Examination of lower cranial nervesCRANIAL NERVES (XI,XII)
- 1. WELCOME 1
- 2. NEUROANATOMY OF LOWER CRANIAL NERVES (XI,XII) Presented by Dr. Md. Tabriz Hossain Phase-A resident(Nephrology) Green unit, NINS 2
- 3. Development of Cranial nerves. The accessory nerve is derived from the basal plate of the embryonic spinal segments C1-C6. 3
- 4. A motor nerve formed by union of- -Cranial root -Spinal root. Cranial part: -formed from axons of nerve cells of nucleus ambiguous. -receives corticonuclear fibers from both cerebral hemisphere -efferent fibers emerge from anterior surface of medulla oblongata between the olive and inferior cerebellar peduncle. -nerve runs laterally in posterior cranial fossa - joins the spinal root Accessory Nerve 4
- 5. Spinal Part: ’üĮ Arises from nerve cells in the ventral horn of the C1-C5 segments of the spinal cord .Spinal nucleus receive corticospinal fiber from both cerebral hemisphere. ’üĮ The fibers form a nerve trunk that ascends alongside the spinal cord ’üĮ Enters the skull through the foramen magnum ’üĮ It then turns laterally & joins the cranial root. ’üĮ The two roots unite and leave the skull through the jugular foramen 5
- 6. Spinal root: ’üĮ Formed by fibers of spinal nucleus situated in anterior grey column of spinal cord in upper five cervical segments. 6
- 7. Exit the cranial fossa through jugular foramen (IX,X,XI) and through Hypoglossal canal(XII) 7
- 8. ’üĮ The roots then separate ’üĮ Cranial root joins the vagus nerve ’üĮ Distributed in its pharyngeal & laryngeal branches to the muscles of the soft palate, pharynx and larynx. 8
- 9. ’üĮ Course of spinal root: in neck ŌĆó Enters deep surface of sternocleidomastoid muscle which it supplies. ŌĆó Runs posteriorly & laterally crossing posteror triangle of neck. ŌĆó Passes beneath trapezius muscle which it supplies. 9
- 10. 10
- 11. The supranuclear connections act on the ipsilateral sternocleidomastoid and on the contralateral trapezius. 11
- 12. Function of XI nerve 12
- 15. 15
- 16. ’üĮ May be damaged by 1) Traumatic Injury 2) Tumours at the base of the skull 3) Fractures involving the Jugular foramen 4) Neck laceration Clinical Consideration: 16
- 17. ’üĮ Asymmetric neckline due to diminished trapezius muscle mass ’üĮ Ipsilateral weakness of sternocleidomastoid muscle causing weakness on turning the head against resistance away from the paralysed muscle. XI Nerve lesion 17
- 18. Damage to the accessory nerve (XI) may lead to weakness in the trapezius causingŌĆ” ’üĮ Downward & outward rotation of the upper part of the scapula, sagging of the shoulder ’üĮ Weakness on attempting to shrug the shoulder. ’üĮ Dropping of the shoulder ’üĮ Difficulty in elevating the arm above the horizontal level. XI Nerve lesion 18
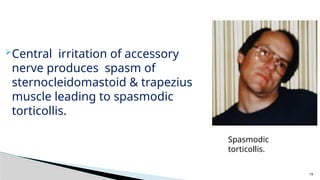
- 19. ’āśCentral irritation of accessory nerve produces spasm of sternocleidomastoid & trapezius muscle leading to spasmodic torticollis. Spasmodic torticollis. 19
- 20. HYPOGLOSSAL NERVE (CN 12) ŌĆōThe hypoglossal nerve is a motor nerve that supplies all the intrinsic muscles of the tongue as well as the styloglossus, the hyoglossus, and the genioglossus muscles. ŌĆōThe hypoglossal nucleus is situated close to the midline beneath the floor of the lower part of the forth ventricle. 20
- 21. ŌĆó It receives corticonuclear fibers from both cerebral hemisphere , however the cells responsible for supplying the genioglossus muscle only receive corticonuclear fibers from the opposite cerebral hemisphere. ŌĆó The hypoglossal nerve pass anteriorly through the medulla oblongata between the pyramid & the olive. 21
- 22. 22
- 23. Course ’āś The hypoglossal nerve crosses the posterior cranial fossa & leaves the skull through the hypoglossal canal. ’āś The nerve passes downward & forward in the neck between the internal caroti artery & the internal jugular vein until it reaches lower border of posterior bell of digastric. ’āś Here it turns forward, crosses internal & external carotid arteries, loop of the inguinal artery ’āś It passes deep to mylohyoid & on lateral surface of hyoglossus sends branches the muscles of the tongue. ’āś hypoglossal nerve is joined by C1 fibers from cervical plexus. 23
- 24. 24
- 25. Clinical testing(XII th cranial nerve) ’é¦ Ask to put out the tongue: in case of LMNL -Tongue deviates toward the paralyzed site. - Smaller, atrophy & fasciculation In case of lesion of corticonuclear fiber: - No atrophy or fibrillation of tongue - On protrusion, tongue will deviate to the side opposite the lesion. 25
- 26. 26
- 27. Clinical Consideration: ŌĆó lesion of hypoglossal nerve may occur anywhere along its course. Causes- -Tumor -Demyelinating disease -Syringobulbia -Vascular accidents -injury of nerve in the neck 27
- 28. Vernet syndrome ( jugular foramen syndrome): ’üĮ is a constellation of cranial nerve palsies due to a lesion at the jugular foramen such as a glomus jugulare tumour or schwannoma. ’üĮ It consists of motor paralysis of: ’üĮ Glossopharyngeal nerve (CN IX) ’üĮ Vagus nerve (CN X) ’üĮ Accessory nerve (CN XI) Lower Cranial Nerve Palsy 28
- 29. ’üĮ Pseudobulbar palsy: ’üĮ Lesion: Supranuclear lesion of the lower cranial nerves(IX,X,XI,XII) Lesion is bilateral and UMN type What causes the lesions ? Bilateral repeated CVA Involving Internal capsule Demyelinating disease(MS) Motor Neuron Disease ’üĮ Patient present withŌĆō Indistinct , slurred and high pitched speech (Donald Duck or Hot Potato Dysarthria) Tongue-small, stiff or spastic. Combined Lower Cranial Nerve Palsy 29
- 30. Bulbar palsy: ’é¦ Site of lesion: Nucleus of the lower cranial nerves (IX,X,XI,XII) in medulla ’é¦ Lesion is bilateral and LMN type ’é¦ Patient present with Dysarthria, Dysphonia, Dysphagia nasal regurgitation tongue-wasted,fasciculation Causes: Motor Neuron Disease (MND) GBS Syringobulbia Brainstem Infarction Poliomyelitis Neurosyphilis Neurosarcoid 30
- 31. Collet-Sicard syndrome: Unilateral lesions of cranial nerves IX, X, XI, and XII. CAUSES: ŌŚ” Tumours of the skull base, ŌŚ” Coiling and dissections of the internal carotid artery, ŌŚ” Multiple myeloma, ŌŚ” Vasculitis, ŌŚ” Carotid fibromuscular dysplasia, ŌŚ” Shotgun injuries, ŌŚ” Idiopathic cranial polyneuropathy, ŌŚ” Atlas fractures, ŌŚ” Occipital condyle fractures. 31
- 32. Villaret's syndrome: (retroparotid space syndrome, syndrome of retroparotid space) ’üĮ Combines ipsilatral paralysis of the last four cranial nerves (IX, X, XI, XII) and Horner syndrome . ’üĮ Sometimes cranial nerve VII also involved. ’üĮ It may also involve the cervical ganglia of the sympathetic trunk. ’üĮ Paralysis is caused by a lesion in the retroparotid space, 32
- 33. ’ü▒Glomus tumors (paragangliomas) are common causes of jugular foramen syndrome. ’ü▒ Benign, slow-growing head and neck tumors ’ü▒ Originates from the neural crest cells. ’ü▒ Commonly arise in the ŌĆó jugular bulb (glomus jugulare), ŌĆó middle ear (glomus tympanicum), ŌĆó nodose ganglion of the vagus nerve (glomus vagale) 33
- 34. Thank you 34