Dr giolitto swiss endos 12.2004
- 1. Laparoscopic sacropexy: an approach to pelvic prolapse Jean Pierre Giolitto, M.D. Polyclinique les Bleuets REIMS - France SWISS-ENDOS December 2004
- 2. Introduction 1992’āĀ1996 strict reproduction of the technique by laparotomy. 1996’āĀ2000 innovative aspects new anatomic spaces endoscopic vision pneumo dissection 2000’āĀ2004 simplification of the technique reproducibility with acceptable operating time excellent results with anatomical correction and good functional results
- 3. Preoperative evaluation Evaluation of the prolapse degree of prolapse: uterus bladder rectum enterocele cystocele central: break of vesico vaginal fascia, vaginal rugae absent lateral: vaginal rugae present higher rectocele (fascia detachment) lower rectocele (deficient levator ani muscle)
- 4. Preoperative evaluation Evaluation of the (in)continence clinical examination urodynamic investigation ’āĀ prolapse plus pure SUI ’āĀ prolapse and hidden SUI ’āĀ prolapse without urinary problem Evaluation of the rectal dysfunction constipation fecal or gas incontinence Evaluation of the enterocele MRI
- 5. Preoperative evaluation Evaluation of the feasibility of laparoscopy ’ü« general anesthesia with pneumo peritoneum ’ü« Trendelenburg position ’ü« older and obese patients ’ü« the vaginal route will not be forgotten
- 6. Preoperative preparation Bowel preparation ’ü« empty the bowel and enlarge operating space ’ü« low residual diet 4-5 days prior to surgery ’ü« local enema one day before Vaginal oestrogens 3 or 4 weeks before Vaginal and parietal disinfection
- 7. Preoperative assessment ’ü» Clinical reexamination under general anesthesia search for new information which might modify the strategy ’ü» Morphology of the abdominal wall position of trocars ’ü« pubis ŌĆō umbilicus distance ’ü« first trocar ├ś 10mm: umbilical or supra umbilical ’ü« one 5 or 10mm trocar suprapubic on midline; at least 6cm between 1st and 2nd ’ü« two 5mm lateral trocars at level of anterior superior iliac spines
- 8. Preoperative assessment Exposition of the operating field ’ü« fixation of the uterus to the anterior abdominal wall ’ü« fixation of the bowel: sigmoid colon to the left abdominal wall Use a 5 or 6cm straight needle with a nylon suture
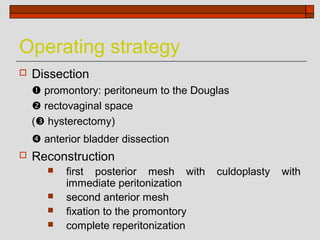
- 9. Operating strategy ’ü» Dissection ’üĄ promontory: peritoneum to the Douglas ’üČ rectovaginal space (’üĘ hysterectomy) ’üĖ anterior bladder dissection ’ü» Reconstruction ’ü« first posterior mesh with culdoplasty with immediate peritonization ’ü« second anterior mesh ’ü« fixation to the promontory ’ü« complete reperitonization
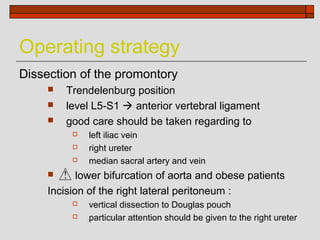
- 10. Operating strategy Dissection of the promontory ’ü« Trendelenburg position ’ü« level L5-S1 ’āĀ anterior vertebral ligament ’ü« good care should be taken regarding to ’ü» left iliac vein ’ü» right ureter ’ü» median sacral artery and vein ’ü« lower bifurcation of aorta and obese patients Incision of the right lateral peritoneum : ’ü» vertical dissection to Douglas pouch ’ü» particular attention should be given to the right ureter
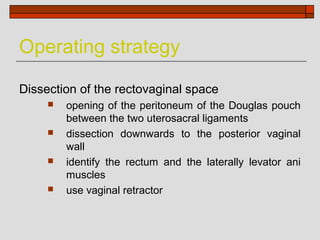
- 11. Operating strategy Dissection of the rectovaginal space ’ü« opening of the peritoneum of the Douglas pouch between the two uterosacral ligaments ’ü« dissection downwards to the posterior vaginal wall ’ü« identify the rectum and the laterally levator ani muscles ’ü« use vaginal retractor
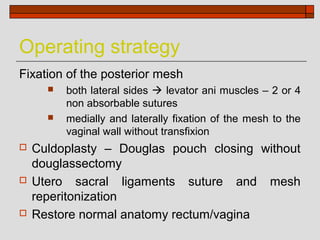
- 12. Operating strategy Fixation of the posterior mesh ’ü« both lateral sides ’āĀ levator ani muscles ŌĆō 2 or 4 non absorbable sutures ’ü« medially and laterally fixation of the mesh to the vaginal wall without transfixion ’ü» Culdoplasty ŌĆō Douglas pouch closing without douglassectomy ’ü» Utero sacral ligaments suture and mesh reperitonization ’ü» Restore normal anatomy rectum/vagina
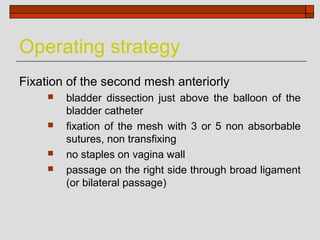
- 13. Operating strategy Fixation of the second mesh anteriorly ’ü« bladder dissection just above the balloon of the bladder catheter ’ü« fixation of the mesh with 3 or 5 non absorbable sutures, non transfixing ’ü« no staples on vagina wall ’ü« passage on the right side through broad ligament (or bilateral passage)
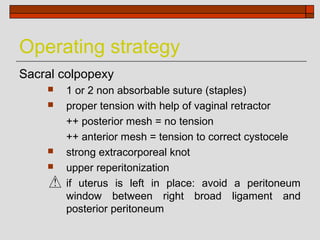
- 14. Operating strategy Sacral colpopexy ’ü« 1 or 2 non absorbable suture (staples) ’ü« proper tension with help of vaginal retractor ++ posterior mesh = no tension ++ anterior mesh = tension to correct cystocele ’ü« strong extracorporeal knot ’ü« upper reperitonization if uterus is left in place: avoid a peritoneum window between right broad ligament and posterior peritoneum
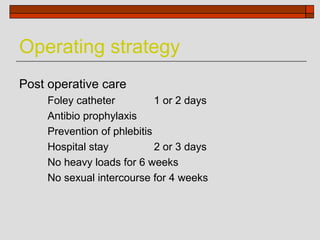
- 15. Operating strategy Post operative care Foley catheter 1 or 2 days Antibio prophylaxis Prevention of phlebitis Hospital stay 2 or 3 days No heavy loads for 6 weeks No sexual intercourse for 4 weeks
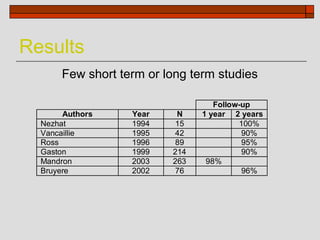
- 16. Results Few short term or long term studies Follow-up Authors Year N 1 year 2 years Nezhat 1994 15 100% Vancaillie 1995 42 90% Ross 1996 89 95% Gaston 1999 214 90% Mandron 2003 263 98% Bruyere 2002 76 96%
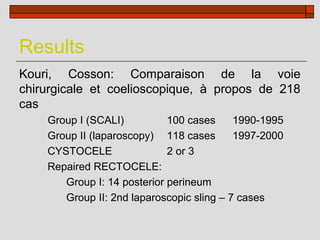
- 17. Results Kouri, Cosson: Comparaison de la voie chirurgicale et coelioscopique, ├Ā propos de 218 cas Group I (SCALI) 100 cases 1990-1995 Group II (laparoscopy) 118 cases 1997-2000 CYSTOCELE 2 or 3 Repaired RECTOCELE: Group I: 14 posterior perineum Group II: 2nd laparoscopic sling ŌĆō 7 cases
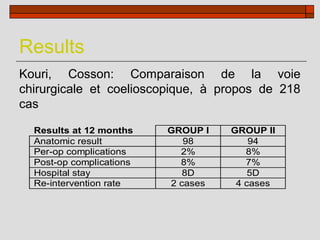
- 18. Results Kouri, Cosson: Comparaison de la voie chirurgicale et coelioscopique, ├Ā propos de 218 cas Results at 12 months GROUP I GROUP II Anatomic result 98 94 Per-op complications 2% 8% Post-op complications 8% 7% Hospital stay 8D 5D Re-intervention rate 2 cases 4 cases
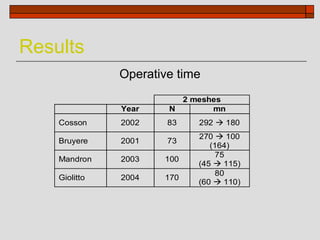
- 19. Results Operative time 2 meshes Year N mn Cosson 2002 83 292 ’āĀ 180 270 ’āĀ 100 Bruyere 2001 73 (164) 75 Mandron 2003 100 (45 ’āĀ 115) 80 Giolitto 2004 170 (60 ’āĀ 110)
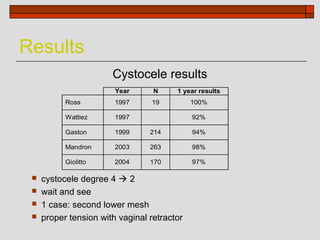
- 20. Results Cystocele results Year N 1 year results Ross 1997 19 100% Wattiez 1997 92% Gaston 1999 214 94% Mandron 2003 263 98% Giolitto 2004 170 97% ’ü« cystocele degree 4 ’āĀ 2 ’ü« wait and see ’ü« 1 case: second lower mesh ’ü« proper tension with vaginal retractor
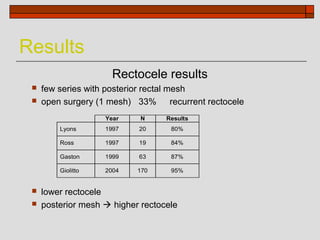
- 21. Results Rectocele results ’ü« few series with posterior rectal mesh ’ü« open surgery (1 mesh) 33% recurrent rectocele Year N Results Lyons 1997 20 80% Ross 1997 19 84% Gaston 1999 63 87% Giolitto 2004 170 95% ’ü« lower rectocele ’ü« posterior mesh ’āĀ higher rectocele
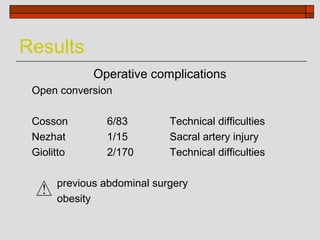
- 22. Results Operative complications Open conversion Cosson 6/83 Technical difficulties Nezhat 1/15 Sacral artery injury Giolitto 2/170 Technical difficulties previous abdominal surgery obesity
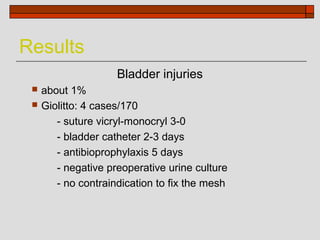
- 23. Results Bladder injuries ’ü« about 1% ’ü« Giolitto: 4 cases/170 - suture vicryl-monocryl 3-0 - bladder catheter 2-3 days - antibioprophylaxis 5 days - negative preoperative urine culture - no contraindication to fix the mesh
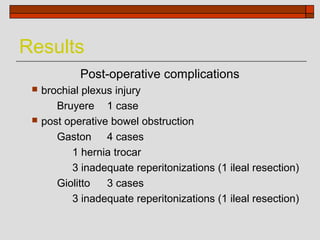
- 24. Results Post-operative complications ’ü« brochial plexus injury Bruyere 1 case ’ü« post operative bowel obstruction Gaston 4 cases 1 hernia trocar 3 inadequate reperitonizations (1 ileal resection) Giolitto 3 cases 3 inadequate reperitonizations (1 ileal resection)
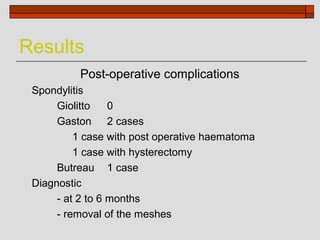
- 25. Results Post-operative complications Spondylitis Giolitto 0 Gaston 2 cases 1 case with post operative haematoma 1 case with hysterectomy Butreau 1 case Diagnostic - at 2 to 6 months - removal of the meshes
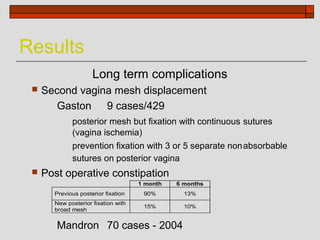
- 26. Results Long term complications ’ü« Second vagina mesh displacement Gaston 9 cases/429 posterior mesh but fixation with continuous sutures (vagina ischemia) prevention fixation with 3 or 5 separate nonabsorbable sutures on posterior vagina ’ü« Post operative constipation 1 month 6 months Previous posterior fixation 90% 13% New posterior fixation with 15% 10% broad mesh Mandron 70 cases - 2004
- 27. Conclusion Laparoscopy ’ü» advantage of the treatment by laparotomy ’ü» low morbidity such as the vaginal route ’ü» reproducibility of the technique ’ü» time: around 90 minutes ’ü» further studies required