controle of cardiac output regulation.ppt
- 1. + Control Of Cardiac Output By Manpreet & Olivia
- 2. + Introduction ’ü« Terminology ’ü« Components of stroke volume ’ü« Cardiac cycle ’ü« Pressure-volume loops ’ü« Frank-Starling mechanism ’ü« Factors affecting CO
- 3. + Terminology Cardiac Output ’ü« => ŌĆśvolume of blood pumped by each ventricle per minuteŌĆÖ ’ü« Measured - litres per minute. ’ü« CO = SV X HR Stroke volume ’ü« =>ŌĆØ The volume of blood ejected from each ventricle during each ventricle contractionŌĆØ ’ü« SV = End diastolic volume ŌĆō End systolic volume ’ü« Affected by: contractility, afterload & preload [SV CAP] ’ü« E.g SV increases when: increase contractility, increased preload, decreased afterload. ’ü« SV increases in anxiety, exercise and pregnancy ’ü« Heart failure has decreased SV
- 4. + Preload & Afterload ’ü« Preload ’ü« Preload approximated by ventricular EDV ’ü« Dependent on venous tone and circulating blood volume ’ü« VEnodilators (e.g nitroglycerin) decrease preEload ’ü« Afterload ’ü« Afterload approximated by MAP ’ü« Affected by Wall tension ’ü« Increased afterload -> LV compensates by thickening (hypertrophy) ’ü« Chronic hypertension (increased MAP) -> LV hypertrophy ’ü« VAsodilators decrease Afterload (Atrial) ’ü« ACEi + ARBs decrease both preload and afterload
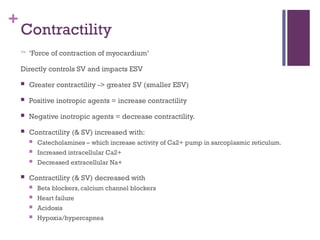
- 5. + Contractility ’ā× ŌĆśForce of contraction of myocardiumŌĆÖ Directly controls SV and impacts ESV ’ü« Greater contractility -> greater SV (smaller ESV) ’ü« Positive inotropic agents = increase contractility ’ü« Negative inotropic agents = decrease contractility. ’ü« Contractility (& SV) increased with: ’ü« Catecholamines ŌĆō which increase activity of Ca2+ pump in sarcoplasmic reticulum. ’ü« Increased intracellular Ca2+ ’ü« Decreased extracellular Na+ ’ü« Contractility (& SV) decreased with ’ü« Beta blockers, calcium channel blockers ’ü« Heart failure ’ü« Acidosis ’ü« Hypoxia/hypercapnea
- 8. + ’ü« => ŌĆśability of the heart to change its force of contraction and therefore SV in response to changes in venous returnŌĆÖ ’ü« As blood returns to the heart in diastole, ventricle fills so volume increases and intra-ventricular pressure also progressively rise Frank-Starling Mechanism ’ü« Myocardial fibres in the ventricular wall are stretched and put under tension (preload) ’ü« Cardiac muscle responds to increased stretch with a more forceful contraction
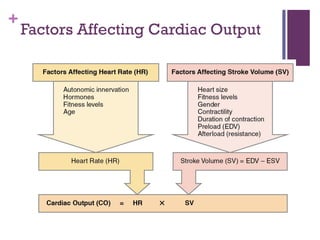
- 9. + Factors Affecting Cardiac Output
- 10. + Factors Decreasing Heart Rate and Force of Contraction Factor Effect Cardioinhibitor nerves (vagus) Release of acetylcholine Proprioreceptors Decreased rates of firing following exercise Chemoreceptors Increased levels of O2; decreased levels of H+ and CO2 Baroreceptors Increased rates of firing, indicating higher blood volume/pressure Limbic system Anticipation of relaxation Catecholamines Decreased epinephrine and norepinephrine Thyroid hormones Decreased T3 and T4 Calcium Decreased Ca2+ Potassium Increased K+ Sodium Increased Na+ Body temperature Decrease in body temperature Decreasing HR
- 11. + Increasing HR Major Factors Increasing Heart Rate and Force of Contraction Factor Effect Cardioaccelerator nerves Release of norepinephrine Proprioreceptors Increased rates of firing during exercise Chemoreceptors Decreased levels of O2; increased levels of H+, CO2, and lactic acid Baroreceptors Decreased rates of firing, indicating falling blood volume/pressure Limbic system Anticipation of physical exercise or strong emotions Catecholamines Increased epinephrine and norepinephrine Thyroid hormones Increased T3 and T4 Calcium Increased Ca2+ Potassium Decreased K+ Sodium Decreased Na+ Body temperature Increased body temperature Nicotine and caffeine Stimulants, increasing heart rate
- 12. + Summary Table: Factors Affecting SV
Editor's Notes
- Normal CO approx 5L End diastolic volume = amount of blood in the ventricles (maximum) End systolic volume = amount of blood remaining in the ventricles after it has contracted (normally a very small amount) EDV ŌĆō ESV = amount of blood the ventricles are pumping out to the body
- MAP = 2/3 diastolic pressure + 1/3 systolic pressure
- S1 ŌĆō mitral and tricupsid valve closure. Loudest at mitral area S2 ŌĆō aortic and pulmonary valve closure. Loudest at left sternal border S3 ŌĆō in early diastole during rapid ventricular filling phase. Associated with increased filling pressures (e.g. mitral regurg, CHF) and more common in dilated ventricles (but normal in children and pregnant women) S4 ŌĆō (ŌĆśatrial kickŌĆÖ) ŌĆō in late diastole. High atrial pressure. Associated with entricular hypertrophy. Left atrium must push against stiff LV wall.
- Phases: A ŌĆō ventricular filling, diastole B ŌĆō isovolumetric contraction, systole (mitral valve closes and the ventricle begins to contract, LVP increases) it is the period of highest oxygen consumption C ŌĆō ejection, systole (LV volume decreases as LVP reaches its peak and then decreases as the ventricle begins to relax) D ŌĆō isovolumetric relaxation, diastole Points: 1 ŌĆō pressure and volume at the end of diastole (EDPVR) 2 ŌĆō LVP has exceeded aortic diastolic pressure leading to the opening of the aortic valve and ejection to begin. 3 ŌĆō aortic valve closes, ejection stops and isovolumetric relaxation begins, LVP falls but LV stays the same as all valves are closed at this time 4 ŌĆō when the LVP falls below atrial pressure, the mitral valve opens and ventricle begins to fill
- Frank-starling mechanism is essentially stating that SV is proportional to preload within the normal physiological range. So normally as preload increases, so does SV. In HF ventricular filling is impaired so SV is reduced and there is poor contractility of the ventricle


![+
Terminology
Cardiac Output
’ü« => ŌĆśvolume of blood pumped by each ventricle per minuteŌĆÖ
’ü« Measured - litres per minute.
’ü« CO = SV X HR
Stroke volume
’ü« =>ŌĆØ The volume of blood ejected from each ventricle during each ventricle
contractionŌĆØ
’ü« SV = End diastolic volume ŌĆō End systolic volume
’ü« Affected by: contractility, afterload & preload [SV CAP]
’ü« E.g SV increases when: increase contractility, increased preload, decreased
afterload.
’ü« SV increases in anxiety, exercise and pregnancy
’ü« Heart failure has decreased SV](https://image.slidesharecdn.com/5789329-241206171838-df7eac19/85/controle-of-cardiac-output-regulation-ppt-3-320.jpg)