EARLY NUTRITION
- 1. Early Nutritional Intervention and its Benefits for Stroke Patients Dimas Cortez, Breanna Schmidt, Cady Latshaw, & Jessie Sypinski
- 3. PICO QUESTION âą In acute stroke patients on a medical-surgical floor, what is the benefit of early nutritional screening and support on recovery after stroke? âą POPULATION: Acute stroke patients on a medical-surgical floor. âą INTERVENTION: Early nutritional screening and support. âą COMPARISION: Prolonging nutritional assessment. âą OUTCOME: Recovery after stroke.
- 4. LEARNING OBJECTIVES 1. The learner will develop a clear understanding of the impact of early nutritional screening on outcomes for patients after a stroke. 2. The learner will be able to identify stroke deficits that would hinder appropriate nutritional intake. 3. The learner will be able to recognize multiple feeding strategies in order to obtain optimal nutritional status in patients that suffered from a stroke. 4. The learner will be able to compare and contrast different nutritional assessment tools for the use of dysphagia screening.
- 5. DEFICITS THAT IMPAIR EATING âą Inability to maintain upright posture. âą Loss of upper extremity movement or sensation. âą Problems with chewing or swallowing. âą Communication deficits. âą Visual deficits. âą Depression. (Perry et al., 2012). www.health24.com
- 6. SIGNIFICANCE TO PRACTICE âą The reported frequency of malnutrition after stroke has varied from 8% to 34% (American Heart Association, 2003). âą Studies have shown that malnutrition increases the risk of several complications including infections, pressure ulcers, and gastrointestinal bleeding. It is also associated with lower functional ability and mortality (Mosselman et al., 2013). âą Although the effects of malnutrition are well-recognized, nutritional intervention is not considered a priority (Perry et al., 2012). âą Tools such as the Mini Nutritional Assessment (MNA) identified that malnutrition post-stroke ranged from 16% to 26% within the first week (Creasey, 2012). âą Post-stroke patients often suffer from a range of disabilities that effect nutritional intake, like postural, upper limb, and visual impairments (Nip et al., 2011).
- 7. CURRENT PRACTICE Literature âą There is a lack of standardization of assessment of nutritional status (American Heart Association, 2003). âą The screening of nutritional status and support is not a standard of practice depsite known complications for malnutrition (Mosselman, 2013) âą There is a lack of nutrition-related information in nursing literature (Mosselman, 2013). âą The nursing role in nutrition is often thought of mealtime management and enteral tube feedings (Perry et al., 2012). Good Samaritan âą During a stroke admission, there is no specific nutritional assessment done. âą The admitting nurse does a quick swallowing evaluation. âą Nutritional consults are only given automatically to patients presenting with low Braden scores. âą A full nutritional assessment is usually not done for several days post-admission.
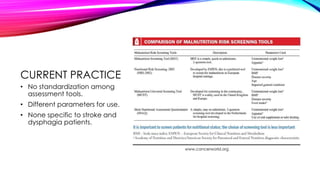
- 8. CURRENT PRACTICE âą No standardization among assessment tools. âą Different parameters for use. âą None specific to stroke and dysphagia patients. www.cancerworld.org
- 9. LITERATURE REVIEW âą Databases searched: EBSCO Health, Google Scholar, PubMed, Cochrane Library, Medline Plus. âą Keywords used: nutrition, stroke outcome, prognosis, acute cerebrovascular accident, malnutrition, dysphagia, nursing, feeding, eating, eating difficulties, outcomes, risk factors, early nutritional supplementation. âą Year limits: 2003- 2013. âą Other search limits used: clinical guidelines, systematic review, meta-analysis, randomized controlled trial. âą Number of articles reviewed: 12 articles reviewed.
- 10. SUMMARY OF EVIDENCE âą Early nutritional support can decrease morbidity and mortality, reduce complications, and reduce further risks and deterioration of patient (Wang et al., 2013). âą Early nutritional status is associated with long term outcomes (Garibella, 2003). âą There is an increased prevalence of dysphagia that is consistent among stroke patients (Martino et al., 2005). âą Nutritional supplementation decreased the prevalence of pressure sores in the majority amount of patients in a study that included over 6,000 patients (Geeganage, Beavan, Ellender, & Bath, 2012).
- 11. SUMMARY OF EVIDENCE âŠCONTINUED âą Nutritional Supplementation that started earlier rather than later revealed a lower end-of study fatality percentage (Geeganage, Beavan, Ellender, & Bath, 2012). âą Acute stroke patients nutritional needs should be the primary focus with a special focus on the delivery of protein (Creasey, 2012). âą A dietician consult should be implemented in order to provide adequate nutrition (Wirth et al., 2013).
- 12. CONSIDERATIONS FOR PRACTICE âą The use of behavioral interventions and acupuncture reduced dysphagia and pharyngeal electrical stimulation decreased pharyngeal transit time (Geeganage, Beavan, Ellender, & Bath, 2012). âą Women become more malnourished after experiencing a stroke compared to men (Medin et al., 2011). âą Stroke patients should have more supervision during mealtimes and assessments on food consumption should be utilized (Medin et al., 2011). âą Dysphagia should not be the only eating difficulty that is assessed in stroke patients. Stroke patients should also be assessed for arm movement, lip closure, and the ability to swallow (Westergren, 2006).
- 13. RECOMMENDATIONS FOR NURSING PRACTICE âą Early nutritional assessment and detection is recommended to ensure safe swallowing (Westergren, 2006). âą For patients requiring long-term nutritional support, PEG feeding results in decreased complications (Geeganage, 2012). âą Evaluating food consumption and how patients manage food on a plate would help decrease the prevalence of malnutrition (Medin et al., 2011). âą Early screening of malnutrition risks should be completed within the first 10 days of admission (Mosselman et al., 2013).
- 14. REFERENCES âą American Heart Association. (2003). Poor nutritional status on admission predicts poor outcomes after stroke: Observational data from the FOOD trial. Stroke, 34, 1450-1456. doi: 10.1161/01.S TR.0000074037.49197.8C âą Crary, M., Humphrey, J., Carnaby-Mann, G., Sambandam, R., Miller, L., & Silliman, S. (2009). Dysphagia, Nutrition, and Hydration in Ischemic Stroke Patients at Admission and Discharge from Acute Care. Dysphagia, 69-76. doi: 10.1007/s00455-012-9414-0 âą Creasey, L. (2012). Impact of nutrition practice on acute ischemic stroke outcome. Support Line, 34, 20-26. http://0- web.a.ebscohost.com.alvin.iii.com/ehost/detail/detail?vid=4&sid=5d239db9-2e7b-4542-af79- bb10155c48bc%40sessionmgr4001&hid=4106&bdata=JnNjb3BlPXNpdGU%3d#db=c8h&AN=2011513393 âą Geeganage, C., Beavan, J., Ellender, S., Bath, PMW. (2012). Interventions for dysphagia and nutritional support in acute and subacute stroke (Review). The Cochrane Collaboration, 10, 1-16. http://www.bibliotecacochrane.com/pdf/CD000323.pdf âą Martino, R., Foley, N., Bhogal, S., Diamant, N., Speechley, M., & Teasell, R. (2005). Dysphagia After Stroke: Incidence, Diagnosis, and Pulmonary Complications. Stroke,36, 2756-2763. doi: 10.1161/01.STR.0000190056.76543.eb âą Medin, J., Windahl, J., Magnus, A., Tham, K., Wredling, R. (2011). Eating difficulties among stroke patients in the acute state: A descriptive, cross-sectional, comparative study. Journal of Clinical Nursing, 20, 2563-2572. http://doi:10.1111/j.1365-2702.2011.03812.x
- 15. REFERENCES âąMosselman, M., Kruitwagen, C., Schuurmans, M., & Hafsteinsdottir, T. (2013). Malnutrition and risk of malnutrition in patients with stroke: Prevalence during hospital stay. Journal of Neuroscience Nursing, 194-204. doi: 10.1097/JNN.0b013e31829863cb âąNip, W. F. R., Perry, L., McLaren, S., & Mackenzie, A. (2011). Dietary intake, nutritional status and rehabilitation outcomes of stroke patients in hospital. Journal of Human Nutrition and Dietetics, 24, 460-469. http://doi:10.1111/j.1365- 277X.2011.01173.x âąPerry, L., Hamilton, S., Williams, J., & Jones, S. (2012). Nursing interventions for improving nutritional status and outcomes of stroke patients: Descriptive reviews of processes and outcomes. World views on Evidence-Based Nursing, 17-39. http://doi:10.1111/j.1741-6787.2012.00255.x âąWang, X., Dong, Y., Han, X., Qi, X., Huang, C., Hou, L., & Kline, A. (2013). Nutritional support for patients sustaining traumatic brain injury: A systematic review and meta-analysis of prospective studies. PLOS ONE, 8(3). Retrieved from www.plosone.org âąWestergren, A. (2006). Detection of eating difficulties after stroke: A systematic review. International Nursing Review, 53, 143-149. doi:10.1111/j.1365-2648.2008.04915.x âąWirth, R., Smoliner, C., JĂ€ger, M., Warnecke, T., Leischker, A., & Dziewas, R. (2013). Guideline clinical nutrition in patients with stroke. Experimental & Translational Stroke Medicine, 5(14), 14-14. doi:10.1186/2040-7378-5-14