clinical aspects of vein
- 1. Clinical aspects of vein Presented by: ANKITA MISHRA 16
- 2. Clinical anatomy of vein Anatomy of the venous system of the leg DEEP VEINS POSTERIOR TIBIAL ANTERIOR TIBIAL PERONEAL ` SOLEAL GASTROC NEMIUS POPLITEAL FEMORAL ILIAC SUPERFICIAL VEINS LONG SAPHENOUS (LSV) SHORT SAPHENOUS (SSV)
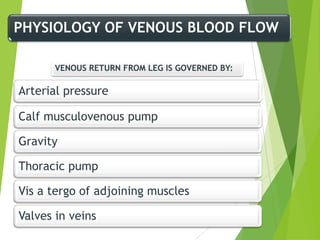
- 3. PHYSIOLOGY OF VENOUS BLOOD FLOW VENOUS RETURN FROM LEG IS GOVERNED BY: Arterial pressure Calf musculovenous pump Gravity Thoracic pump Vis a tergo of adjoining muscles Valves in veins
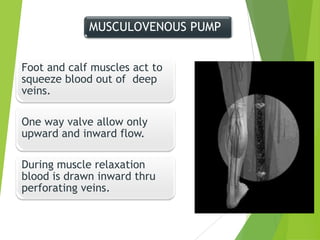
- 4. MUSCULOVENOUS PUMP Foot and calf muscles act to squeeze blood out of deep veins. One way valve allow only upward and inward flow. During muscle relaxation blood is drawn inward thru perforating veins.
- 5. VENOUS VALVULAR FUNCTION VALVE LEAFLETS ALLOW UNIDIRECTIONAL FLOW UPWARD OR INWARD. ŌĆ£NONREFLUXING OF VALVESŌĆØ MAJOR VALVES-OSTIAL VALVE PRETERMINAL VALVE
- 6. PATHOPHYSIOLOGY Primary muscle pump failure Venous obstruction Venous valvular incompetance: 1.perforator incompetence-hydrodynamic reflux 2.sup.vein incompetence- hydrostatic reflux 3.deep vein incompetence- isolated/2┬░
- 7. Vein Disorders Venous Thrombosis (Superficial and Deep Vein Thrombosis), Thrombophlebitis Chronic Venous Insufficiency Varicose Veins
- 8. Chronic Venous Insufficiency Results from obstruction of venous valves in legs or reflux of blood back through valves Venous ulceration is serious complication Pharmacological therapy is antibiotics for infections Debridement to promote healing Topical Therapy may be used with cleansing and debridement
- 9. Stages of chronic venous insufficiency 0 - no symptoms; 1 - heavy feet syndrome; 2 - intermittent edema; 3 - persistent edema, hyper- or hypopigmentation, lipodermatosclerosis, eczema; 4 - venous ulcer.
- 10. Causes Primary Theories of Aetiology: ŌĆó Weak wall theory ŌĆó Congenital valvular incompetence Aggravating factors: ŌĆó Female sex ŌĆó High parity ŌĆó Occupation requiring prolonged standing ŌĆó Marked obesity ŌĆó Constricting clothes ŌĆó Estrogen intake ŌĆó Deep venous thrombosis
- 11. Secondary Anything that raises intra-abdominal pressure or raises pressure in superficial/deep venous system soŌĆ”: ŌĆóPregnancy ŌĆóAbdominal/pelvic mass ŌĆóAscites ŌĆóobesity ŌĆóconstipation ŌĆóthrombosis of leg veins (DVT) ŌĆóAV fistula ŌĆóVena cava thrombose ŌĆóLarge liver cysts
- 12. Varicose disease Varicose disease of subcutaneous veins is their irreversible dilation and elongation occurring due to crude pathological change of venous walls and valvular apparatus.
- 13. ANY RISK FACTOR INCREASED VENOUS PRESSURE DILATION OF VEIN WALLS STRECHING OF VALVES-VALVULAR INCOMPETENCE REVERSAL OF BLOOD FLOW FAILURE OF MUSCLES TO PUMP BLOOD VEINS DISTEND,ELONGATE,TORTOUS,POUCHED,INELASTIC AND FRIABLE
- 14. Surgical Intervention INDICATED OR DONE FOR PREVENTION OR RELIEF OF EDEMA, FOR RECURRENT LEG ULCERS OR PAIN OR FOR COSMETIC PURPOSES VEIN LIGATION AND STRIPPING THE GREAT SAPHENEOUS VEIN IS LIGATED (TIED) CLOSE TO THE FEMORAL JUNCTION THE VEINS ARE STRIPPED OUT THROUGH SMALL INCISIONS AT THE GROIN, ABOVE & BELOW THE KNEE AND AT THE ANKLES. STERILE DRESSING ARE PLACED OVER THE INCISIONS AND AN ELASTIC BANDAGE EXTENDING FROM THE FOOT TO THE GROIN IS FIRMLY APPLIED
- 15. NURSING CARE AFTER VEIN LIGATION & STRIPPING Keep pt. flat on bed for first 4 hrs. after surgery, elevate leg to promote venous return when lying or sitting Medicate 30 mins. before ambulation and assist patient Keep elastic bandage snug and intact, do not remove bandage Monitor for signs of bleeding, esp. on 1st post-op day if there is bleeding, elevate the leg, apply pressure over the wound and notify the surgeon
- 19. RISK FACTORS Age Gender Height left>right Heredity Pregnancy Obesity and overweight Posture
- 20. ’é¦ 25-50% of adult women ’é¦ 15-30% of adult men Is it an industrialized country disease? UK: 45 000 hospital admissions per year
- 21. Treatment complications Major complications following VV surgery are relatively rare Up to 20% morbidity Infection Hematoma Pain Nerve damage Saphenous nerve (LSV surgery) Sural, peroneal nerve (SSV surgery) Lymphatic leak - Venous thrombosis - Vascular injury Recurrence
- 22. Deep Vein Thrombosis (DVT) DVT: Blood clot in a vein located deep in the muscles of the legs, thighs, pelvis or arms DVT is the result of 3 principle factors 1. Reduce or stagnant blood flow in deep veins 2. Injury to the blood vessels wall 3. Increase clotting activity (hyper-coagulability 22 or thrombophilia)
- 23. Risk of DVT 1. Immobilization 2. Recent surgery or trauma 3. The use of medication 4. Inherited or acquired hypercoagulability, Note: Approximately 75-90% of DVT have at least one established risk factor : Inherited thrombophilias can be identified in 24-37% of patients 23
- 24. SIGN AND SYMPTOMS Leg pain or tenderness Leg swelling Increase wormth of one leg,change in skin color (redness) Homans sign positive 24
- 25. Medical Management Deep vein thrombosis ’üČREQUIRES HOSPITALIZATION ’üČBED REST W/ LEGS ELEVATED TO 15-20 DEGREES ABOVE HEART LEVEL ( KNEES SLIGHTLY FLEXED, TRUNK HORIZONTAL (HEAD MAY BE RAISED) TO PROMOTE VENOUS RETURN AND HELP PREVENT FURTHER EMBOLI AND PREVENT EDEMA ’üČAPPLICATION OF WARM MOIST HEAT TO REDUCE PAIN, PROMOTES VENOUS RETURN ’üČELASTIC STOCKING OR BANDAGE ’üČANTICOAGULANTS, INITIALLY WITH IV HEPARIN THEN COUMADIN ’üČFIBRINOLYTIC TO RESOLVE THE THROMBUS ’üČVASODILATOR IF NEEDED TO CONTROL VESSEL SPASM AND IMPROVE CIRCULATION
- 26. Nursing Assessment ’üČcharacteristic of the pain ’üČonset & duration of symptoms ’üČhistory of thrombophlebitis or venous disorders ’üČcolor & temp. of extremity ’üČedema of calf of thigh - use a tape measure, measure both legs for comparison ’üČIdentify areas of tenderness and any thrombosis SURGERY ’üČif the thrombus is recurrent and extensive or if the pt. is at high risk for pulmonary embolism ’üČThrombectomy ŌĆō incising the common femoral vein in the groin and extracting the clots ’üČVena caval interruption ŌĆō transvenous placement of a grid or umbrella filter in the vena cava to block the passage of emboli
- 27. Thrombophlebitis ’üČinflammation of the veins caused by thrombus or blood clot Factors assoc. with the devt. of Thrombophlebitis ’üČvenous stasis ’üČdamage to the vessel wall ’üČhypercoagulability of the blood ŌĆō oral contraceptive use ’üČcommon to hospitalized pts. , undergone major surgery (pelvic or hip surgery), MI Pathophysiology ’üČdevelops in both the deep and superficial veins of the lower extremity ’üČdeep veins ŌĆō femoral, popliteal, small calf veins ’üČsuperficial veins ŌĆō saphenous vein ’üČThrombus ŌĆō form in the veins from accumulation of platelets, fibrin, WBC and RBC
- 28. Thrombophlebitis ŌĆóThrombosis with infammation of superfiacial veins ŌĆóOccur spontaneously/due to minor trauma ŌĆóCan occur durin injection of sclerosing fluid for treatment
- 29. Main symptoms of thrombophlebitis Edema of the extremity The pains are localised in the gastrocnemius muscles as a rule, along the course of vascular bundles The skin of the extremity becomes cyanotic.
- 30. Medical Management Thrombophlebitis ’üČbed rest with legs elevated ’üČapply moist heat ’üČNSAIDŌĆÖs ( Non ŌĆō steroidal anti-inflammatory drugs) - aspirin
- 31. Homans' sign ŌĆó Pains in gastrocnemius muscle upon dorsal flexing of the foot is characteristic of thrombophlebitis of profound veins of the extremity.
- 32. Classification of functional tests 1. Test enable one to judge the condition of valvular apparatus Trendelenburg-Trojanov's tests Hackenbruch's 2. Test enable of insufficient perforating veins Pratt's test II Scheins' test Thalmann's test 3. Test enable the patency of profound veins Delbe-Pertez test (marching test) Pratt-I test
- 34. Pratt's test II.
- 36. Scheins' test.
- 37. Delbe-Pertez test (marching test)
- 39. Thrombectomy from femoral vein
- 41. Edema