal carcinoma, including its anatomy, epidemiology, etiology, presentation, investigations, treatment options, and complications. Hypopharyngeal carcinoma most commonly arises in the piriform fossa and affects males over age 60, with risk factors including alcohol, smoking, and irradiation. Presenting symptoms include dysphagia, sore throat, and neck mass. Treatment depends on staging and may include surgical excision, chemoradiotherapy, or radiotherapy alone. Complications can include bleeding, tracheal damage, leakage, and swallowing difficulties.Surgical options for different Pleural Diseases



Surgical options for different Pleural DiseasesIrfanNashad1
╠²
This document discusses various pleural diseases including pleural effusion, empyema, and chylothorax. It begins by defining the pleura and pleural space. For pleural effusion, it describes the types (hydrothorax, haemothorax, pyothorax), causes, signs and symptoms, investigations including thoracentesis, and treatments including drainage, pleurodesis, and surgery. For empyema, it covers definition, causes, pathogenesis, complications, investigations and criteria for diagnosis, and treatments including antibiotics, drainage, decortication, and thoracoplasty. For chylothorax, it defines it as chyle in the pleural space due to thoracicDiseases of the External Ear.ppt



Diseases of the External Ear.pptDrKrishnaKoiralaENT
╠²
Diseases of the external ear are common conditions to be encountered in ENT practice. This presentation is about the major conditions of pinna and EAC including pinna defects, pseudocyst of pinna, perichondritis, hematoma, pseudocyst of pinna, otitis externa, otomycosis, malignant otitis externa, keratosis obturans etc. Meningococci



MeningococciArun Geetha Viswanathan
╠²
Meningococci are a type of bacteria that cause serious infections. The most common infection is meningitis, which is an inflammation of the thin tissue that surrounds the brain and spinal cord. Meningococci can also cause other problems, including a serious bloodstream infection called sepsis. In its early stages, you may have flu-like symptoms and a stiff neck. But the disease can progress quickly and can be fatal. Early diagnosis and treatment are extremely important. Lab tests on your blood and cerebrospinal fluid can tell if you have it. Treatment is with antibiotics. Since the infection spreads from person to person, family members may also need to be treated.
A vaccine can prevent meningococcal infections.Recently uploaded (20)
Flag Screening in Physiotherapy Examination.pptx



Flag Screening in Physiotherapy Examination.pptxBALAJI SOMA
╠²
Flag screening is a crucial part of physiotherapy assessment that helps in identifying medical, psychological, occupational, and social barriers to recovery. Recognizing these flags ensures that physiotherapists make informed decisions, provide holistic care, and refer patients appropriately when necessary. By integrating flag screening into practice, physiotherapists can optimize patient outcomes and prevent chronicity of conditions.Presentaci├│ "Projecte Benestar". MWC 2025



Presentaci├│ "Projecte Benestar". MWC 2025Badalona Serveis Assistencials
╠²
Presentaci├│ que va acompanyar la demostraci├│ pr├Āctica de metge d'Innovaci├│ Jos├® Ferrer sobre el projecte Benestar de BSA, nom d'IDIAP Pere Gol, el 5 de mar├¦ de 2025 a l'estand de XarSMART al Mobible Word Congress. Regulation of tubular reabsorption _AntiCopy.pdf



Regulation of tubular reabsorption _AntiCopy.pdfMedicoseAcademics
╠²
Title: Regulation of Tubular Reabsorption ŌĆō A Comprehensive Overview
Description:
This lecture provides a detailed and structured explanation of the mechanisms regulating tubular reabsorption in the kidneys. It explores how different physiological and hormonal factors influence glomerular filtration and reabsorption rates, ensuring fluid and electrolyte balance in the body.
¤öŹ Who Should Read This?
This presentation is designed for:
Ō£ö’ĖÅ Medical Students (MBBS, BDS, Nursing, Allied Health Sciences) preparing for physiology exams.
Ō£ö’ĖÅ Medical Educators & Professors looking for structured teaching material.
Ō£ö’ĖÅ Healthcare Professionals (doctors, nephrologists, and physiologists) seeking a refresher on renal physiology.
Ō£ö’ĖÅ Postgraduate Students & Researchers in the field of medical sciences and physiology.
¤ōī What YouŌĆÖll Learn:
Ō£ģ Local Regulation of Tubular Reabsorption
Ō£ö’ĖÅ Glomerulo-Tubular Balance ŌĆō its mechanism and clinical significance
Ō£ö’ĖÅ Net reabsorptive forces affecting peritubular capillaries
Ō£ö’ĖÅ Role of peritubular hydrostatic and colloid osmotic pressures
Ō£ģ Hormonal Regulation of Tubular Reabsorption
Ō£ö’ĖÅ Effects of Aldosterone, Angiotensin II, ADH, and Natriuretic Peptides
Ō£ö’ĖÅ Clinical conditions like AddisonŌĆÖs disease & Conn Syndrome
Ō£ö’ĖÅ Mechanisms of pressure natriuresis and diuresis
Ō£ģ Nervous System Regulation
Ō£ö’ĖÅ Sympathetic Nervous System activation and its effects on sodium reabsorption
¤®║ Clinical Correlations & Case Discussions
Ō£ö’ĖÅ How renal regulation is altered in hypertension, hypotension, and proteinuria
Ō£ö’ĖÅ Comparison of Glomerulo-Tubular Balance vs. Tubulo-Glomerular Feedback
This presentation provides detailed diagrams, flowcharts, and calculations to enhance understanding and retention. Whether you are studying, teaching, or practicing medicine, this lecture will serve as a valuable resource for mastering renal physiology.
¤ōó Keywords for Easy Search:
#Physiology #RenalPhysiology #TubularReabsorption #GlomeruloTubularBalance #HormonalRegulation #MedicalEducation #NephrologyRenal Physiology - Regulation of GFR and RBF



Renal Physiology - Regulation of GFR and RBFMedicoseAcademics
╠²
1. Explain the physiological control of glomerular filtration and renal blood flow
2. Describe the humoral and autoregulatory feedback mechanisms that mediate the autoregulation of renal plasma flow and glomerular filtration rate
MLS 208 - UNIT 4 A - Tissue Processing - ETANDO AYUK - SANU 1 - Secured.pdf



MLS 208 - UNIT 4 A - Tissue Processing - ETANDO AYUK - SANU 1 - Secured.pdfEswatini Medical Christian University - EMCU / Southern Nazarene University - SANU
╠²
The course covers the steps undertaken from tissue collection, reception, fixation,
sectioning, tissue processing and staining. It covers all the general and special
techniques in histo/cytology laboratory. This course will provide the student with the
basic knowledge of the theory and practical aspect in the diagnosis of tumour cells
and non-malignant conditions in body tissues and for cytology focusing on
gynaecological and non-gynaecological samples.Macafem Reviews 2024 - Macafem for Menopause Symptoms



Macafem Reviews 2024 - Macafem for Menopause SymptomsMacafem Supplement
╠²
At Macafem, we provide 100% natural support for women navigating menopause. For over 20 years, we've helped women manage symptoms, and in 2024, we're proud to share their heartfelt experiences.Best Sampling Practices Webinar ŌĆō USP <797> Compliance & Environmental Monito...



Best Sampling Practices Webinar ŌĆō USP <797> Compliance & Environmental Monito...NuAire
╠²
Best Sampling Practices Webinar ŌĆō USP <797> Compliance & Environmental Monitoring
Are your cleanroom sampling practices USP <797> compliant? This webinar, hosted by Pharmacy Purchasing & Products (PP&P Magazine) and sponsored by NuAire, features microbiology expert Abby Roth discussing best practices for surface & air sampling, data analysis, and compliance.
¤ÆĪ Key Topics Covered:
Ō£ö’ĖÅ Viable air & surface sampling best practices
Ō£ö’ĖÅ USP <797> requirements & compliance strategies
Ō£ö’ĖÅ How to analyze & trend viable sample data
Ō£ö’ĖÅ Improving environmental monitoring in cleanrooms
¤Äź Watch Now: https://www.nuaire.com/resources/best-sampling-practices-cleanroom-usp-797
¤ōó Stay informedŌĆöfollow Abby Roth on LinkedIn for more cleanroom insights!Stability of Dosage Forms as per ICH Guidelines



Stability of Dosage Forms as per ICH GuidelinesKHUSHAL CHAVAN
╠²
This presentation covers the stability testing of pharmaceutical dosage forms according to ICH guidelines (Q1A-Q1F). It explains the definition of stability, various testing protocols, storage conditions, and evaluation criteria required for regulatory submissions. Key topics include stress testing, container closure systems, stability commitment, and photostability testing. The guidelines ensure that pharmaceutical products maintain their identity, purity, strength, and efficacy throughout their shelf life. This resource is valuable for pharmaceutical professionals, researchers, and regulatory experts.Multimodal Approaches to Clitoral Augmentation for FGM (PRP _ filler)"



Multimodal Approaches to Clitoral Augmentation for FGM (PRP _ filler)"Rehab Aboshama
╠²
Multimodal Approaches to Clitoral Augmentation for FGM (PRP _ filler)"
Biography of Dr. Vincenzo Giordano



Biography of Dr. Vincenzo GiordanoDr. Vincenzo Giordano
╠²
Dr. Vincenzo Giordano began his medical career 2011 at Aberdeen Royal Infirmary in the Department of Cardiothoracic Surgery. Here, he performed complex adult cardiothoracic surgical procedures, significantly enhancing his proficiency in patient critical care, as evidenced by his FCCS certification.Acute & Chronic Inflammation, Chemical mediators in Inflammation and Wound he...



Acute & Chronic Inflammation, Chemical mediators in Inflammation and Wound he...Ganapathi Vankudoth
╠²
A complete information of Inflammation, it includes types of Inflammation, purpose of Inflammation, pathogenesis of acute inflammation, chemical mediators in inflammation, types of chronic inflammation, wound healing and Inflammation in skin repair, phases of wound healing, factors influencing wound healing and types of wound healing.MORPHOLOGICAL FEATURES OF PNEUMONIA.....



MORPHOLOGICAL FEATURES OF PNEUMONIA.....maheenmazhar021
╠²
This presentation provides a detailed exploration of the morphological and microscopic features of pneumonia, covering its histopathology, classification, and clinical significance. Designed for medical students, pathologists, and healthcare professionals, this lecture differentiates bacterial vs. viral pneumonia, explains lobar, bronchopneumonia, and interstitial pneumonia, and discusses diagnostic imaging patterns.
¤ÆĪ Key Topics Covered:
Ō£ģ Normal lung histology vs. pneumonia-affected lung
Ō£ģ Morphological changes in lobar, bronchopneumonia, and interstitial pneumonia
Ō£ģ Microscopic features: Fibroblastic plugs, alveolar septal thickening, inflammatory cell infiltration
Ō£ģ Stages of lobar pneumonia: Congestion, Red hepatization, Gray hepatization, Resolution
Ō£ģ Common causative pathogens (Streptococcus pneumoniae, Klebsiella pneumoniae, Mycoplasma, etc.)
Ō£ģ Clinical case study with diagnostic approach and differentials
¤ö¼ Who Should Watch?
This is an essential resource for medical students, pathology trainees, and respiratory health professionals looking to enhance their understanding of pneumoniaŌĆÖs morphological aspects.PRODUCTION OF HB VACCINE AND INTERFERONS BY rDNA - Copy.pptx



PRODUCTION OF HB VACCINE AND INTERFERONS BY rDNA - Copy.pptxkarishmaduhijod1
╠²
APPLICATION of RECOMBINANAT DNA TECHNOLOGY : IN THE PRODUCTION OF HEPATITIS B VACCINE ,INSULIN and INTERFERONSAPIENT Medi-trivia Quiz (FINALS) | TRI-ORTA 2025



SAPIENT Medi-trivia Quiz (FINALS) | TRI-ORTA 2025Dr. Anindya
╠²
Final Round of SAPIENT Medi-trivia quiz
Part of TRI-ORTA 2025
Venue: GLT, Medical College Kolkata
Date: 25-02-2025Local Anesthetic Use in the Vulnerable Patients



Local Anesthetic Use in the Vulnerable PatientsReza Aminnejad
╠²
Local anesthetics are a cornerstone of pain management, but their use requires special consideration in vulnerable groups such as pediatric, elderly, diabetic, or obese patients. In this presentation, weŌĆÖll explore how factors like age and physiology influence local anesthetics' selection, dosing, and safety. By understanding these differences, we can optimize patient care and minimize risks.
physiology 1 T3T4 & Jaundice & capillary circulation ž│žżž¦┘ä.pptx



physiology 1 T3T4 & Jaundice & capillary circulation ž│žżž¦┘ä.pptxamralmohammady27
╠²
┘ä┘ł ž╣┘åž»┘ā ┘䞦ž© ž¬┘łž© žŻ┘ł ž¬ž¦ž©┘䞬 ┘üž¦┘ä
power point show
┘ć┘Ŗ┘å┘üž╣┘ā ž¼ž»ž¦ ┘ü┘Ŗ ┘ģž▒ž¦ž¼ž╣ž® ž│ž▒┘Ŗž╣ž® ┘ä┘Ŗ┘äž® ž¦┘䞦┘ģž¬žŁž¦┘å
┘łž¦┘ä┘ä┘Ŗ ┘Ŗ┘éž»ž▒ ┘Ŗž╣┘ģ┘ä žŁž¦ž¼ž® ┘Ŗž╣┘ģ┘ä┘枦
┘łž┤┘āž▒ž¦ ┘ä┘äž»┘āž¬┘łž▒ž® ┘å┘łž¦┘ä ž╣┘ä┘ē ž¬ž¼┘ģ┘Ŗž╣ž® žŻž│ž”┘äž® ž¦┘äž©┘Ŗ┘łMLS 208 - UNIT 4 A - Tissue Processing - ETANDO AYUK - SANU 1 - Secured.pdf



MLS 208 - UNIT 4 A - Tissue Processing - ETANDO AYUK - SANU 1 - Secured.pdfEswatini Medical Christian University - EMCU / Southern Nazarene University - SANU
╠²
Acute & Chronic Inflammation, Chemical mediators in Inflammation and Wound he...



Acute & Chronic Inflammation, Chemical mediators in Inflammation and Wound he...Ganapathi Vankudoth
╠²
Cervical Lymphadenopathy
- 1. Differential Diagnosis of Enlarged Cervical Lymph Nodes Apoorva Kottary 28 1
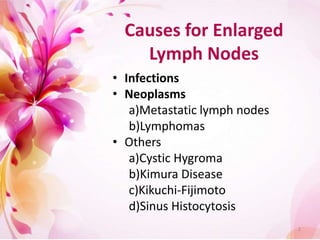
- 2. Causes for Enlarged Lymph Nodes ŌĆó Infections ŌĆó Neoplasms a)Metastatic lymph nodes b)Lymphomas ŌĆó Others a)Cystic Hygroma b)Kimura Disease c)Kikuchi-Fijimoto d)Sinus Histocytosis 2
- 3. 3
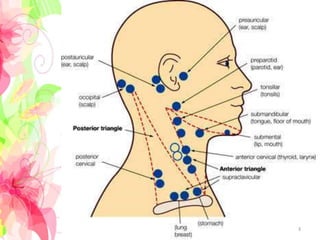
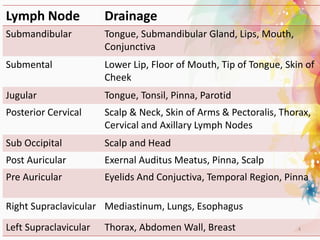
- 4. Lymph Node Drainage Submandibular Tongue, Submandibular Gland, Lips, Mouth, Conjunctiva Submental Lower Lip, Floor of Mouth, Tip of Tongue, Skin of Cheek Jugular Tongue, Tonsil, Pinna, Parotid Posterior Cervical Scalp & Neck, Skin of Arms & Pectoralis, Thorax, Cervical and Axillary Lymph Nodes Sub Occipital Scalp and Head Post Auricular Exernal Auditus Meatus, Pinna, Scalp Pre Auricular Eyelids And Conjuctiva, Temporal Region, Pinna Right Supraclavicular Mediastinum, Lungs, Esophagus Left Supraclavicular Thorax, Abdomen Wall, Breast 4
- 5. Infections ŌĆó Bacterial ŌĆō Coccal infections, Influenza, Tularemia, Typhoid ŌĆó Viral - HIV, Syphilis, Herpes, Hepatitis, Cat scratch Disease ŌĆó Parasitic ŌĆō Toxoplasmosis, Trypanosomiasis, Histoplasmosis, Leishmaniasis ŌĆó Mycobacterial - Tuberculosis 5
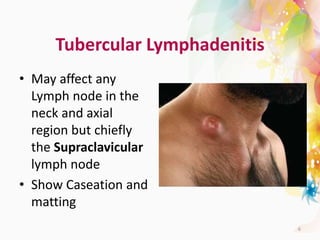
- 6. Tubercular Lymphadenitis ŌĆó May affect any Lymph node in the neck and axial region but chiefly the Supraclavicular lymph node ŌĆó Show Caseation and matting 6
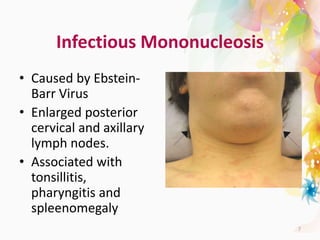
- 7. Infectious Mononucleosis ŌĆó Caused by Ebstein- Barr Virus ŌĆó Enlarged posterior cervical and axillary lymph nodes. ŌĆó Associated with tonsillitis, pharyngitis and spleenomegaly 7
- 8. Neoplastic Lesions ŌĆó Metastatic Lymph Nodes ŌĆó Lymphomas ŌĆó Kaposi Sarcoma ŌĆó Castleman disease 8
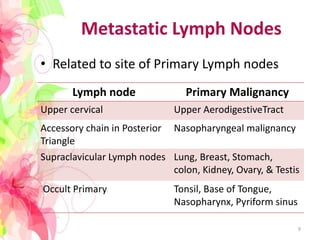
- 9. Metastatic Lymph Nodes ŌĆó Related to site of Primary Lymph nodes Lymph node Primary Malignancy Upper cervical Upper AerodigestiveTract Accessory chain in Posterior Triangle Nasopharyngeal malignancy Supraclavicular Lymph nodes Lung, Breast, Stomach, colon, Kidney, Ovary, & Testis Occult Primary Tonsil, Base of Tongue, Nasopharynx, Pyriform sinus 9
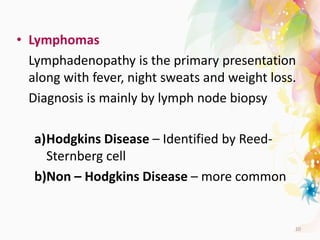
- 10. ŌĆó Lymphomas Lymphadenopathy is the primary presentation along with fever, night sweats and weight loss. Diagnosis is mainly by lymph node biopsy a)Hodgkins Disease ŌĆō Identified by Reed- Sternberg cell b)Non ŌĆō Hodgkins Disease ŌĆō more common 10
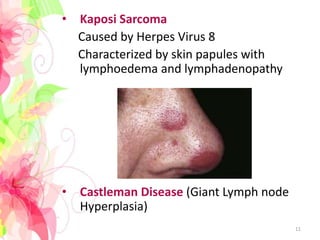
- 11. ŌĆó Kaposi Sarcoma Caused by Herpes Virus 8 Characterized by skin papules with lymphoedema and lymphadenopathy ŌĆó Castleman Disease (Giant Lymph node Hyperplasia) 11
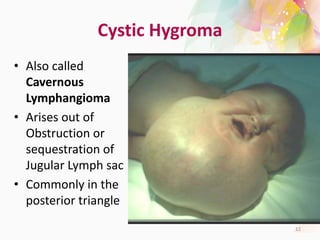
- 12. Cystic Hygroma ŌĆó Also called Cavernous Lymphangioma ŌĆó Arises out of Obstruction or sequestration of Jugular Lymph sac ŌĆó Commonly in the posterior triangle 12
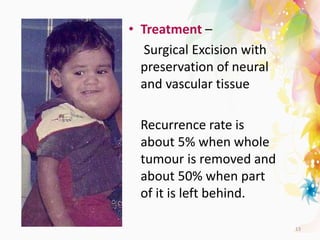
- 13. ŌĆó Treatment ŌĆō Surgical Excision with preservation of neural and vascular tissue Recurrence rate is about 5% when whole tumour is removed and about 50% when part of it is left behind. 13
- 14. ŌĆó Kimura Disease Chronic inflammatory Disorder with painless unilateral inflammation of cervical lymph nodes ŌĆó Kikuchi ŌĆō Fujimoto Disease Necrotizing lymphadenitis chiefly affecting the cervical Lymph nodes ŌĆó Sinus Histiocytosis (Rosai ŌĆō Dorfman Disease) Rare Histiocytic disorder with over production of WBCs 14
- 15. Factors that will aid diagnosis ŌĆó Size ŌĆó Pain / Tenderness ŌĆó Consistency ŌĆó Matting ŌĆó Location 15
- 16. THANK YOU 16




