ECTOPIC PREGNENCY.pptx ectopic pregnancy ppt
- 1. Ectopic Pregnancy and Emergencies in the First 20 Weeks of Pregnancy By Dr Kushiya Sri K
- 2. Approach to the childbearing women Brief history Initial Assessment (Primary Survey) ’éĘ Airway, Breathing, Circulation (ABCs): o Airway: Ensure the airway is patent o Breathing: Assess respiratory rate and oxygen saturation. Provide supplemental oxygen if needed o Circulation: Monitor heart rate, blood pressure, and signs of shock (e.g., tachycardia, hypotension, pallor) ’éĘ Assess for Hemodynamic Stability: o Unstable Patient: If the patient presents with signs of shock (e.g., hypotension, tachycardia, altered mental status), initiate immediate resuscitation (Airway securing) , Blood products and prepare for urgent surgical intervention. o Stable Patient: If the patient is hemodynamically stable, proceed with further evaluation and diagnostic workup
- 3. History ŌĆó Menstrual history ŌĆó Ask about previous pregnancy problems and miscarriages ŌĆó Discuss previous medical and surgical history and ask about substance abuse and smoking ŌĆó Ask about sexual activity and contraception ŌĆó Spontaneous abortion ŌĆó In a woman of childbearing age, hysterectomy with oophorectomy excludes ectopic pregnancy. ŌĆó In the situation of hysterectomy without oophorectomy, ectopic pregnancy is exceedingly rare. The theory is that a fistulous tract after hysterectomy enables embryo implantation in the tube or adnexa
- 4. ’éĘ Physical Examination: o Vital Signs: Check blood pressure, heart rate, respiratory rate, and temperature o Abdominal Exam: Assess for tenderness, rebound, or guarding, which may indicate peritoneal irritation o Pelvic Exam: ’é¦ Assess for cervical motion tenderness, adnexal tenderness or masses, and uterine size. Vaginal bleeding may also be noted
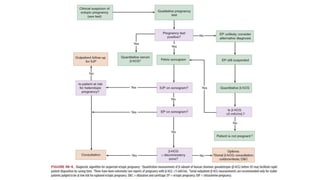
- 5. Diagnostic Evaluation ’éĘ Pregnancy Test: o Obtain a UPT or serum hCG (human chorionic gonadotropin) test to confirm pregnancy. ’éĘ Quantitative Serum hCG: o Measure the serum quantitative hCG level to help assess the viability and location of the pregnancy ’éĘ Transvaginal Ultrasound (TVUS): o Perform a transvaginal ultrasound to determine the location of the pregnancy. Key findings include: ’é¦ Intrauterine Pregnancy (IUP): Presence of a gestational sac within the uterus generally excludes ectopic pregnancy. ’é¦ Ectopic Pregnancy: Absence of an intrauterine pregnancy with a positive hCG level
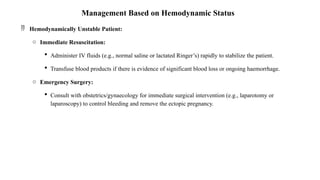
- 6. Management Based on Hemodynamic Status ’éĘ Hemodynamically Unstable Patient: o Immediate Resuscitation: ’é¦ Administer IV fluids (e.g., normal saline or lactated RingerŌĆÖs) rapidly to stabilize the patient. ’é¦ Transfuse blood products if there is evidence of significant blood loss or ongoing haemorrhage. o Emergency Surgery: ’é¦ Consult with obstetrics/gynaecology for immediate surgical intervention (e.g., laparotomy or laparoscopy) to control bleeding and remove the ectopic pregnancy.
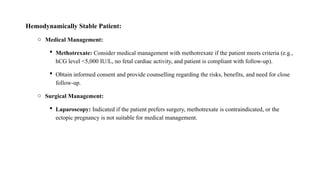
- 7. Hemodynamically Stable Patient: o Medical Management: ’é¦ Methotrexate: Consider medical management with methotrexate if the patient meets criteria (e.g., hCG level <5,000 IU/L, no fetal cardiac activity, and patient is compliant with follow-up). ’é¦ Obtain informed consent and provide counselling regarding the risks, benefits, and need for close follow-up. o Surgical Management: ’é¦ Laparoscopy: Indicated if the patient prefers surgery, methotrexate is contraindicated, or the ectopic pregnancy is not suitable for medical management.
- 8. Common obstetric-related conditions in the first 20 weeks of pregnancy ’āś Ectopic Pregnancy ’āś Spontaneous Abortion ’āś Septic Abortion ’āś Gestational Trophoblastic Disease ’āś Nausea And Vomiting Of Pregnancy
- 9. Ectopic Pregnancy Ectopic pregnancy occurs when a conceptus implants outside of the uterine cavity; ruptured ectopic pregnancies are a leading cause of maternal death in the first trimester of pregnancy Major Risk Factors for Ectopic Pregnancy ŌĆó Pelvic inflammatory disease, history of sexually transmitted infections ŌĆó History of tubal surgery or tubal sterilization ŌĆó Conception with intrauterine device in place ŌĆó Maternal age 35ŌĆō44 (age-related change in tubal function) ŌĆó Previous ectopic pregnancy ŌĆó Cigarette smoking (may alter embryo tubal transport)
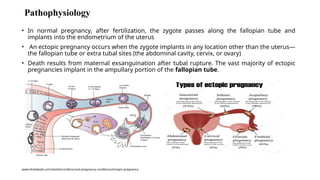
- 10. Pathophysiology ŌĆó In normal pregnancy, after fertilization, the zygote passes along the fallopian tube and implants into the endometrium of the uterus ŌĆó An ectopic pregnancy occurs when the zygote implants in any location other than the uterusŌĆö the fallopian tube or extra tubal sites (the abdominal cavity, cervix, or ovary) ŌĆó Death results from maternal exsanguination after tubal rupture. The vast majority of ectopic pregnancies implant in the ampullary portion of the fallopian tube. www.draliabadi.com/obstetrics/abnormal-pregnancy-conditions/ectopic-pregnancy
- 11. The underlying cause is most often damage to the tubal mucosa from ’āśPrevious infection ’āśPreventing transport of the ovum to the uterus ’āśTubal surgery ’āśDefects in the ovum resulting in premature implantation
- 12. Symptoms of Ectopic Pregnancy ŌĆó Sudden, sharp pain in the abdomen ŌĆó Abnormal bleeding. Either light spotting or heavy bleeding that occurs between periods. ŌĆó Feeling weak, dizzy, or faint. Blood loss due to internal bleeding can cause dizzy spells and fainting. ŌĆó Shoulder pain. When blood from a ruptured tube collects underneath the diaphragm, it can put pressure on the chest and shoulders, causing pain
- 13. Diagnosis : ŌĆó Serum ╬▓-hCG approximately doubles every 2 days early in a normal pregnancy and that longer doubling times indicate pathologic pregnancy ŌĆó Spontaneous abortion, hCG is expected to decrease by 21% to 35% in 2 days ŌĆó HCG levels that fail to increase by 53% or more in 2 days are suggestive but not diagnostic of ectopic pregnancy or an abnormal IUP. However, an increase of >53% does not rule out ectopic pregnancy additional testing should be performed
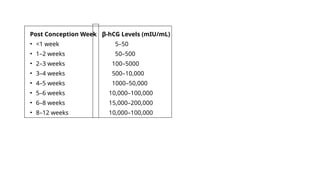
- 14. Post Conception Week ╬▓-hCG Levels (mIU/mL) ŌĆó <1 week 5ŌĆō50 ŌĆó 1ŌĆō2 weeks 50ŌĆō500 ŌĆó 2ŌĆō3 weeks 100ŌĆō5000 ŌĆó 3ŌĆō4 weeks 500ŌĆō10,000 ŌĆó 4ŌĆō5 weeks 1000ŌĆō50,000 ŌĆó 5ŌĆō6 weeks 10,000ŌĆō100,000 ŌĆó 6ŌĆō8 weeks 15,000ŌĆō200,000 ŌĆó 8ŌĆō12 weeks 10,000ŌĆō100,000
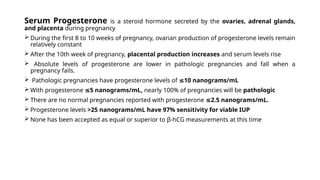
- 15. Serum Progesterone is a steroid hormone secreted by the ovaries, adrenal glands, and placenta during pregnancy ’āś During the first 8 to 10 weeks of pregnancy, ovarian production of progesterone levels remain relatively constant ’āś After the 10th week of pregnancy, placental production increases and serum levels rise ’āś Absolute levels of progesterone are lower in pathologic pregnancies and fall when a pregnancy fails. ’āś Pathologic pregnancies have progesterone levels of 10 nanograms/mL Ōēż ’āś With progesterone 5 nanograms/mL, Ōēż nearly 100% of pregnancies will be pathologic ’āś There are no normal pregnancies reported with progesterone 2.5 nanograms/mL. Ōēż ’āś Progesterone levels >25 nanograms/mL have 97% sensitivity for viable IUP ’āś None has been accepted as equal or superior to ╬▓-hCG measurements at this time
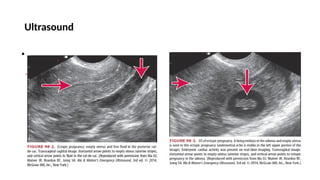
- 16. Ultrasound ŌĆó .
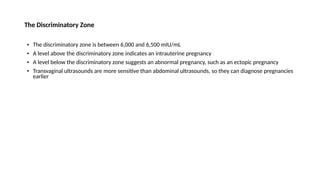
- 18. The Discriminatory Zone ŌĆó The discriminatory zone is between 6,000 and 6,500 mIU/mL ŌĆó A level above the discriminatory zone indicates an intrauterine pregnancy ŌĆó A level below the discriminatory zone suggests an abnormal pregnancy, such as an ectopic pregnancy ŌĆó Transvaginal ultrasounds are more sensitive than abdominal ultrasounds, so they can diagnose pregnancies earlier
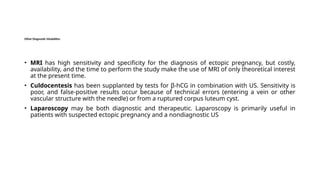
- 19. Other Diagnostic Modalities ŌĆó MRI has high sensitivity and specificity for the diagnosis of ectopic pregnancy, but costly, availability, and the time to perform the study make the use of MRI of only theoretical interest at the present time. ŌĆó Culdocentesis has been supplanted by tests for ╬▓-hCG in combination with US. Sensitivity is poor, and false-positive results occur because of technical errors (entering a vein or other vascular structure with the needle) or from a ruptured corpus luteum cyst. ŌĆó Laparoscopy may be both diagnostic and therapeutic. Laparoscopy is primarily useful in patients with suspected ectopic pregnancy and a nondiagnostic US
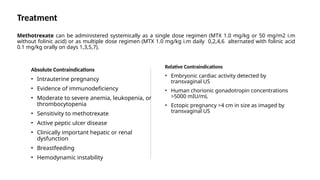
- 20. Treatment Methotrexate can be administered systemically as a single dose regimen (MTX 1.0 mg/kg or 50 mg/m2 i.m without folinic acid) or as multiple dose regimen (MTX 1.0 mg/kg i.m daily 0,2,4,6 alternated with folinic acid 0.1 mg/kg orally on days 1,3,5,7). Absolute Contraindications ŌĆó Intrauterine pregnancy ŌĆó Evidence of immunodeficiency ŌĆó Moderate to severe anemia, leukopenia, or thrombocytopenia ŌĆó Sensitivity to methotrexate ŌĆó Active peptic ulcer disease ŌĆó Clinically important hepatic or renal dysfunction ŌĆó Breastfeeding ŌĆó Hemodynamic instability Relative Contraindications ŌĆó Embryonic cardiac activity detected by transvaginal US ŌĆó Human chorionic gonadotropin concentrations >5000 mIU/mL ŌĆó Ectopic pregnancy >4 cm in size as imaged by transvaginal US
- 21. Surgical Management Laparoscopy: A minimally invasive procedure where small incisions are made in the abdomen to remove the ectopic pregnancy. Open surgery (laparotomy): A larger incision is made in the abdomen to directly access the fallopian tube or affected areas. Salpingostomy vs. Salpingectomy: Different surgical approaches to address the ectopic pregnancy.
- 22. SPONTANEOUS ABORTION The World Health Organization defines spontaneous abortion as loss of pregnancy before 20 weeks or loss of a fetus weighing <500 grams ŌĆó Other associations include advanced maternal age, prior poor obstetric history, concurrent medical disorders, previous abortion, infection ŌĆó Exposure to some agents, such as certain anesthetic agents, certain heavy metals, and tobacco, may also contribute to the incidence of abortion Diagnosis ŌĆó Obtain a quantitative serum ╬▓-hCG level, CBC to evaluate for blood loss, blood type, Rh factor and antibody screen, and urinalysis (urinary tract infection has been associated with increased fetal wastage) ŌĆó US can help rule out ectopic pregnancy, aid as a prognostic tool for fetal viability, and diagnose retained products of conception
- 23. Treatment ŌĆó Patients with a diagnosis of incomplete abortion should have the uterus evacuated ŌĆó The decision to proceed with medical treatment, such as PO misoprostol 600 micrograms ŌĆó If opted for surgical treatment such as dilatation and curettage should be made by an obstetrician ŌĆó Patients with a complete abortion, as shown by US and complete passage of products of conception and can be discharged safely with follow-up
- 24. Septic Abortion A septic abortion is a spontaneous or abortion complicated by a pelvic infection. ŌĆó Presenting complaints include fever, abdominal pain, vaginal discharge, vaginal bleeding, and history of recent pregnancy ŌĆó The most common causes are retained products of conception due to incomplete spontaneous or therapeutic abortion and introduction of either normal or pathologic vaginal bacteria by instrumentation. Diagnosis ’āś Obtain a quantitative serum ╬▓-hCG level, Routine Investigation ’āś A US will help identify retained products of conception in the uterus Treatment consists of fluid resuscitation, broad-spectrum IV antibiotics and early obstetric consultation for evacuation of the uterus Antibiotics, such as ampicillin/sulbactam, 3 grams IV or clindamycin 600 milligrams plus gentamicin 1 to 2 milligrams/kg IV
- 25. Gestational Trophoblastic Disease ’āś Gestational trophoblastic disease is a neoplasm that arises in the trophoblastic cells of the placenta ’āś Complete moles are more common in that is no actual fetus and in the partial mole a deformed nonviable fetus is present ’āś Patients with a history of hydatidiform molar pregnancy are at increased risk of future molar pregnancies , choriocarcinoma with cerebral metastases ’āś A risk of 1% in subsequent gestations after one molar pregnancy and a risk as high as 23% after two molar gestations Symptoms include vaginal bleeding in the first or second trimester (75% to 95% of cases), hyperemesis (26%) and Preeclampsia
- 26. ŌĆó When pregnancy-induced hypertension is seen before 24 weeks of gestation, consider the possibility of a molar pregnancy ŌĆó If trophoblastic disease is suspected because of abnormally high ╬▓-hCG levels ŌĆó Because not all molar pregnancies are found on US Treatment is by suction curettage in the hospital setting because of risk of hemorrhage ╬▓-hCG levels that fail to decrease after evaluation are evidence of persistent or invasive disease necessitating chemotherapy Metastasis to lung, liver, and brain may occur, but the prognosis for most patients is very good
- 27. Nausea and Vomiting of Pregnancy and Hyperemesis Gravidarum Nausea and vomiting of pregnancy is quite common with these symptoms reported in up to 90% of pregnancies Severe nausea and vomiting of pregnancy is known as hyperemesis gravidarum and is defined as vomiting with weight loss, volume depletion and laboratory values showing hypokalemia or ketonemia Findings on physical examination in nausea and vomiting of pregnancy are usually normal except for signs of volume depletion ŌĆó Laboratory tests to consider include CBC, serum electrolytes, BUN, creatinine, and urinalysis. The finding of ketonuria is important because it is an early sign of starvation
- 28. ŌĆó The presence of abdominal pain in nausea and vomiting of pregnancy or hyperemesis gravidarum is highly unusual and should suggest another diagnosis ŌĆó Cholelithiasis and cholecystitis are more common in pregnant women than in women of comparable age and health status who are not pregnant ŌĆó Differential diagnosis of vomiting or vomiting with abdominal pain should include cholecystitis, cholelithiasis, gastroenteritis, pancreatitis, appendicitis, hepatitis, peptic ulcer, pyelonephritis, ectopic pregnancy, fatty liver of pregnancy ŌĆó Treatment consists of IV fluids containing 5% glucose in either lactated RingerŌĆÖs solution or normal saline to replete volume and reverse ketonuria
- 30. THANK YOUŌĆ”..