DIABETES GESTASIONAL - PW.pptx
- 1. PW ŌĆō BOARD 47 Diabetes Gestasional
- 3. DIABETES GESTASIONAL ŌĆó DM pada kehamilan dibagi menjadi dua kelompok yaitu : ŌĆó 1) DM yang memang sudah diketahui sebelumnya dan kemudian menjadi hamil (Diabetes Melitus Hamil/ DMH/ DM pragestasional) dan ŌĆó 2) DM yang baru ditemukan saat hamil (Diabetes Melitus Gestasional/ DMG). ŌĆó Diabetes melitus gestasional didefinisikan sebagai suatu intoleransi glukosa yang terjadi atau pertama kali ditemukan pada saat hamil PAPD
- 4. DIABETES GESTASIONAL ŌĆó Pada kehamilan terjadi resistensi insulin fisiologis akibat peningkatan hormon-hormon kehamilan (human placental lactogen/HPL, progesterone, kortisol, prolaktin) yang mencapai puncaknya pada trimester ketiga kehamilan ŌĆó Kegagalan sel beta ini dipikirkan karena beberapa hal diantaranya: ŌĆó 1) autoimun, ŌĆó 2) kelainan genetik dan ŌĆó 3) resistensi insulin kronik. PAPD
- 7. DIABETES GESTASIONAL PAPD ŌĆó Faktor risiko DMG yang dikenal adalah: A. Faktor risiko obstetri ŌĆó Riwayat keguguran beberapa kali ŌĆó Riwayat melahirkan bayi meninggal tanpa sebab ŌĆó jelas ŌĆó Riwayat melahirkan bayi dengan cacat bawaan ŌĆó Riwayat melahirkan bayi >4000 gram ŌĆó Riwayat pre eklamsia ŌĆó Polihidramnion B. Riwayat umum ŌĆó Usia saat hamil >30 tahun ŌĆó Riwayat DM dalam keluarga ŌĆó Riwayat DMG pada kehamilan sebelumnya ŌĆó lnfeksi saluran kemih berulang saat hamil
- 8. TALAKSANA DIABETES GESTASIONAL PAPD ŌĆó Penatalaksanaan harus dimulai dengan terapi nutrisi medik yang diatur oleh ahli gizi. ŌĆó Secara umum, pada trimester pertama tidak diperlukan penambahan asupan kalori. ŌĆó Sedangkan pada ibu hamil dengan berat badan normal secara umum memerlukan tambahan 300 kcal pada trimester kedua dan ketiga. Jumlah kalori yang dianjurkan adalah 30 kcal/berat badan saat hamil. ŌĆó Pada mereka yang obes dengan indeks massa tubuh >30 kg/ m2 maka pembatasan kalori perlu dilakukan yaitu jumlah kalori hanya 25 kcal/ kg berat badan. ŌĆó Asupan karbohidrat sebaiknya terbagi sepanjang hari untuk mencegah ketonemia yang berdampak pada perkembangan kognitif bayi.
- 15. ŌØæ Terapi Nutrisi Medis (TNM) DIABETES GESTASIO NAL PERKENI 2021
- 16. ŌØæ Terapi Nutrisi Medis (TNM) DIABETES GESTASIO NAL PERKENI 2021
- 25. CLASSIFICATION Diabetes can be classified into the following general categories: 1. Type 1 diabetes (due to autoimmune b-cell destruction, usually leading to absolute insulin deficiency, including latent autoimmune diabetes of adulthood) 2. Type 2 diabetes (due to a non-autoimmune progressive loss of adequate b-cell insulin secretion frequently on the background of insulin resistance and metabolic syndrome) 3. Specific types of diabetes due to other causes, e.g., monogenic diabetes syndromes (such as neonatal diabetes and maturity-onset diabetes of the young), diseases of the exocrine pancreas (such as cystic fibrosis and pancreatitis), and drug- or chemical-induced diabetes (such as with glucocorticoid use, in the treatment of HIV/AIDS, or after organ transplantation) 4. Gestational diabetes mellitus (diabetes diagnosed in the second or third trimester of pregnancy that was not clearly overt diabetes prior to gestation) DIABETES TIPE LAIN Diabetes Care Volume 46, Supplement 1, January 2023, ADA
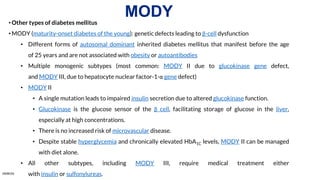
- 26. ŌĆóOther types of diabetes mellitus ŌĆóMODY (maturity-onset diabetes of the young): genetic defects leading to ╬▓-cell dysfunction ŌĆó Different forms of autosomal dominant inherited diabetes mellitus that manifest before the age of 25 years and are not associated with obesity or autoantibodies ŌĆó Multiple monogenic subtypes (most common: MODY II due to glucokinase gene defect, and MODY III, due to hepatocyte nuclear factor-1-╬▒ gene defect) ŌĆó MODY II ŌĆó A single mutation leads to impaired insulin secretion due to altered glucokinase function. ŌĆó Glucokinase is the glucose sensor of the ╬▓ cell, facilitating storage of glucose in the liver, especially at high concentrations. ŌĆó There is no increased risk of microvascular disease. ŌĆó Despite stable hyperglycemia and chronically elevated HbA1C levels, MODY II can be managed with diet alone. ŌĆó All other subtypes, including MODY III, require medical treatment either with insulin or sulfonylureas. MODY AMBOSS
- 27. MODY CATATAN
- 28. ŌĆó MODY is frequently characterized by onset of hyperglycemia at an early age (classically before age 25 years, although diagnosis may occur at older ages). ŌĆó MODY is characterized by impaired insulin secretion with minimal or no defects in insulin action (in the absence of coexistent obesity). It is inherited in an autos MODY Maturity-Onset Diabetes of the Young Diabetes Care Volume 46, Supplement 1, January 2023, ADA
- 29. ŌĆó A diagnosis of one of the three most common forms of MODY, including HFN1AMODY, GCK-MODY, and HNF4A- MODY, allows for more cost-effective therapy (no therapy for GCK-MODY; sulfonylureas as first-line therapy for HNF1A-MODY and HNF4A-MODY). ŌĆó Additionally, diagnosis can lead to identification of other affected family members ŌĆó Positivity for a single antibody should be exclusion criteria for MODY testing. A minimum of three antibodies should be testedŌĆöGAD, IA2 and ZnT8 are preferred. ŌĆó IAA is not widely performed and cannot be used once insulin treatment is given, and ICA antibody testing using primate or rodent pancreatic tissue should not be performed due to a high false-negative rateC- peptide testing to identify and exclude those with absolute insulin deficiency (i.e., urine C-peptide <0.2 nmol/mmol or serum/plasma <200 pmol/L) will further improve selection, but the test has limited use at diagnosis due to the preserved insulin secretion during the honeymoon period and is most useful 3ŌĆō5 years postdiagnosis DIAGNOSIS MODY Maturity-Onset Diabetes of the Young Diabetes Care Volume 46, Supplement 1, January 2023, ADA Medscape
- 30. A 26-year-old primigravid woman at 25 weeks' gestation comes to the physician for a prenatal visit. She has no history of serious illness and her only medication is a daily prenatal vitamin. A 1-hour 50-g glucose challenge shows a glucose concentration of 167 mg/dL (N < 135). A 100-g oral glucose tolerance test shows glucose concentrations of 213 mg/dL (N < 180) and 165 mg/dL (N < 140) at 1 and 3 hours, respectively. If she does not receive adequate treatment for her condition, which of the following complications is her infant at greatest risk of developing? Restricted growth Elevated calcium levels Islet cell hyperplasia Decreased amniotic fluid production Omphalocele Decreased hematocrit SOAL Ambo