Challenges in orthopedics nizwa hospital
- 1. Challanges in Orthopedics Nizwa Hospital ŌĆó DR Dinesh Dhar ŌĆó Senior Specialist Orthopedics , Nizwa Hospital
- 2. Why Challenges? ŌĆó Increase Health awareness among people ŌĆó Increased demand for better health facilities ŌĆó Litigations ŌĆó Increase in number of senior citizens ŌĆó Higher Consumer expectations ŌĆó Geographic Location of Nizwa
- 3. Nizwa at Cross Roads
- 7. Everyone pays injury costs THE ANNUAL NATIONAL COST OF INJURY IS ESTIMATED TO BE $ 188 BILLION
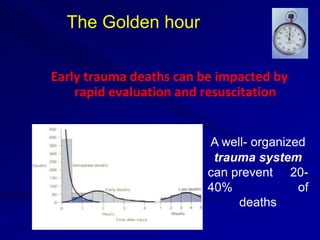
- 9. The Golden hour Early trauma deaths can be impacted by rapid evaluation and resuscitation A well- organized trauma system can prevent 20- 40% of deaths
- 10. Trauma Systems Increased time to definitive care associated with higher mortality rates Trauma system development reduces risk of death from injury Sampalis JS et al. Journal of Trauma, 1999 Nathens AB. J Trauma, 2000
- 11. Five CŌĆÖs of Trauma Care Comprehensive Communication Consistency Cost Commitment
- 12. CHALLENGES OF OUR PRACTICE SETTING Geographic distances Health delivery system under stress Supportig orthopedic speciality lacking in peripheral centres GP s not trained to deal with trauma pts
- 13. Specialty Shortages (Availability) Neurosurgery Vascular surgeons Trauma Surgeons Trained Nursing personnel
- 14. Consequences of Shortages Lack of experience with trauma care Shifting of patients for definitive care Overloading Tertiary Resources Delay in definitive treatment
- 16. Clinical Transfer Issues Unstable trauma transfers Transfers for technology Delays in Transfer Spinal Injuries Vascular Injuries
- 17. Necessary Workup prior to Transfer Hx and PE. IV Access GCS < 8 = Intubate pt X- rays ??? Do not delay transfer for extensive (complete) x-ray evaluation !
- 18. Unstable Trauma Transfers Case 1 Hx: 50 yr male head on collision. ? Pulse at the scene. CPR started Arrived at ED, no pulse, V Fib Defibrillated x1, Sinus tachycardia. BP 70/ Pupils mid positioned and fixed CXR = normal; FAST negative; abdomen soft. Multiple fractures Call for Transfer? NH ??
- 19. Outcome NH called In ambulance pt. develops V fib Defibrillation x5, ACLS protocols Arrives NH , full CPR Pronounced after 5 minutes Appropriate transfer??
- 20. CASE HISTORY 2. 27 Y.O. MALE PEDESTRIAN STRUCK BY CAR TRANSPORTED BY EMS AMBULANCE TO LOCAL HOSPITAL.
- 21. V.S. BP 70/50 P= 60 R= 22 GEN: NON RESPONSIVE CHEST: CLEAR AND SYMETRIC BS + ABD: TENDER LOWER ABDOMEN PELVIS: TENDER ; LARGE SCROTAL HEMATOMA RECTAL: NORMAL , NO LONG BONE FRACTURES
- 22. RESUSITATION / EVALUATION 6 LITERS CRYSTALLOID; 2UNITS PC HYPOTENSIVE/ TACHYCHARDIA CXR =NEG. PELVIS = S-I DISRUPTION , WIDENED SYMPHYSIS ANALGESICS GIVEN FOR PAIN TRANSFERRED TO NH 5 HRS AFTER INITIALARRIVAL
- 23. ARRIVAL NH: BP = 80/ P = 115 RR = 12 CARDIOPULMONARYARREST ASYSTOLIC , NO RESPIRATIONS CODE BLUE : INTUBATED ; RESUSITATED ABG = 6.72/60/565
- 24. RESUSITATION / EVALUATION 8.5 LITERS CRYSTALLOID; 6 UNITS O-NEG , 4 UNITS FFP HGB = 8.2 K+ = 4.5 BUN/CR =12/2.1 PT/PTT = 19/66 ABG = 7.07/38/556 CXR, C-SPINE, PELVIS CYSTOGRAM, FAST = NEG CT HEAD = NEGATIVE
- 25. DEFINITIVE TREATMENT: EXTERNAL FIXATOR APPLIED ANGIOGRAM: BLEEDING LT HYPOGASTRIC ARTERY BRANCHES EMBOLIZATION
- 26. Case 3 ŌĆó 32 yrs old male MVA Type 3c open fracture left proximal femur with injury to femoral vessels on weekend. ŌĆó Initial Resuscitation done , Tertiary centres contacted in Muscat for Vascular injury ŌĆó Nobody ready to take patient for non availability of vascular surgeon. ŌĆó Finally Transferred to Sohar hopsital but too late for vascular repair . ŌĆó End Result Amputation . System Failure? ŌĆó All Vascular surgeons on leave at same time ?
- 27. Delay in Transfer Issues Accessing entry into the Level I / 2 center Available resources for transport Non availability of blood products No facility for ventilation / intubation Mass RTA victims which need evacuation
- 28. Ambulance Service Availability Level of training Leaving the community ŌĆ£uncoveredŌĆØ Undue delay waiting for Driver , Escort personnel?
- 29. Advanced Response Team Air Transports Khareef season Interhospital Transports Trauma ~ 80% Scene Calls 10%
- 30. Khareef season ŌĆó Testing timer for NH Surgical Services ŌĆó 2017 three Major Accidents with sudden influx of mass accident victims ŌĆó Stretches our services to maximum ŌĆó No secondary care hospital between Nizwa and Salalah over 900 km . ŌĆó Only Haima hospital in middle with no Surgical or blood bank services .
- 33. Technology Changes CT scan details the injury CT Available in all hospitals Newer generations with increased detail and speed MRI non availability in Level 2 hospitals C- arm fluroscopy availability in all orthopedic centres
- 34. Technology Changes: Interventional radiology: embolization angio, stents Pelvic Trauma ŌĆō embolization Arterial injury ŌĆō Angio with endovascular stent Spinal Cord injury / Ligament Injuries Knee ŌĆōMRI Facility
- 35. Potential Impact Delays in secondary triage Patient safety ŌĆōIncreased radiation exposure ŌĆōDelays in emergent care Cost ŌĆōPatients billed twice ŌĆōBurden to entire trauma system
- 37. Orthopedic Logistics ŌĆó Shortage of Basic Trauma Implants ŌĆó Delay in procurement of Implants for trauma and other orthopedic services ŌĆó Only one dedicated OT for trauma and elective cases . ŌĆó New Generation Implants not available ŌĆó Common Surgical OPD and Wards ŌĆó Constant Shortage of beds . ŌĆó Subspeciality Training ? ŌĆó Physiotherapy Services under strain
- 38. H Pressures on Orthopedic Services Personnel Shortages ŌĆōSurgeons , Physio. ŌĆōNurses , OT staff Bed capacity/availability Disaster Management Implants Procurement Trauma Sevices
- 39. More than 4 million potential years of productive life are lost annually due to injury, exceeding losses from heart disease, cancer & stroke COMBINED Why we should not so much excited
- 40. In order to succeed, regional trauma centre development is must .It should have adequate facilities and trained personnel.
- 41. Collaboration of Researchers, Educators, Scholars & Teachers (CREST) Opportunities for improvement: CREST? Educational outreach Facilitate referral process Standardized protocols Upgrading remote health Centres ? Improve communication
- 42. TAKE HOME MESSAGE: The Moral Dilemma : ŌĆó Technology is neutral ŌĆō it is neither good nor evil ŌĆó It is up to us to breathe the moral and ethical life into these technologies ŌĆó And then apply them with empathy and compassion for each and every patient
- 44. Thanks