DL 16-AUB.pptx
- 2. SLO 1.Discuss about the definition, incidence, pathogenesis and PALM- COEIN classification of AUB. 2. Discuss the etiology, clinical features, investigations and treatment of puberty menorrhagia. 3. Discuss about the Metropathica hemorrhagica, irregular ripening and Halbanâs disease.
- 3. Objectives âĒ Normal uterine bleeding âĒ Common terminologies âĒ Classification âĒ Pathogenesis âĒ Investigation âĒ Management
- 4. Normal uterine bleeding âĒ Normal duration â 3-7 days âĒ Normal cycle frequency â 21- 35 days âĒ Normal amount â 30- 80ml âĒ Normal control of menstrual bleeding Menstrual bleeding- Platelet aggregation forms clot Prostaglandin F2alpha- myometrial contraction, constricts Endometrial vessels
- 5. Common terminologies âĒ Menorrhagia â Cyclical bleeding Excessive In amount or duration . Polymenorrhea â frequent cycles <21 days . Epimenorrhagia- frequent cycles + excessive bleeding . Metrorrhagia â intermenstrual bleeding . Oligomenorrhea- cycles frequency > 35days Hypomenorrhea- Scanty bleeding, cycle duration less than 2 days . Menometrorrhagia- Bleeding irregular and excessive
- 6. Abnormal uterine bleeding âĒ Excessive bleeding forom the uterus through the gental tract with palpable pelvic organ pathology or macroscopic / microscopic pathology.
- 7. Menorrhagia- causes âĒ Pelvic âĒ Fibroid uterus âĒ Adenomyosis âĒ Endometriosis âĒ IUCD in utero âĒ Chronic tubo ovarian mass âĒ Tubercular endometritis âĒ Retroverted uterus âĒ Granulosa cell tumour
- 8. ContinuedâĶâĶ âĒ Systemic Liver dysfunction . Congestive cardiac failure . Severe hypertension Endocrine hypothyroidism . Hyperthyroidism Hematological Idiopathic thrombocytopenic purpura . Leukemia . Von willebrand disease . Platelet deficiency
- 10. Polymenorrhea - causes âĒ Dysfunctional âduring adolescence âĒ - preceding menopause âĒ - following delivery and abortion âĒ Ovarian hyperemia âĒ PID and ovarian endometriosis
- 11. Metrorrhagia - causes âĒ Causes of acyclic bleeding âĒ DUB âĒ Submucous fibroid âĒ Uterine polyp âĒ Carcinoma cervix âĒ causes of contact bleeding âĒ Ca cervix âĒ Mucous polyp of cervix âĒ Vascular ectopy of cervix âĒ Cervicitis âĒ Cervical endometriosis
- 12. âĒ Causes of Intermenstrual bleeding âĒ Urethral caruncle âĒ Decubitus ulcer âĒ Breakthrough bleeding âĒ Iucd in utero âĒ Ovular bleeding
- 13. Oligomenorrhea âĒ Causes âĒ Age related â adolescence and menopause âĒ Obesity âĒ Stress related and exercise related âĒ Endocrine âPcos, hyperthyroidism, hyperprolactinemia âĒ Androgen producing tumours â ovarian , adrenal tumours âĒ Tubercular endometritis âĒ Drugs â phenothiazine, cimetidine, methyldopa
- 14. Hypomenorrhea âĒ Causes âĒ Uterine synechiae âĒ Tubercular endometritis- late cases âĒ Oral contraceptive âĒ Thyroid dysfunction âĒ Malnutrition
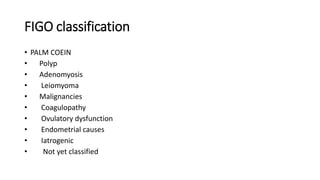
- 15. FIGO classification âĒ PALM COEIN âĒ Polyp âĒ Adenomyosis âĒ Leiomyoma âĒ Malignancies âĒ Coagulopathy âĒ Ovulatory dysfunction âĒ Endometrial causes âĒ Iatrogenic âĒ Not yet classified
- 18. Dysfunctional uterine bleeding âĒ Abnormal uterine bleeding without any palpable pelvic organ pathology either macroscopic or microscopic. âĒ Common during extremes of reproductive life, following pregnancy during lactation âĒ Immature hypothalamic pituitary ovarian axis- anovulatory cycle âĒ Types âĒ Anovulatory cycles- âĒ Ovulatory cycles
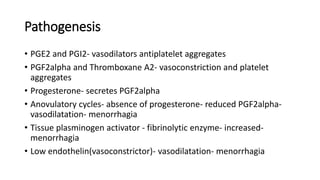
- 19. Pathogenesis âĒ PGE2 and PGI2- vasodilators antiplatelet aggregates âĒ PGF2alpha and Thromboxane A2- vasoconstriction and platelet aggregates âĒ Progesterone- secretes PGF2alpha âĒ Anovulatory cycles- absence of progesterone- reduced PGF2alpha- vasodilatation- menorrhagia âĒ Tissue plasminogen activator - fibrinolytic enzyme- increased- menorrhagia âĒ Low endothelin(vasoconstrictor)- vasodilatation- menorrhagia
- 20. Puberty menorrhagia âĒ Causes âĒ Hypothalamic pituitary ovarian dysfunction âĒ Blood dyscrasia- coagulation disorders, thrombocytopenic purpura, von willebrand disease, leukemia âĒ Hypothyroidism âĒ Genital tuberculosis âĒ Liver disorders âĒ Feminising ovarian tumour, adrenal hyperplasia
- 21. Clinical features âĒ Often Initial cycles regular âĒ Heavy regular cycles or âĒ Normal bleeding for several days âĒ Investigations âĒ Hb, bleeding time, clotting time, coagulation factors, blood film âĒ Xraychest - tb âĒ Thyroid function test âĒ Ultrasound âĒ D &C - tb endometrium
- 22. Management âĒ Treat cause, anemia âĒ Anovulatory cycles-acute - IV premarin 25mg 6-8hrly Estrogen for 21days Progesterone- for 10 days for 3-6cycles âĒ Chronic - oral combined pills or cyclical progesterone âĒ NSAIDs- mefenemic acid ,naproxen, ponstan, ibuprofen âĒ Mirena IUCD, Arterial embolisation, Uterine tamponade- foley catheter for 24hrs âĒ Anti tb treatment âĒ Iv tranexemic acid with oestrogen âĒ Desmopressin analogue of arginine vasopressin iv or nasal spray- von willebrand disease
- 23. Reproductive age âĒ Causes âĒ PALM COEIN classification âĒ PALM- structural abnormaties- studied by imaging and histopathological study âĒ COEIN- non structural- coagulation disorders and hormonal dysfunction
- 24. Investigation âĒ Ultrasound- polypus, adenomyosis, leiomyoma, malignancy âĒ Saline sonography- polypus âĒ Hysteroscopy- polypus âĒ Dilitaion and curettage âĒ Papsmear
- 25. Childbearing and premenopausal women âĒ Metropathia hemorrhagica âĒ Anovulatory AUB- 40-45years âĒ Continuous painless vaginal bleeding preceded by 6-8weeks of amenorrhoea âĒ Uterus slightly bulky âĒ Myohyperplasia- Uterine wall measurements upto 25mm âĒ Endometrium thick , polypoidal, thin slender polypi project into Uterine cavity âĒ Cystic glandular hyperplasia- Swiss cheese pattern
- 28. Investigation âĒ Hb, thyroid function test, coagulation profile âĒ Ultrasound âĒ Curettage, uterine aspiration, hysteroscopic biopsy âĒ Doppler ultrasound- endometrial vascularity âĒ Hysterosalpingography and saline salpingography
- 29. Treatment âĒ Correct anemia âĒ Treat the cause âĒ Combined oral contraceptives âĒ Progestogens âĒ Gestrinone âĒ Danazol âĒ GnRH analogues- 4weekly inj âĒ Tranexemic acid âĒ NSAIDs, ethamsylate , mirena iucd âĒ SERM- ormeloxifene, centchroman
- 30. Minimal invasive surgery âĒ Ablative techniques âĒ 1st generation- hysteroscopic ablation endometrium resectoscope, roller ball laser âĒ 2nd generation- radio frequency induced thermal ablation, balloon therapy, microwave ablation âĒ Uterine tamponade- âĒ Bilateral uterine artery embolisation âĒ If no response- hysterectomy
- 32. Thank you