Clinical aspects of upper and lower motor neuron lesions
Download as PPTX, PDF14 likes2,286 views
Lecture by Prof. Osama Shukir Muhammed Amin FRCP(Edin), FRCP(Glasg), FRCP(Ire), FRCP(Lond), FACP, FAHA about the clinical aspects of upper and lower motor neuron lesions.
1 of 15
Downloaded 76 times













Recommended
Upper and lower motor neuron



Upper and lower motor neuronMuhammad Saim
╠²
Upper motor neurons originate in the brain and convey signals for voluntary movement through descending pathways to lower motor neurons. Lower motor neurons originate in the spinal cord and brainstem and directly innervate skeletal muscles. An upper motor neuron lesion causes spastic weakness without atrophy while a lower motor neuron lesion causes flaccid paralysis with atrophy.Transverse myelitis



Transverse myelitisPRADEEPA MANI
╠²
INTRODUCTION, DEFINITION, ETIOLOGY, EPIDEMIOLOGY, TYPES, PATHOLOGY, CLINICAL COURSE, CLINICAL FEATURES, DIAGNOSIS, DIFFERENTIAL DIAGNOSIS, MANAGEMENT AND PROGNOSISStroke syndromes



Stroke syndromesmrinal joshi
╠²
1. Stroke is defined as a nontraumatic brain injury caused by occlusion or rupture of cerebral blood vessels that results in sudden neurological deficits.
2. The most common types of stroke are ischemic (85%) and hemorrhagic (15%). Ischemic strokes are further classified as thrombotic, embolic, or lacunar.
3. Major risk factors for stroke include hypertension, heart disease, diabetes, smoking, and older age. Location of brain injury determines the specific neurological symptoms, such as deficits on one side of the body for middle cerebral artery strokes.Tremor



Tremorbausher willayat
╠²
This document discusses different types of tremors, including essential tremor, parkinsonian tremor, enhanced physiologic tremor, drug-induced tremor, cerebellar tremor, psychogenic tremor, dystonic tremor, and Wilson's disease tremor. It provides details on symptoms, causes, diagnostic criteria and approach for each type. The most common tremors are essential tremor, parkinsonian tremor, and enhanced physiologic tremor. A thorough history, physical exam, and categorization of tremor characteristics are important for diagnosis.MUSCLE TONE.pptx



MUSCLE TONE.pptxIndhujaKarunakaran2
╠²
This document defines and describes various types of muscle tone and how they are assessed clinically. It can be summarized as:
1) Muscle tone refers to the tension present in relaxed muscles and their resistance to passive movement. It is assessed using tests like Babinski's tonus test and head dropping.
2) Extrapyramidal rigidity is assessed using tests like shoulder shaking and produces increased resistance to passive movement equally in all directions.
3) Paratonia involves an abnormal response to passive movement seen in frontal lobe diseases, either resisting movement (gegenhalten) or assisting it too much (mitgehen). It is assessed using tests like limb placement.Tracts of spinal cord (1)



Tracts of spinal cord (1)Zulcaif Ahmad
╠²
This document describes the different tracts of the spinal cord, dividing them into short tracts within the spinal cord, and long tracts connecting the spinal cord to other parts of the central nervous system. The long tracts are further divided into ascending tracts traveling from spinal cord to brain, and descending tracts traveling from brain to spinal cord. The descending tracts are then described in more detail, including the pyramidal, extrapyramidal, vestibular, reticular, tectospinal, rubrospinal, and olivospinal tracts.Diseases of Spinal Cord



Diseases of Spinal CordA T M Hasibul Hasan
╠²
1) The document discusses the anatomy, imaging, classification, clinical approach, and localization of spinal cord pathology. It covers various spinal cord diseases including compressive myelopathy, non-compressive myelopathy, intramedullary and extramedullary lesions.
2) Special patterns of presentation like Brown-Sequard syndrome, anterior/posterior cord syndromes, and central cord syndrome are explained. Localization of lesions in the cervical, thoracic, lumbar, and sacral regions is outlined.
3) The clinical approach involves considering features like onset, progression, bladder involvement, presence of pain, and nature of paraplegia to classify spinal cord diseases. Key points on examination include types of motor and sensoryMyelopathy 1



Myelopathy 1sunil bhatt
╠²
This document provides information on myelopathy and spinal cord lesions:
- Myelopathy describes any neurological deficit related to the spinal cord, and can cause quadriplegia, paraplegia, sensory deficits, and autonomic disturbances. It can be inflammatory (myelitis) or vascular in nature (vascular myelopathy).
- Cervical spondylotic myelopathy is the most common form of myelopathy. Lesions of the spinal cord can be compressive (intramedullary or extramedullary) or non-compressive.
- Different levels of spinal cord lesions present with distinct symptoms, such as sensory losses in specific dermatomes or weaknesses of particular muscles. Features helpUpper and Lower motor neuron lesions



Upper and Lower motor neuron lesionsDr. Aryan (Anish Dhakal)
╠²
Upper and lower motor neurons control skeletal muscle contraction through a two-neuron pathway. Upper motor neurons originate in the brain and direct the activity of lower motor neurons in the spinal cord and brainstem. Lesions of upper motor neurons cause spastic weakness, hyperreflexia, and loss of fine motor skills. Lesions of lower motor neurons result in flaccid paralysis, loss of reflexes, and muscular atrophy. Differentiating between upper and lower motor neuron lesions is important for determining the neurological level and prognosis.Spinal cord syndromes



Spinal cord syndromesDr. Mohammed Sadiq Azam M.D.
╠²
The document discusses various spinal cord syndromes classified as either complete or incomplete cord syndromes. It provides details on complete cord transection which results in paralysis, loss of sensation, and autonomic dysfunction below the level of injury. Brown-Sequard syndrome and central cord syndrome are discussed as examples of incomplete cord syndromes characterized by mixed upper and lower motor neuron findings on one or both sides of the body. The document also covers syndromes involving specific regions of the spinal cord including conus medullaris, cauda equina, and anterior spinal artery syndromes.DERMATOMES AND MYOTOMES



DERMATOMES AND MYOTOMESDr.Monica Dhanani
╠²
Dermatomes:- the sensory distribution of each nerve root is called the dermatomes.
The area of the skin supplied by a single nerve root
Ataxia



AtaxiaFizio
╠²
This document provides information on ataxia, including its definition as a neurological disorder involving lack of voluntary muscle coordination. It describes the main types of ataxia and several specific hereditary forms. Key points include Friedreich's ataxia being the most common hereditary form, typically beginning in childhood. Imaging tests and lab work can help evaluate for various causes, while genetic testing can confirm hereditary types. Overall the document outlines the classification, causes, clinical features and investigative approach for ataxia.Syringomyelia



SyringomyeliaShanavas Cholakkal
╠²
This document provides an overview of syringomyelia, including:
- It is a spinal cord cavity filled with cerebrospinal fluid, with a prevalence of 9 per 100,000 people.
- It can be caused by traumatic injury, Chiari malformation, or other craniovertebral junction anomalies.
- Symptoms depend on the location and extent of the syrinx and can include sensory loss, weakness, pain, and autonomic dysfunction.
- Magnetic resonance imaging is the best way to diagnose and assess syringomyelia.
- Treatment may involve surgery to decompress the craniovertebral junction, open the syrinx, or place a shuntWrist drop



Wrist dropDrDivya Chandil
╠²
This document discusses radial nerve palsy, which is an injury to the radial nerve resulting in impaired nerve function and causing wrist drop. Wrist drop is the characteristic clinical sign where the wrist hangs flaccidly and cannot be extended. Causes of radial nerve palsy include sleeping with one's arm compressed (e.g. Saturday night palsy from falling asleep with one's arm on a chair or bar), compression from walking with a crutch (crutch palsy), or from another person sleeping on one's arm (honeymoon palsy). Radial nerve palsy results in weakness of wrist and finger extension and grip. Treatment involves reducing pain, increasing range of motion, and restoringBLOOD SUPPLY of brain and spinal cord.pptx



BLOOD SUPPLY of brain and spinal cord.pptxmunnam37
╠²
The document summarizes the blood supply of the brain and spinal cord. It discusses the major arteries including the internal carotid, vertebral, and basilar arteries. It describes the branches and territories supplied by the anterior, middle, and posterior cerebral arteries. It also discusses important anastomoses like the Circle of Willis. Various artery syndromes are summarized such as anterior cerebral artery occlusion presenting with contralateral leg weakness. Important veins are also mentioned along with clinical correlations of arterial occlusions.Pyramidal tract



Pyramidal tractDr Vinay Patidar patidar
╠²
The pyramidal tract provides voluntary control of muscle movement and consists of the corticospinal tract and corticobulbar tract. The corticospinal tract controls limb movements from the motor cortex to spinal cord. The corticobulbar tract controls facial and neck muscles from the motor cortex to brainstem. Damage to these tracts can cause weakness, increased muscle tone and reflexes, and abnormal movements on the opposite side of the body.pyramidal, extrapyramidal pathways 



pyramidal, extrapyramidal pathways med_students0
╠²
The document summarizes the descending motor systems, including the pyramidal and extrapyramidal tracts. It describes the corticobulbospinal tract (pyramidal tract) in detail, including its corticobulbar and corticospinal divisions. It also discusses the rubrospinal, reticulospinal, vestibulospinal, and tectospinal tracts that make up the extrapyramidal tracts. Finally, it provides information about the primary motor area and premotor area of the cerebral cortex.Sensory ataxia



Sensory ataxiaSusanth Mj
╠²
This document discusses sensory ataxia, including its causes, clinical presentation, and differential diagnosis. Sensory ataxia results from disorders of the cerebellum, vestibular system, or sensory pathways. It is characterized by incoordination without significant weakness. Key findings include impaired proprioception, positive Romberg's sign, pseudoathetosis, and loss of vibration or joint position sense. Causes include peripheral neuropathies, paraneoplastic disorders, infections like HIV, autoimmune conditions like Sjogren's syndrome, and medications like chemotherapy. Dorsal root ganglionopathies commonly underlie sensory ataxia and can be assessed through nerve conduction studies and lumbar puncture. Distinguishing sensoryCompressive Myelopathy



Compressive MyelopathyStanley Medical College, Department of Medicine
╠²
1) The document discusses various causes of compressive myelopathy including spondylosis, herniated discs, spinal stenosis, and tuberculosis. It describes the clinical features and treatments for different levels of involvement in the cervical and lumbar spine.
2) Imaging techniques like MRI, CT myelogram, and X-rays are used to identify compression of the spinal cord or nerve roots from conditions like herniations, osteophytes, and tuberculosis lesions.
3) Surgical intervention may be indicated for moderate to severe myelopathy, progressive neurological deficits, or failure of conservative treatment. The goal is to decompress the spinal cord and relieve compression.Stroke Syndromes - By Prof. Dr.Dhanarj.M (Sr.Consultant Neurologist)



Stroke Syndromes - By Prof. Dr.Dhanarj.M (Sr.Consultant Neurologist)Ramesh Babu
╠²
This document discusses the localization of stroke syndromes through clinical evaluation. It outlines three steps: 1) clinically localizing the site of the lesion, 2) identifying the involved vascular territory and vessel, and 3) correlating with imaging findings. It then describes in detail the various anterior and posterior circulation stroke syndromes, highlighting the characteristic clinical features associated with lesions in different areas supplied by major arteries. The importance of careful clinical localization in combination with imaging to determine etiology and guide treatment is emphasized. Limitations where clinical evaluation alone may not be definitive are also noted.Extrapyramidal tracts and disorders



Extrapyramidal tracts and disordersPriyanka Gupta
╠²
The document discusses various extrapyramidal tracts in the brain and spinal cord that help control motor function. It describes the rubrospinal, reticulospinal, olivospinal, tectospinal, and vestibulospinal tracts, including their origins, pathways, and functions. Common extrapyramidal disorders like Parkinson's disease, chorea, hemiballism, athetosis, dystonia, and tardive dyskinesia are also briefly outlined.Neural control of bladder



Neural control of bladderPravinKumar582
╠²
This PPT is for educational purpose for neural control of bladder, along with various types of neurogenic bladderCerebellar ataxia



Cerebellar ataxiaHanaa Nooh
╠²
The document discusses cerebellar ataxia, a disorder caused by damage to the cerebellum that controls coordination. It causes loss of coordination, balance problems, and slurred speech. The cerebellum coordinates muscle movement and is located in the hindbrain. Causes include viruses, alcohol, tumors, and toxins. Symptoms are diagnosed through neurological exams, imaging scans, and lab tests. Treatment focuses on physical therapy, assistive devices, and treating any underlying causes to ease symptoms and improve quality of life. Prevention involves vaccinations to reduce risk of viral infections that can lead to cerebellar ataxia.Superficial and deep reflexes!



Superficial and deep reflexes!Muhammadasif909
╠²
Reflex activity is the response to a peripheral stimulation that occurs without our consciousness.
Is an involuntary response to a stimulus.
It is a type of protective mechanism.
Syringomyelia



SyringomyeliaVaibhaviParmar7
╠²
Syringomyelia is a condition where a cyst, called a syrinx, develops in the spinal cord. It most commonly affects the lower cervical spine. It is often associated with abnormalities of the skull or spinal column. The majority of cases are linked to Chiari malformation type 1, where the cerebellar tonsils are displaced into the spinal canal. Symptoms vary depending on the location of the syrinx but can include pain, loss of sensation, muscle weakness or atrophy, and autonomic dysfunction. Diagnosis is made using imaging like MRI. Treatment involves surgery to decompress pressure on the spinal cord like laminectomy with the goal of resolving the syrinx.Transverse myelitis



Transverse myelitisdrsurajkanase7
╠²
Transverse myelitis is a rare neurological condition where the spinal cord becomes inflamed across its width. It is often caused by an autoimmune response following a viral infection. Symptoms depend on the level of spinal cord involvement and may include sensory changes, motor weakness, and sphincter disturbances. Diagnosis involves ruling out other causes and showing signs of spinal cord inflammation. The goals of physiotherapy are to improve strength, mobility, and independence through exercises and management of issues like spasticity and skin care.Involuntary movements



Involuntary movementsVitrag Shah
╠²
- The basal ganglia are a group of subcortical nuclei that are part of neuronal circuits involved in motor control. Abnormalities in basal ganglia output can cause either hypokinetic or hyperkinetic involuntary movements.
- The document discusses various types of involuntary movements including Parkinsonism, tremor, chorea, dystonia, tics, and ataxia. It provides details on the clinical features and pathogenesis of these movement disorders.
- Treatment options discussed include dopamine agonists and antagonists, which aim to restore the imbalance of basal ganglia activity underlying different hyperkinetic and hypokinetic movement disorders.Syringomyelia



SyringomyeliaLiew Boon Seng
╠²
This document provides an overview of syringomyelia, including its pathogenesis, pathology, classification, clinical features, and natural history. Syringomyelia is a condition characterized by fluid-filled cavities within the spinal cord. It most commonly affects the cervical and thoracic regions. Clinical features include pain and sensory loss. The natural history varies, but symptoms typically progress slowly over years, with some patients experiencing stabilization or spontaneous resolution in rare cases.Clinical Aspects of Upper and Lower Motor Neuron Lesions



Clinical Aspects of Upper and Lower Motor Neuron LesionsJeremy McCool
╠²
A lecture I gave to undergraduate medical students of the International Medical University, Malaysia (IMU University). Neurology and Neurosciences. Clinical Aspects of Upper and Lower Motor Neuron Lesions



Clinical Aspects of Upper and Lower Motor Neuron LesionsJeremy McCool
╠²
A lecture given by Prof. Dr. Osama Shukir Muhammed Amin FRCP to semester 4 students of the International Medical University, Malaysia (now IMU University), about the Clinical Aspects of Upper and Lower Motor Neuron Lesions.More Related Content
What's hot (20)
Upper and Lower motor neuron lesions



Upper and Lower motor neuron lesionsDr. Aryan (Anish Dhakal)
╠²
Upper and lower motor neurons control skeletal muscle contraction through a two-neuron pathway. Upper motor neurons originate in the brain and direct the activity of lower motor neurons in the spinal cord and brainstem. Lesions of upper motor neurons cause spastic weakness, hyperreflexia, and loss of fine motor skills. Lesions of lower motor neurons result in flaccid paralysis, loss of reflexes, and muscular atrophy. Differentiating between upper and lower motor neuron lesions is important for determining the neurological level and prognosis.Spinal cord syndromes



Spinal cord syndromesDr. Mohammed Sadiq Azam M.D.
╠²
The document discusses various spinal cord syndromes classified as either complete or incomplete cord syndromes. It provides details on complete cord transection which results in paralysis, loss of sensation, and autonomic dysfunction below the level of injury. Brown-Sequard syndrome and central cord syndrome are discussed as examples of incomplete cord syndromes characterized by mixed upper and lower motor neuron findings on one or both sides of the body. The document also covers syndromes involving specific regions of the spinal cord including conus medullaris, cauda equina, and anterior spinal artery syndromes.DERMATOMES AND MYOTOMES



DERMATOMES AND MYOTOMESDr.Monica Dhanani
╠²
Dermatomes:- the sensory distribution of each nerve root is called the dermatomes.
The area of the skin supplied by a single nerve root
Ataxia



AtaxiaFizio
╠²
This document provides information on ataxia, including its definition as a neurological disorder involving lack of voluntary muscle coordination. It describes the main types of ataxia and several specific hereditary forms. Key points include Friedreich's ataxia being the most common hereditary form, typically beginning in childhood. Imaging tests and lab work can help evaluate for various causes, while genetic testing can confirm hereditary types. Overall the document outlines the classification, causes, clinical features and investigative approach for ataxia.Syringomyelia



SyringomyeliaShanavas Cholakkal
╠²
This document provides an overview of syringomyelia, including:
- It is a spinal cord cavity filled with cerebrospinal fluid, with a prevalence of 9 per 100,000 people.
- It can be caused by traumatic injury, Chiari malformation, or other craniovertebral junction anomalies.
- Symptoms depend on the location and extent of the syrinx and can include sensory loss, weakness, pain, and autonomic dysfunction.
- Magnetic resonance imaging is the best way to diagnose and assess syringomyelia.
- Treatment may involve surgery to decompress the craniovertebral junction, open the syrinx, or place a shuntWrist drop



Wrist dropDrDivya Chandil
╠²
This document discusses radial nerve palsy, which is an injury to the radial nerve resulting in impaired nerve function and causing wrist drop. Wrist drop is the characteristic clinical sign where the wrist hangs flaccidly and cannot be extended. Causes of radial nerve palsy include sleeping with one's arm compressed (e.g. Saturday night palsy from falling asleep with one's arm on a chair or bar), compression from walking with a crutch (crutch palsy), or from another person sleeping on one's arm (honeymoon palsy). Radial nerve palsy results in weakness of wrist and finger extension and grip. Treatment involves reducing pain, increasing range of motion, and restoringBLOOD SUPPLY of brain and spinal cord.pptx



BLOOD SUPPLY of brain and spinal cord.pptxmunnam37
╠²
The document summarizes the blood supply of the brain and spinal cord. It discusses the major arteries including the internal carotid, vertebral, and basilar arteries. It describes the branches and territories supplied by the anterior, middle, and posterior cerebral arteries. It also discusses important anastomoses like the Circle of Willis. Various artery syndromes are summarized such as anterior cerebral artery occlusion presenting with contralateral leg weakness. Important veins are also mentioned along with clinical correlations of arterial occlusions.Pyramidal tract



Pyramidal tractDr Vinay Patidar patidar
╠²
The pyramidal tract provides voluntary control of muscle movement and consists of the corticospinal tract and corticobulbar tract. The corticospinal tract controls limb movements from the motor cortex to spinal cord. The corticobulbar tract controls facial and neck muscles from the motor cortex to brainstem. Damage to these tracts can cause weakness, increased muscle tone and reflexes, and abnormal movements on the opposite side of the body.pyramidal, extrapyramidal pathways 



pyramidal, extrapyramidal pathways med_students0
╠²
The document summarizes the descending motor systems, including the pyramidal and extrapyramidal tracts. It describes the corticobulbospinal tract (pyramidal tract) in detail, including its corticobulbar and corticospinal divisions. It also discusses the rubrospinal, reticulospinal, vestibulospinal, and tectospinal tracts that make up the extrapyramidal tracts. Finally, it provides information about the primary motor area and premotor area of the cerebral cortex.Sensory ataxia



Sensory ataxiaSusanth Mj
╠²
This document discusses sensory ataxia, including its causes, clinical presentation, and differential diagnosis. Sensory ataxia results from disorders of the cerebellum, vestibular system, or sensory pathways. It is characterized by incoordination without significant weakness. Key findings include impaired proprioception, positive Romberg's sign, pseudoathetosis, and loss of vibration or joint position sense. Causes include peripheral neuropathies, paraneoplastic disorders, infections like HIV, autoimmune conditions like Sjogren's syndrome, and medications like chemotherapy. Dorsal root ganglionopathies commonly underlie sensory ataxia and can be assessed through nerve conduction studies and lumbar puncture. Distinguishing sensoryCompressive Myelopathy



Compressive MyelopathyStanley Medical College, Department of Medicine
╠²
1) The document discusses various causes of compressive myelopathy including spondylosis, herniated discs, spinal stenosis, and tuberculosis. It describes the clinical features and treatments for different levels of involvement in the cervical and lumbar spine.
2) Imaging techniques like MRI, CT myelogram, and X-rays are used to identify compression of the spinal cord or nerve roots from conditions like herniations, osteophytes, and tuberculosis lesions.
3) Surgical intervention may be indicated for moderate to severe myelopathy, progressive neurological deficits, or failure of conservative treatment. The goal is to decompress the spinal cord and relieve compression.Stroke Syndromes - By Prof. Dr.Dhanarj.M (Sr.Consultant Neurologist)



Stroke Syndromes - By Prof. Dr.Dhanarj.M (Sr.Consultant Neurologist)Ramesh Babu
╠²
This document discusses the localization of stroke syndromes through clinical evaluation. It outlines three steps: 1) clinically localizing the site of the lesion, 2) identifying the involved vascular territory and vessel, and 3) correlating with imaging findings. It then describes in detail the various anterior and posterior circulation stroke syndromes, highlighting the characteristic clinical features associated with lesions in different areas supplied by major arteries. The importance of careful clinical localization in combination with imaging to determine etiology and guide treatment is emphasized. Limitations where clinical evaluation alone may not be definitive are also noted.Extrapyramidal tracts and disorders



Extrapyramidal tracts and disordersPriyanka Gupta
╠²
The document discusses various extrapyramidal tracts in the brain and spinal cord that help control motor function. It describes the rubrospinal, reticulospinal, olivospinal, tectospinal, and vestibulospinal tracts, including their origins, pathways, and functions. Common extrapyramidal disorders like Parkinson's disease, chorea, hemiballism, athetosis, dystonia, and tardive dyskinesia are also briefly outlined.Neural control of bladder



Neural control of bladderPravinKumar582
╠²
This PPT is for educational purpose for neural control of bladder, along with various types of neurogenic bladderCerebellar ataxia



Cerebellar ataxiaHanaa Nooh
╠²
The document discusses cerebellar ataxia, a disorder caused by damage to the cerebellum that controls coordination. It causes loss of coordination, balance problems, and slurred speech. The cerebellum coordinates muscle movement and is located in the hindbrain. Causes include viruses, alcohol, tumors, and toxins. Symptoms are diagnosed through neurological exams, imaging scans, and lab tests. Treatment focuses on physical therapy, assistive devices, and treating any underlying causes to ease symptoms and improve quality of life. Prevention involves vaccinations to reduce risk of viral infections that can lead to cerebellar ataxia.Superficial and deep reflexes!



Superficial and deep reflexes!Muhammadasif909
╠²
Reflex activity is the response to a peripheral stimulation that occurs without our consciousness.
Is an involuntary response to a stimulus.
It is a type of protective mechanism.
Syringomyelia



SyringomyeliaVaibhaviParmar7
╠²
Syringomyelia is a condition where a cyst, called a syrinx, develops in the spinal cord. It most commonly affects the lower cervical spine. It is often associated with abnormalities of the skull or spinal column. The majority of cases are linked to Chiari malformation type 1, where the cerebellar tonsils are displaced into the spinal canal. Symptoms vary depending on the location of the syrinx but can include pain, loss of sensation, muscle weakness or atrophy, and autonomic dysfunction. Diagnosis is made using imaging like MRI. Treatment involves surgery to decompress pressure on the spinal cord like laminectomy with the goal of resolving the syrinx.Transverse myelitis



Transverse myelitisdrsurajkanase7
╠²
Transverse myelitis is a rare neurological condition where the spinal cord becomes inflamed across its width. It is often caused by an autoimmune response following a viral infection. Symptoms depend on the level of spinal cord involvement and may include sensory changes, motor weakness, and sphincter disturbances. Diagnosis involves ruling out other causes and showing signs of spinal cord inflammation. The goals of physiotherapy are to improve strength, mobility, and independence through exercises and management of issues like spasticity and skin care.Involuntary movements



Involuntary movementsVitrag Shah
╠²
- The basal ganglia are a group of subcortical nuclei that are part of neuronal circuits involved in motor control. Abnormalities in basal ganglia output can cause either hypokinetic or hyperkinetic involuntary movements.
- The document discusses various types of involuntary movements including Parkinsonism, tremor, chorea, dystonia, tics, and ataxia. It provides details on the clinical features and pathogenesis of these movement disorders.
- Treatment options discussed include dopamine agonists and antagonists, which aim to restore the imbalance of basal ganglia activity underlying different hyperkinetic and hypokinetic movement disorders.Syringomyelia



SyringomyeliaLiew Boon Seng
╠²
This document provides an overview of syringomyelia, including its pathogenesis, pathology, classification, clinical features, and natural history. Syringomyelia is a condition characterized by fluid-filled cavities within the spinal cord. It most commonly affects the cervical and thoracic regions. Clinical features include pain and sensory loss. The natural history varies, but symptoms typically progress slowly over years, with some patients experiencing stabilization or spontaneous resolution in rare cases.Similar to Clinical aspects of upper and lower motor neuron lesions (20)
Clinical Aspects of Upper and Lower Motor Neuron Lesions



Clinical Aspects of Upper and Lower Motor Neuron LesionsJeremy McCool
╠²
A lecture I gave to undergraduate medical students of the International Medical University, Malaysia (IMU University). Neurology and Neurosciences. Clinical Aspects of Upper and Lower Motor Neuron Lesions



Clinical Aspects of Upper and Lower Motor Neuron LesionsJeremy McCool
╠²
A lecture given by Prof. Dr. Osama Shukir Muhammed Amin FRCP to semester 4 students of the International Medical University, Malaysia (now IMU University), about the Clinical Aspects of Upper and Lower Motor Neuron Lesions.Motor Neuron Disease and PT Mx



Motor Neuron Disease and PT Mxrichamistry3
╠²
Motor neurons are neurons that control muscles and glands. Their cell bodies are located in the brainstem or spinal cord, and their axons project to muscles. Motor neuron disease (MND) refers to conditions where motor neurons degenerate, leading to muscle weakness and atrophy. The most common type is amyotrophic lateral sclerosis (ALS), where both upper and lower motor neurons are affected. In ALS, muscles weaken and waste away as motor neurons die, and symptoms may include limb weakness, bulbar problems like slurred speech, and respiratory issues. The disease progresses as motor neurons continue to deteriorate over time.Motor neuron diseases



Motor neuron diseasesDr Ashish
╠²
Upper motor neurons convey impulses for voluntary motor activity and exert control over lower motor neurons, which directly innervate skeletal muscle. Upper motor neuron cell bodies are located in the motor cortex and premotor areas. Their axons form tracts that project to lower motor neurons in the brainstem and spinal cord. Lower motor neuron cell bodies are located in the brainstem and spinal cord. Damage to upper motor neurons results in spasticity and hyperreflexia, while lower motor neuron damage causes weakness, atrophy, fasciculations and hyporeflexia. Amyotrophic lateral sclerosis is a motor neuron disorder characterized by both upper and lower motor neuron degeneration.Limb Weakness (Part 1), with some clinical examples and imaging



Limb Weakness (Part 1), with some clinical examples and imagingJeremy McCool
╠²
A lecture given by Prof. Dr. Osama Shukir Muhammed Amin FRCP to semester 4 students of the International Medical University, Malaysia (now IMU University), about Limb Weakness (Part 1). Myelopathy - spinal cord lesions.pptx



Myelopathy - spinal cord lesions.pptxJwan AlSofi
╠²
Approach to patient with spinal cord lesions & diseases
Localize spinal cord lesions
Determining the Level of the Lesion in Myelopathy
Diseases of spinal cord
Limb Weakness Part I



Limb Weakness Part IReed O'Brien
╠²
Lecture by Prof. Osama Shukir Muhammed Amin FRCP(Edin), FRCP(Glasg), FRCP(Ire), FRCP(Lond), FACP, FAHA, to consolidate information pre-Task Based Learning about Limb Weakness. This lecture addresses upper motor neuron signs, their localization, and rationale for choosing diagnostic investigations. The next lecture will be about lower motor neuron lesions.Physiology of posture movementand equilibrium



Physiology of posture movementand equilibriumwebzforu
╠²
This document discusses the physiology of posture, movement, and equilibrium. It covers 3 main points:
1. The neural control of posture and movement involves pathways from the cortex, brainstem, and cerebellum that converge on spinal motor neurons. The pyramidal system controls voluntary movement while the extrapyramidal system adjusts posture.
2. Lesions to different parts of the motor control pathways produce distinct deficits, such as loss of fine motor skills from damage to the lateral corticospinal tract. Transections of the spinal cord and brainstem in animals produce characteristic reflexes and rigidity.
3. The brainstem, cerebellum, and vestibular systems work together to maintain equilibrium andParaparesis biplave nams



Paraparesis biplave namsbiplave karki
╠²
1) Paraplegia is defined as impairment of motor function in the lower extremities, which can be caused by lesions in the cerebral cortex, spinal cord, nerves supplying the lower limbs, or muscles directly.
2) Complete paralysis of both lower limbs is known as paraplegia, while partial paralysis is called paraparesis. Lesions that transect motor tracts cause spastic paraplegia or quadriplegia with heightened reflexes.
3) Determining the level and type of spinal cord lesion is important for diagnosis and involves assessing sensory loss, motor weakness, reflex changes, and associated symptoms.paraparesisbiplavenams-190401002135.pdf



paraparesisbiplavenams-190401002135.pdfNamanMishra87
╠²
1) Paraplegia is defined as impairment of motor function in the lower extremities, which can be caused by lesions in the cerebral cortex, spinal cord, nerves supplying the lower limbs, or muscles directly.
2) The document provides details on the causes, features, levels of lesions, and approaches to examining a patient with paraplegia. Common causes include trauma, tumors, tuberculosis, thrombosis, and transverse myelitis.
3) Based on the level and completeness of the spinal cord lesion, the features of paraplegia such as muscle tone, reflexes, and sensory involvement will differ. Determining the level of lesion is important for diagnosing the underlying cause.Localization



LocalizationQamar Zaman
╠²
This document discusses neurological examination and localization of lesions in the nervous system. It describes the steps in neurological diagnosis and provides information on localization of lesions at different levels of the neuraxis from the cortex to muscles. Key signs and symptoms are outlined for upper motor neuron and lower motor neuron lesions, as well as peripheral nerve disorders, neuromuscular junction disorders, and muscle disorders. Specific examination findings that help localize lesions in different parts of the brain, spinal cord, nerves, and neuromuscular junction are also summarized.vnd.openxmlformats-officedocument.presentationml.pdf



vnd.openxmlformats-officedocument.presentationml.pdfRoop
╠²
This document describes several descending tracts that control motor activity from the brain through the spinal cord. It discusses the origin, course, decussation, destination, function, and clinical implications of major tracts including the pyramidal, corticobulbar, corticospinal, corticorubrospinal, reticulospinal, tectospinal, and vestibulospinal tracts. Clinical conditions resulting from lesions in these tracts like upper motor neuron syndrome, pseudobulbar palsy, decerebrate and decorticate rigidity are also explained.Spasticity



SpasticitySurbhiChaturvedi10
╠²
This document provides an overview of spasticity including:
- Definitions of spasticity and tone as the continuous partial contraction of muscles at rest.
- Pathophysiology involving an imbalance between excitatory and inhibitory signals to motor neurons due to lack of descending inhibition.
- Characteristics including increased resistance to passive movement and hyperactive stretch reflexes.
- Factors that can aggravate spasticity like pain, stress, and infection.
- A spectrum of care including oral drugs, rehabilitation, intrathecal baclofen, and neurosurgery to manage spasticity based on individual needs.Tone new



Tone newdr debasish hota
╠²
Muscle tone is the baseline tension present in muscles even when at rest. It is controlled by both spinal and supra-spinal mechanisms. At the spinal level, muscle tone is regulated by the stretch reflex involving muscle spindles, alpha and gamma motoneurons. Supra-spinally, various descending pathways from the brainstem and cortex facilitate or inhibit muscle tone. Abnormalities in muscle tone include hypertonia (spasticity or rigidity) and hypotonia. Spasticity results from upper motor neuron lesions and involves exaggerated stretch reflexes. Rigidity occurs in extrapyramidal conditions and is speed-independent. Hypotonia is decreased muscle tone. Clinical examination of tone involves assessing resistance to passive movementlocalization of disorders in neurosurgery .pptx



localization of disorders in neurosurgery .pptxSaujanya Jung Pandey
╠²
how to localize in neurological disorderslocalization of disorders in neurosurgery .pptx



localization of disorders in neurosurgery .pptxSaujanya Jung Pandey
╠²
how to localize in neurological disordersLimb Weakness (Part II), spinal cord to muscles



Limb Weakness (Part II), spinal cord to musclesJeremy McCool
╠²
A lecture given by Prof. Dr. Osama Shukir Muhammed Amin FRCP to semester 4 students of the International Medical University, Malaysia (now IMU University), about Limb Weakness (Part 1). Motor System (Neurology 1)



Motor System (Neurology 1)Dr. Alok Kumar
╠²
The document describes the examination and assessment of the motor system. It discusses the motorpyramidal system, which includes neurons in the cortex and anterior horn of the spinal cord. The examination involves assessing body position, gait, muscle inspection and palpation, reflexes, tone, and strength. Various types of paralysis or paresis are defined based on the number of limbs or parts of the body affected. Central paresis symptoms include muscle hypertension, decreased force, hyperreflexia, clonus, and pathological reflexes. Lesions in different parts of the motor system cause distinct patterns of weakness, including hemispheric, brainstem, spinal cord, nerve root and peripheral nerve lesions.Gangguan motorik, appetizer ;)



Gangguan motorik, appetizer ;)Ersifa Fatimah
╠²
Banyak pasien neuro dengan keluhan gangguan motorik, terutama kelemahan anggota badan. Tapi ternyata gangguan motorik tu nggak cuma "parese" aja.. ada banyak macemnya! (Ada yg pernah bikin stats-nya??)
File ini cuma menceritakan sekelumit tentang gangguan motorik, dan si desainer ppt ini pun cuma sempet baca sedikit. Tapi dari yang sedikit ini, rasanya bikin pengen belajar lebih banyak lagi! (karena itu dikasi subtitle "Appetizer"..)
Menarik banget cerita tentang jenis2 gangguan motorik ini, lokasi lesi-nya, ciri2 khususnya, n penyebabnya..
Oia, insyaAllah ppt ini akan selalu dilengkapi & diupdate sesuai referensi yg sanggup dibaca si desainer^^v
(Tugas modul ini pun digarap dengan sangat senang hati, hehehehe..)Recently uploaded (20)
Restoring Remission in RRMM: Present and Future of Sequential Immunotherapy W...



Restoring Remission in RRMM: Present and Future of Sequential Immunotherapy W...PVI, PeerView Institute for Medical Education
╠²
Chair, Shaji K. Kumar, MD, and patient Vikki, discuss multiple myeloma in this CME/NCPD/AAPA/IPCE activity titled ŌĆ£Restoring Remission in RRMM: Present and Future of Sequential Immunotherapy With GPRC5D-Targeting Options.ŌĆØ For the full presentation, downloadable Practice Aids, and complete CME/NCPD/AAPA/IPCE information, and to apply for credit, please visit us at https://bit.ly/4fYDKkj. CME/NCPD/AAPA/IPCE credit will be available until February 23, 2026.Macafem Reviews 2024 - Macafem for Menopause Symptoms



Macafem Reviews 2024 - Macafem for Menopause SymptomsMacafem Supplement
╠²
At Macafem, we provide 100% natural support for women navigating menopause. For over 20 years, we've helped women manage symptoms, and in 2024, we're proud to share their heartfelt experiences.Restoring Remission in RRMM: Present and Future of Sequential Immunotherapy W...



Restoring Remission in RRMM: Present and Future of Sequential Immunotherapy W...PVI, PeerView Institute for Medical Education
╠²
Chair, Shaji K. Kumar, MD, prepared useful Practice Aids pertaining to multiple myeloma for this CME/NCPD/AAPA/IPCE activity titled ŌĆ£Restoring Remission in RRMM: Present and Future of Sequential Immunotherapy With GPRC5D-Targeting Options.ŌĆØ For the full presentation, downloadable Practice Aids, and complete CME/NCPD/AAPA/IPCE information, and to apply for credit, please visit us at https://bit.ly/4fYDKkj. CME/NCPD/AAPA/IPCE credit will be available until February 23, 2026.Advancements in IgA Nephropathy: Discovering the Potential of Complement Path...



Advancements in IgA Nephropathy: Discovering the Potential of Complement Path...PVI, PeerView Institute for Medical Education
╠²
Co-Chairs and Presenters, Gerald Appel, MD, and Dana V. Rizk, MD, discuss kidney disease in this CME activity titled ŌĆ£Advancements in IgA Nephropathy: Discovering the Potential of Complement Pathway Therapies.ŌĆØ For the full presentation, downloadable Practice Aids, and complete CME information, and to apply for credit, please visit us at https://bit.ly/48UHvVM. CME credit will be available until February 25, 2026.IMMUNO-ONCOLOGY DESCOVERING THE IMPORTANCE OF CLINICAL IMUNOLOGY IN MEDICINE



IMMUNO-ONCOLOGY DESCOVERING THE IMPORTANCE OF CLINICAL IMUNOLOGY IN MEDICINERelianceNwosu
╠²
This presentation emphasizes the role of immunodiagnostics and Immunotherapy. psychosomaticdisorder and it's physiotherapy management



psychosomaticdisorder and it's physiotherapy managementDr Shiksha Verma (PT)
╠²
Psychosomatic disorder Public health 101 x health disinformation.pptx



Public health 101 x health disinformation.pptxTina Purnat
╠²
Public health approaches to health disinformation E Book Daniya Sanal.pdf#healthy books.com



E Book Daniya Sanal.pdf#healthy books.comDaniyaSanal
╠²
good health for good life good heart for safe and secure life..the good quality of life will makes good and #haelthy vibes...Neurologic Manifestations of Infective Endocarditis.pptx



Neurologic Manifestations of Infective Endocarditis.pptxdribnibrahem164
╠²
neurological complications of infective endocarditisCOLD PCR application used in breast cancer research



COLD PCR application used in breast cancer researchSona Thesis Consultancy
╠²
COLD-PCR is a modified version of the polymerase chain reaction (PCR) technique used to selectively amplify and enrich rare or minority DNA sequences, such as mutations or genetic variations. Powerpoint presentation about the influence of cultural and helath belief sys...



Powerpoint presentation about the influence of cultural and helath belief sys...JessakinNaron
╠²
study about the influence of cultural and health belief system on health care practiceStrategies for Promoting Innovation in Healthcare Like Akiva Greenfield.pdf



Strategies for Promoting Innovation in Healthcare Like Akiva Greenfield.pdfakivagreenfieldus
╠²
Healthcare innovation has been greatly aided by leaders like Akiva Greenfield, CEO of Nexus, particularly in fields like operational efficiency, revenue cycle management (RCM), and client engagement. In order to ensure both operational success and better patient experiences, Akiva's approach combines technological advancements with an emphasis on improving the human side of healthcare.
Union Budget 2025 Healthcare Sector Analysis & Impact (PPT).pdf



Union Budget 2025 Healthcare Sector Analysis & Impact (PPT).pdfAditiAlishetty
╠²
The Union Budget 2025-26 emphasizes enhancing India's healthcare by allocating Ōé╣99,858 crore to the Ministry of Health and Family Welfare, marking a 10% increase from the previous year. Key initiatives include adding 10,000 medical college seats, with a plan to reach 75,000 over five years, and increasing funding for the Pradhan Mantri Ayushman Bharat Health Infrastructure Mission by 41% to Ōé╣4,758 crore. However, experts express concerns that the allocation may still fall short of the sector's urgent needs. Dr. Bipin Vibhute, a distinguished Liver and Multi-Organ Transplant Surgeon, is renowned for pioneering free liver transplants for pediatric patients up to 12 years old in Pune. As the Program Director of the Center for Organ Transplants at Sahyadri Hospitals, he has significantly advanced organ transplantation services across Maharashtra.Pulse and affecting factors.pptx Vital Sign



Pulse and affecting factors.pptx Vital SignProf. (Dr.) Rahul Sharma
╠²
Dicrotic pulse pulse
nursing foundation
pulse rate
affecting factor of pulse
pulse introduction
site of pulse
characteristics of pulse
Rate
Rhythm
Tension
Volume
Tachycardia
Bradycardia
Arrhythmias
Intermittent pulse
Extrasystoles
Atrial fibrillation
Ventricular fibrillation
Sinus arrhythmiaResearch Problems - Nursing Research....



Research Problems - Nursing Research....Dr. Binu Babu Nursing Lectures Incredibly Easy
╠²
Research Problems - Nursing ResearchResearch Hyopthesis and Research Assumption



Research Hyopthesis and Research AssumptionDr. Binu Babu Nursing Lectures Incredibly Easy
╠²
Research Hyopthesis and Assumptiondelayed recovery of anaesthesia ppt. delayed



delayed recovery of anaesthesia ppt. delayedSimmons2
╠²
delayed recovery from anaesthesia
#anaesthesia#delayed recoveryFAO's Support Rabies Control in Bali_Jul22.pptx



FAO's Support Rabies Control in Bali_Jul22.pptxWahid Husein
╠²
What is FAO doing to support rabies control programmes in Bali, Indonesia, using One Health approach with mass dog vaccination and integrated bite case management as main strategieslegal Rights of individual, children and women.pptx



legal Rights of individual, children and women.pptxRishika Rawat
╠²
A legal right is a claim or entitlement that is recognized and protected by the law. It can also refer to the power or privilege that the law grants to a person. Human rights include the right to life and liberty, freedom from slavery and torture, freedom of opinion and expression, the right to work and educationRestoring Remission in RRMM: Present and Future of Sequential Immunotherapy W...



Restoring Remission in RRMM: Present and Future of Sequential Immunotherapy W...PVI, PeerView Institute for Medical Education
╠²
Restoring Remission in RRMM: Present and Future of Sequential Immunotherapy W...



Restoring Remission in RRMM: Present and Future of Sequential Immunotherapy W...PVI, PeerView Institute for Medical Education
╠²
Advancements in IgA Nephropathy: Discovering the Potential of Complement Path...



Advancements in IgA Nephropathy: Discovering the Potential of Complement Path...PVI, PeerView Institute for Medical Education
╠²
Clinical aspects of upper and lower motor neuron lesions
- 1. ŌĆ£Clinical Aspects of Upper and Lower Motor Neuron LesionsŌĆØ Osama Shukir Muhammed Amin MBChB, MD, MRCP, FACP, FAHA, FCCP(USA), FRCP(Edin), FRCP(Glasg), FRCP(Ire), FRCP(Lond) Associate Professor of Neurology School of Medicine, International Medical University, Malaysia
- 3. Left corticospinal tract: Note the origin and journey!
- 4. Function of the cortico-spinal (pyramidal) tracts? The cortico-spinal tract is involved in the volitional activity of skeletal muscle movements of the contralateral side. ŌĆó Upper limbs: shoulder abduction, as well as elbow, wrist, and fingers extensions. ŌĆó Lower limbs: hip and knee flexion, as well as ankle dorsi-flexion and planter eversion. Antigravity muscles and movements?
- 5. Note: These movements are further controlled/modulated by the extrapyramidal and cerebellar systems, with respect to initiation, coordination, speed, tone, etc.
- 6. Lesion(s) of a cortico-spinal tract? ŌĆó This would result in loss of function of that tract with secondary dominance of extrapyramidal and other tractsŌĆÖ functions; e.g., rubrospinal, vestibulospinal, tectospinal, etc. ŌĆó The resulting clinical features depend on the etiology of the lesion, onset, severity, multiplicity, and association with other lesions within and outside the CNS (i.e., peripheral nervous system).
- 7. Pyramidal system damage would result inŌĆ”? ŌĆó Weakness or paresis of the targeted movement (there is no complete paralysis). Monoparesis, hemiparesis, or quadriparesis. ŌĆó Reduced control of volitional movements, especially of distal fine dexterity; e.g., buttoning and unbuttoning. ŌĆó Hypertonia of clasp-knife spasticity and ŌĆ£sustainedŌĆØ clonus. ŌĆó Exaggerated deep tendon reflexes. ŌĆó Extensor planter reflex (Babinski sign), Hoffman sign, pronator drift, etc. ŌĆó No or very minimal atrophy. Disuse atrophy occurs in longstanding cases.
- 8. That is to say: Signs of upper motor neuron lesion! And, this reflects what? Any lesion from the cerebral cortex down to the anterior horn cells of the spinal cord!
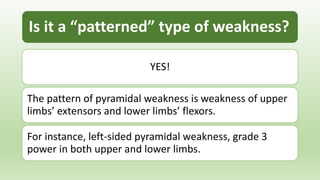
- 9. Is it a ŌĆ£patternedŌĆØ type of weakness? YES! The pattern of pyramidal weakness is weakness of upper limbsŌĆÖ extensors and lower limbsŌĆÖ flexors. For instance, left-sided pyramidal weakness, grade 3 power in both upper and lower limbs.
- 10. Note the origin, course, and target of lower motor neurons!
- 11. Lower motor neuron lesionsŌĆÖ signs? The classical signs are: ’ā╝Weakness or complete paralysis. ’ā╝Hypotonia (flaccidity). ’ā╝Hyporeflexia or areflexia. ’ā╝Fasciculation (involuntary rippling muscle movements). ’ā╝Early and prominent atrophy.
- 12. Such signs would reflect what? Any lesion from the spinal cordŌĆÖs ventral horn alpha motor neurons down to the muscle fibers (i.e., a long pathway).
- 13. How would they present clinically? The presentation depends on the etiology, site of the lesion, multiplicity of the lesion, onset, and progression. And, if there is any coexistent central nervous system damage.
- 14. Where, localize? ŌĆóSpinal cord anterior ventral horn lesions. ŌĆóRadiculopathy. ŌĆóPlexopathy. ŌĆóMotor-end plate diseases. ŌĆóMyopathy/myositis. PS: Each of them depicts a unique constellation of symptoms and signs.
- 15. Rock relief of king Naram-Sin (beloved of moon god Sin), Mountain Qaradagh, Iraq. Circa 2200 BCE. Photo ┬® Osama S. M. Amin.

