Depression in elderly
- 2. Presentation Outline âĒ Definition âĒ Introduction âĒ Epidemiology âĒ Causes and Risk Factors âĒ Diagnosis âĒ Approach âĒ Screening âĒ Differential diagnosis âĒ Treatment âĒ Prognosis
- 3. Definition Depression âĒ A spectrum of mood disorders characterized by a sustained disturbance in emotional, cognitive, behavioral, or somatic regulation and associated with significant functional impairment and a reduction in the capacity for pleasure and enjoyment
- 4. INTRODUCTION âĒ Depression in older adults is a widespread problem, âĒ but it is not a normal part of aging. âĒ It is often not recognized or treated.
- 5. What are the differences between older and younger persons with mental illness? âĒ Assessment is different: e.g. cognitive assessment needed, recognize sensory impairments, allow more time âĒ Symptoms of disorders may be different: e.g. different symptoms in depression âĒ Treatment is different: e.g. different doses of meds, different psychotherapeutic approaches âĒ Outcome may be different: e.g. psychopathology in schizophrenia may improve with age
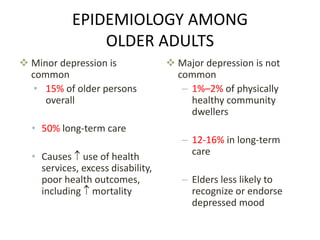
- 6. EPIDEMIOLOGY AMONG OLDER ADULTS ïķ Minor depression is common âĒ 15% of older persons overall âĒ 50% long-term care âĒ Causes ï use of health services, excess disability, poor health outcomes, including ï mortality ïķ Major depression is not common â 1%â2% of physically healthy community dwellers â 12-16% in long-term care â Elders less likely to recognize or endorse depressed mood
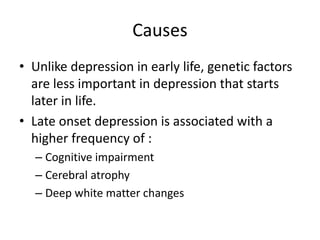
- 10. Causes âĒ Unlike depression in early life, genetic factors are less important in depression that starts later in life. âĒ Late onset depression is associated with a higher frequency of : â Cognitive impairment â Cerebral atrophy â Deep white matter changes
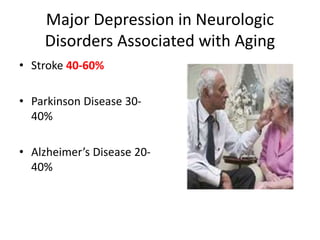
- 11. Major Depression in Neurologic Disorders Associated with Aging âĒ Stroke 40-60% âĒ Parkinson Disease 30- 40% âĒ Alzheimerâs Disease 20- 40%
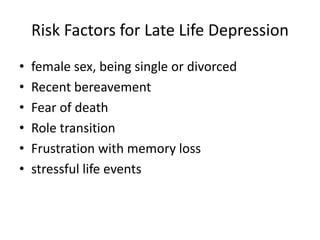
- 12. Risk Factors for Late Life Depression âĒ female sex, being single or divorced âĒ Recent bereavement âĒ Fear of death âĒ Role transition âĒ Frustration with memory loss âĒ stressful life events
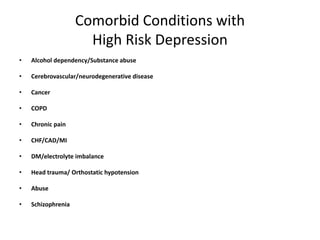
- 13. Comorbid Conditions with High Risk Depression âĒ Alcohol dependency/Substance abuse âĒ Cerebrovascular/neurodegenerative disease âĒ Cancer âĒ COPD âĒ Chronic pain âĒ CHF/CAD/MI âĒ DM/electrolyte imbalance âĒ Head trauma/ Orthostatic hypotension âĒ Abuse âĒ Schizophrenia
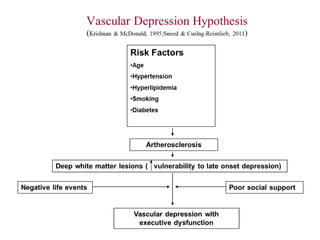
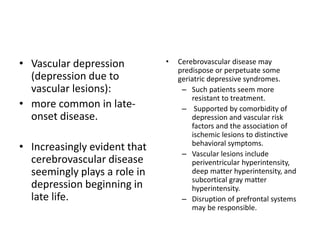
- 15. âĒ Vascular depression (depression due to vascular lesions): âĒ more common in late- onset disease. âĒ Increasingly evident that cerebrovascular disease seemingly plays a role in depression beginning in late life. âĒ Cerebrovascular disease may predispose or perpetuate some geriatric depressive syndromes. â Such patients seem more resistant to treatment. â Supported by comorbidity of depression and vascular risk factors and the association of ischemic lesions to distinctive behavioral symptoms. â Vascular lesions include periventricular hyperintensity, deep matter hyperintensity, and subcortical gray matter hyperintensity. â Disruption of prefrontal systems may be responsible.
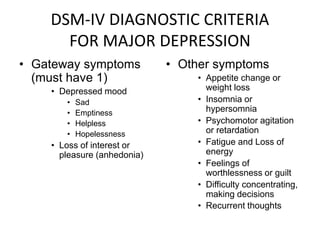
- 16. DSM-IV DIAGNOSTIC CRITERIA FOR MAJOR DEPRESSION âĒ Gateway symptoms (must have 1) âĒ Depressed mood âĒ Sad âĒ Emptiness âĒ Helpless âĒ Hopelessness âĒ Loss of interest or pleasure (anhedonia) âĒ Other symptoms âĒ Appetite change or weight loss âĒ Insomnia or hypersomnia âĒ Psychomotor agitation or retardation âĒ Fatigue and Loss of energy âĒ Feelings of worthlessness or guilt âĒ Difficulty concentrating, making decisions âĒ Recurrent thoughts
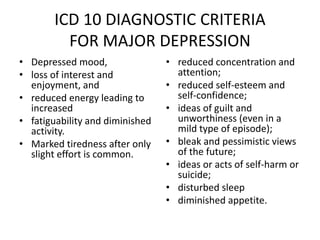
- 17. ICD 10 DIAGNOSTIC CRITERIA FOR MAJOR DEPRESSION âĒ Depressed mood, âĒ loss of interest and enjoyment, and âĒ reduced energy leading to increased âĒ fatiguability and diminished activity. âĒ Marked tiredness after only slight effort is common. âĒ reduced concentration and attention; âĒ reduced self-esteem and self-confidence; âĒ ideas of guilt and unworthiness (even in a mild type of episode); âĒ bleak and pessimistic views of the future; âĒ ideas or acts of self-harm or suicide; âĒ disturbed sleep âĒ diminished appetite.
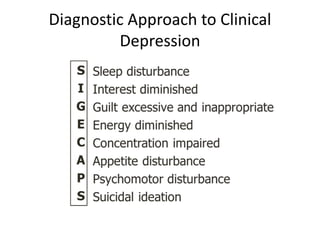
- 18. Diagnostic Approach to Clinical Depression
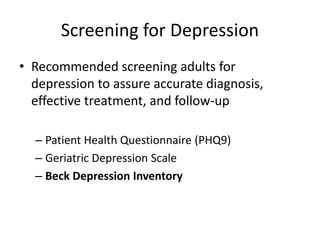
- 19. Screening for Depression âĒ Recommended screening adults for depression to assure accurate diagnosis, effective treatment, and follow-up â Patient Health Questionnaire (PHQ9) â Geriatric Depression Scale â Beck Depression Inventory
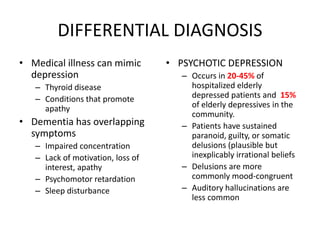
- 20. DIFFERENTIAL DIAGNOSIS âĒ Medical illness can mimic depression â Thyroid disease â Conditions that promote apathy âĒ Dementia has overlapping symptoms â Impaired concentration â Lack of motivation, loss of interest, apathy â Psychomotor retardation â Sleep disturbance âĒ PSYCHOTIC DEPRESSION â Occurs in 20-45% of hospitalized elderly depressed patients and 15% of elderly depressives in the community. â Patients have sustained paranoid, guilty, or somatic delusions (plausible but inexplicably irrational beliefs â Delusions are more commonly mood-congruent â Auditory hallucinations are less common
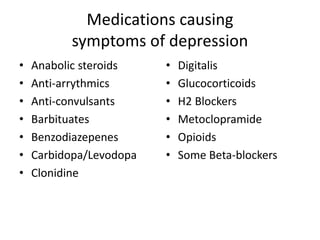
- 21. Medications causing symptoms of depression âĒ Anabolic steroids âĒ Anti-arrythmics âĒ Anti-convulsants âĒ Barbituates âĒ Benzodiazepenes âĒ Carbidopa/Levodopa âĒ Clonidine âĒ Digitalis âĒ Glucocorticoids âĒ H2 Blockers âĒ Metoclopramide âĒ Opioids âĒ Some Beta-blockers
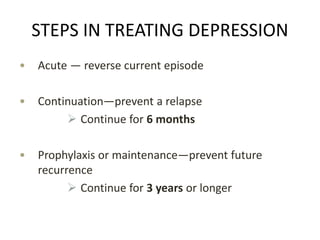
- 22. STEPS IN TREATING DEPRESSION âĒ Acute â reverse current episode âĒ Continuationâprevent a relapse ï Continue for 6 months âĒ Prophylaxis or maintenanceâprevent future recurrence ï Continue for 3 years or longer
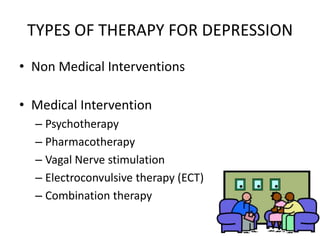
- 23. TYPES OF THERAPY FOR DEPRESSION âĒ Non Medical Interventions âĒ Medical Intervention â Psychotherapy â Pharmacotherapy â Vagal Nerve stimulation â Electroconvulsive therapy (ECT) â Combination therapy
- 25. Thank You