Cleft L-P (2).pptx
- 1. ANAESTHESIA FOR CLEFT LIP-PALATE SURGERY in a one year old child Dr. Swati Daftary Consultant Anaesthesiologist Jaslok Hospital & Research Centre Mumbai ARC 2018
- 2. HISTORY • Simple adhesion of pared margins of the cleft • 1847 – John Snow - Ether for Lip repair • 1850 – Collis – Chloroform for palate repair • 1924 – Magill – intubation for palate repair • 1932 – Magill – flexible armoured tube • 1937-38 – Ayre’s T-piece breathing system • 1955 – Alsop – Oxford ET tube • 1975 – Ring, Adair & Elwyn – RAE ET tube ARC 2018
- 3. THOMAS PHILLIP AYRE (1901-1979) Described T-piece breathing system to overcome the difficulties he had been having while providing anaesthesia for cleft lip and palate surgery in infants. ARC 2018
- 4. CLEFT LIP - PALATE • Second most common congenital deformity • Associated with more than 300 syndromes • Unilateral cleft 1 in 500-1000 live births- highest amongst Asians & Native Americans • Bilateral clefts in 1 in 5000-6500 live births • Cleft lip-palate more common in males • Isolated cleft palate more in females with associated cardiac anomalies in 30 % • Cleft lip and palate (45%), Cleft palate (35%) and cleft lip (20%)
- 5. ETIOLOGY OF CLEFT LIP-PALATE Multifactorial • Genetic factors, father’s age > 40 years • Environmental factors in 1st trimester – Rubella infection, Diabetes Mellitus – Teratogens: steroids, anticonvulsants, alcohol, smoking Embryologically, interruption of mesenchymal migration and fusion of the primitive somite- derived facial elements at 4-7 weeks
- 7. AIMS FOR SURGICAL RECONSTRUCTION • Correction of deformity • To separate the nasal and oral cavities • To improve speech and swallowing mechanisms • To prevent middle ear disease and improve hearing • To provide normal dental occlusion ARC 2018
- 8. APPROPRIATE TIME FOR CLEFT LIP – PALATE REPAIR Conventional Lip repair: Kilner’s rule of 10 10 weeks of age, 10 lb body weight, Hb 10 gm% and WBC count < 10,000/cmm Conventional Palate repair: Bigger the child better, able to withstand the stress of surgery and anaesthesia ARC 2018
- 9. • Primary cleft lip repair at 2-4 months / 6-12weeks • Primary palate repair at 6 months or latest by 12 months for normal speech and velopharyngeal competence • Lip / nose revision in early childhood • Pharyngoplasty at the age of 5-15 years • Palatal revision and alveolar bone graft at 10 years • Rhinoplasty and Maxillary osteotomy between 17- 20 years of age RECENT TREND FOR CLEFT AND RELATED REPAIRS
- 11. CLEFT LIP-PALATE: SURGICAL RECOSTRUCTION • Soft tissue- dissection, undermining and creating flaps for rotation & advancement • Bony tissue- bone / mucoperiosteal flaps, bone grafting from ribs, iliac crest or skull, tongue flap ARC 2018
- 12. POSITION FOR SURGERY: ROSE POSITION ARC 2018
- 13. ANAESTHESIA FOR CLEFT Sx “THE BIG LITTLE PROBLEM”
- 14. ISSUES IN A CLEFT PALATE CHILD • Associated defects and cardiac anomalies • Chronic airway obstruction/sleep apnoea • Right ventricular hypertrophy and cor pulmonale due to chronic hypoxia • Anticipated difficult intubation • Malnutrition, anaemia, dehydration, may require grouping cross matching of blood • Psychological aspect: depression due to disfigurement and difficulties in speech ARC 2018
- 15. PREOPERATIVE EVALUATION • Thorough medical history and examination to uncover associated anomalies, difficult airway • Acute infection related to chronic ENT problems • Investigations: Hb for the isolated cleft lip CBC, coagulation profile, X-ray chest, ECG, 2D ECHO depending on associated anomalies • NBM instructions • Premedication: ± antisialogouge, anticholinergic drug –sedation in patients ≥ 9 mths of age without airway compromise
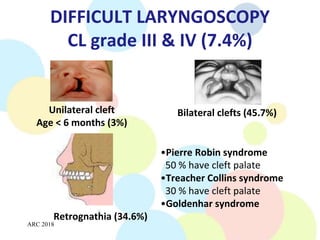
- 16. DIFFICULT LARYNGOSCOPY CL grade III & IV (7.4%) Bilateral clefts (45.7%) Unilateral cleft Age < 6 months (3%) Retrognathia (34.6%) •Pierre Robin syndrome 50 % have cleft palate •Treacher Collins syndrome 30 % have cleft palate •Goldenhar syndrome ARC 2018
- 17. PREFORMED ET TUBE Oxford tube RAE Tube Tube is placed in midline with the upper lip immobile and not distorted.
- 18. PERIOPERATIVE MONITORING • Observation: Colour, capillary refill, blood loss, airway pressures, postoperatively rate and depth of respiration • Precordial stethoscope: Heart & breath sounds • ECG: Cardiac arrhythmia • Pulse oximetry and capnometry • NIBP: Intravascular volume & cardiac output • Temperature • Peripheral nerve stimulator ARC 2018
- 19. INDUCTION OF ANAESTHESIA • Difficult mask ventilation in clefts with associated craniofacial anomalies and retrognathia ⇒ oro- pharyngeal airway + CPAP • If anticipated difficult laryngoscopy (Cormack and Lehane grade III & IV) – spontaneous inhalation induction with airway assessment – Intubation through LMA, assisted by fiberoptic scope – muscle relaxant and ET intubation (video laryngoscope) • Care of left sided cleft & extensive cleft • Oral RAE tube / Oxford tube – midline placement OR Armour reinforced ETT / flexometallic ETT • Care of eyes, padding, positioning of patient, circuit
- 20. ANAESTHESIA MAINTENANCE Airway is shared with the surgeon hence adequacy must be assessed especially after 1. Patient positioning - exaggerated extension of the neck ⇒ accidental extubation 2. Placement of Dingman mouth gag- used for surgical exposure and ETT stabilization 3. Placement of pharyngeal pack to prevent aspiration of blood All these may cause compression / kinking of the tube ARC 2018
- 21. DINGMAN MOUTH GAG ARC 2018
- 22. MAINTENANCE OF ANAESTHESIA (contd.) • Gas, oxygen, suitable inhalational agent, short acting opioid, muscle relaxant and artificial ventilation • Surgical incision infiltrated using saline / LA with adrenaline (< 10 μgm / kg) • Planning for post-operative pain relief • Fluid and temperature maintenance ARC 2018
- 23. PERIOPERATIVE PAIN RELIEF Pharmocological: Combination of short acting opioids, Paracetamol & NSAIDs (NSAIDs not preferred in infants < 6 months and first 12 hours postoperatively) Regional blocks: Cleft Lip ⇒ Bilateral Infraorbital Block (IOB) / Peri- incisional infiltration Cleft Palate ⇒ Bilateral Greater palatine nerve block ARC 2018
- 24. INFRA-ORBITAL NERVE BLOCK A- Transcutaneous approach B- Transoral approach
- 25. INFRA-ORBITAL NERVE BLOCK Area of sensory blockade Infraorbital Nerve Site of injection 1ml 0.25%/0.5% Bupicaine with 1:200000 adrenaline on both sides Bosenberg AT, Kimble FW. Infraorbital nerve block in neonates for cleft lip repair: anatomical study and clinical application. British Journal of Anaesthesia 1995; 74: 506-508 Gaonkar V, Daftary S R. Comparison of preoperative infraorbital block with peri-incisional infiltration for postoperative pain relief in cleft lip surgeries. Indian J Plast Surg 2004;37:105-9
- 26. GREATER PALATINE NERVE BLOCK The greater palatine foramen situated medial & anterior to the second upper molar Nerve is blocked on either side as it exits from the foramen with 1 ml of 0.25% bupivacaine with 1:200,000 adrenaline, submucous injection using 27G needle ARC 2018
- 27. POST-OPERATIVE MANAGEMENT • Check for pharyngeal pack, bleeding & secretions before reversal, extubation • Avoid putting in a laryngoscope • Extubation in fully awake child • In PACU, child in lateral position to facilitate drainage of blood and secretions • Straight sleeves or boxer’s bandage to restrain the hands from touching the surgical site ARC 2018
- 28. POST-OPERATIVE COMPLICATIONS Early complications (26%): More common after palate surgery, child to be observed in PICU/HDU • Airway obstruction: Because of constricting flaps, nasopharyngeal oedema and prolonged surgery (> 2-3 hrs) ⇒ massive macroglossia Management: nasopharyngeal airway / tongue stitch for 48 hours / postoperative intubation • Bleeding: may require re-exploration and blood transfusion if excessive ARC 2018
- 29. AIRWAY OBSTRUCTION POST PALATE REPAIR Treatment: • Nasopharyngeal airway • Tongue stitch ARC 2018
- 30. SECONDARY SURGERY To revise residual defects: • Velopharyngeal incompetence • Palatal dehiscence / Oronasal fistula • Dental malocclusion • Residual cosmetic deformity eg. Cleft rhinoplasty ARC 2018
- 31. VELOPHARYNGEAL INCOMPETENCE Diagnostic features: Hypernasality, misarticulation and nasal regurgitation Confirmation with video nasoendoscopy Treatment: Pharyngeal flap Anaesthetic importance: In operated patients • Obstructive sleep apnoea (OSA) - 70-80 % • Blind nasotracheal intubation & nasogastric tube insertions are contraindicated during subsequent surgeries ARC 2018
- 32. SUMMARY 1. Considering cleft lip and palate a) It is the commonest congenital abnormality b) Cleft palate cannot occur without cleft lip c) It is more common in males d) Cleft lip is more often found on the left side e) Associated abnormalities are very rare FFTTF ARC 2018
- 33. 2. Preoperative assessment of the child with cleft lip and palate a) The presence of rhinorrhoea means surgery should be cancelled b) Bilateral cleft lip predicts difficult laryngoscopy c) Bilateral cleft lip-palate predicts an increased risk of postoperative respiratory complications d) A history of apnoea during feeds may indicate chronic airway obstruction e) Sedative premedication is useful and promotes smooth induction in bilateral cleft lip-palate FTTTF ARC 2018
- 34. 3. When inducing anaesthesia in a child with isolated cleft lip and palate a) Intravenous induction is mandatory b) The use of neuromuscular blocking drugs is contraindicated c) Difficulty with mask ventilation is common d) Difficult laryngoscopy occurs in the majority of patients e) Deferring surgery until the child is older may make airway management easier FFFFT ARC 2018
- 35. 4. Considering primary surgical repair of cleft lip and palate a) Cleft lip may be repaired in the neonatal period b) Cleft palate repair should be delayed until the child has learned to speak c) Infiltration of local anaesthetic is contraindicated as it distorts the surgical field d) Blood transfusion is uncommon e) It is rare for patients to require any further surgery after primary repair TFFFF ARC 2018
- 36. 5. Anaesthesia for cleft lip and palate surgery a) Problems with the tube are rare once the mouth gag has been inserted b) Spontaneous ventilation techniques are not suitable for neonates and infants c) Standard drawover systems are suitable for all patients d) Opioids are contraindicated as they may cause postoperative airway obstruction e) Infraorbital nerve blocks can provide adequate postoperative analgesia for isolated cleft lip repair FTFFT
- 37. 6. Airway obstruction after cleft lip and palate repair a) Is most likely to occur in children with pre- operative airway problems b) May be due to inadequate mouth breathing c) May be treated with insertion of a nasopharyngeal airway d) Oropharyngeal airways should be avoided e) Will always require re-intubation TTTTF ARC 2018